Parathyroid hormone or parathyroid hormone (PTH) is a protein formed in the parathyroid glands that is responsible for increasing the concentration of phosphate and Ca++ in the blood. The production and further transformation of the hormone depends on the calcium content. If its concentration decreases, more PTH is synthesized and released. When increasing, the reverse process is observed. Biologically active is whole (intact) parathyroid hormone 1-84 and 1-34, called the N-terminal fragment. The highest value occurs from 14 to 16 hours, by 8 am it decreases.
Functions of PTG:
- minimizing urinary excretion of calcium and increasing phosphorus;
- if there is a deficiency of these elements in the blood, the hormone promotes their extraction from the bones;
- When there is an excess of calcium in the blood, under the influence of parathyroid hormone, it is deposited in bone tissue.
Parathyroid hormone - what is it?
Parathyroid hormone is a hormone of the parathyroid glands
(it would be more correct to say “parathyroid glands”, but many patients are already very accustomed to the term “parathyroid glands”, although it is not entirely correct from the point of view of word formation).
Parathyroid hormone production
produced by parathyroid cells in response to a decrease in the level of ionized calcium in the blood. On the surface of the cells of the parathyroid glands there are special receptors that are able to assess the concentration of ionized calcium in the blood and, in accordance with its level, produce parathyroid hormone in larger or smaller quantities.
Very often the term “ parathyroid hormone”
"(parathyroid hormone - from parathyroid hormone) is written incorrectly, since it can be difficult for a non-specialist to hear all the features of the correct spelling.
Often on the Internet you can come across terms such as “ parad hormone
”, “
parade hormone
” and even “
parade of hormones
”. The correct term, of course, is one - parathyroid hormone (written together and without a hyphen).
Parathyroid hormone is a polypeptide hormone
(i.e. consisting of amino acids). There are 84 amino acid residues in the parathyroid hormone molecule. Currently, the structure of parathyroid hormone has been completely deciphered by scientists. It was found that in the parathyroid hormone molecule, the first 34 amino acid residues are responsible for the biological activity, and the rest are responsible for the binding of the hormone to receptors and the stability of the molecule as a whole.
The main effect of parathyroid hormone is to increase the level of ionized calcium
in blood. This action is realized through three different effects.
Firstly, parathyroid hormone enhances the activation of vitamin D in the kidneys
, which leads to the formation of an important hormone-like substance, calcitriol, from vitamin D. Calcitriol stimulates the absorption of calcium in the intestine, which leads to an increased flow of calcium from food into the blood. A prerequisite for the implementation of this effect of parathyroid hormone is the presence of a sufficient amount of vitamin D in the body. Without sufficient supply of vitamin D in the blood, parathyroid hormone is not able to enhance the absorption of calcium in the intestine.
Secondly, parathyroid hormone enhances the reabsorption of calcium ions from primary urine
. This effect is realized at the level of the renal tubules.
Thirdly, parathyroid hormone enhances the activity of osteoclasts
– cells that destroy bone tissue. Osteoclasts, like bulldozers or excavators, begin to actively destroy bone beams and release the resulting calcium into the blood. As a result, the concentration of calcium in the blood increases, but the strength of bone tissue decreases, which increases the likelihood of fractures.
Parathyroid hormone is a very interesting hormone, since the effect of parathyroid hormone on the bone directly depends on the mode of its production
. Everything that we said above about the negative effect of parathyroid hormone on bone tissue is true only for cases when parathyroid hormone is constantly and continuously elevated. At the same time, periodic and short-term release of parathyroid hormone into the blood has a positive effect on bone tissue, leading to increased formation of bone beams and bone strengthening. Now this effect is used in the treatment of osteoporosis - even a medicinal analogue of parathyroid hormone (teriparatide) has been synthesized, the periodic administration of which into the body can increase the strength of bone tissue and reduce the likelihood of fractures.
Parathyroid hormone (PTH) is a polypeptide hormone that is synthesized by the parathyroid glands and plays an important role in regulating calcium and phosphorus levels in the body.
Synonyms Russian
Parathyroid hormone, parathyrin, PTH.
English synonyms
Parathyroid hormone, intact PTH, parathormone, parathyrin.
Research method
Solid-phase chemiluminescent enzyme-linked immunosorbent assay (“sandwich” method).
Determination range: 1.2 - 5000 pg/ml.
Units
Pg/ml (picograms per milliliter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- During the day before the test, do not drink alcohol or take medications (as agreed with your doctor).
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress for 24 hours before the test.
- Do not smoke 3 hours before the test.
General information about the study
Parathyroid hormone (PTH) is produced by the parathyroid glands, located in pairs on the posterior surface of each lobe of the thyroid gland. Intact PTH (the whole hormone molecule) consists of 84 amino acids, has a short half-life (about four minutes) and is the main biologically active form of the hormone. Its N- and C-terminal fragments have a longer lifespan, and their activity and metabolism are being studied.
PTH plays an important role in the regulation of phosphorus-calcium metabolism and ensures the maintenance of stable concentrations of calcium and phosphorus in the extracellular fluid. The level of PTH is closely related to the amount of calcium, vitamin D, phosphorus, calcium, magnesium in the body; the regulation of its secretion is carried out according to the feedback principle. When the concentration of calcium in the blood decreases (hypocalcemia), the release of PTH by the parathyroid glands increases, and when it increases (hypercalcemia), on the contrary, it decreases. These mechanisms are aimed at maintaining a stable level of calcium in the blood. An increase in PTH promotes the activation of osteoclasts, bone resorption and the release of calcium from bones, enhances the absorption of calcium from the intestine, delays the excretion of calcium by the kidneys and inhibits the reverse reabsorption of phosphorus. The PTH antagonist is the hormone calcitonin, secreted by the C cells of the thyroid gland. Normally, when the normal concentration of calcium in the blood is reached, PTH production decreases.
With pathology and excessive synthesis of PTH (hyperparathyroidism), hypercalcemia, hyperphosphaturia, generalized osteoporosis, vascular calcification, and damage to the gastrointestinal mucosa develop. Insufficient secretion of PTH (hypoparathyroidism) is accompanied by hypocalcemia and hyperphosphatemia and can lead to convulsions and tetany.
It is important to simultaneously assess the level of free, or ionized, calcium in the blood and PTH, taking into account clinical manifestations and the results of other laboratory and instrumental studies, this allows for differential diagnosis of very similar pathological conditions and development of the correct treatment tactics.
What is the research used for?
- To assess the function of the parathyroid glands.
- To find out the causes of hypo- or hypercalcemia, calcium metabolism disorders.
- For differential diagnosis of primary, secondary and tertiary hyperparathyroidism.
- For the diagnosis of hypoparathyroidism.
- For monitoring patients with chronic calcium metabolism disorders.
- To evaluate the effectiveness of treatment of pathology of the parathyroid glands and their surgical removal for neoplasms.
When is the study scheduled?
- When the level of calcium in the blood changes (hyper- or hypocalcemia).
- For symptoms of hypercalcemia (fatigue, nausea, abdominal pain, thirst) or hypocalcemia (abdominal pain, muscle cramps, tingling fingers).
- When the size and structure of the parathyroid glands change according to instrumental methods (for example, CT).
- In the treatment of calcium metabolism disorders.
- For neoplasms of the parathyroid glands, as well as immediately after their surgical removal.
- For osteoporosis and changes in bone structure.
- For chronic kidney disease and reduced glomerular filtration rate.
What do the results mean?
Reference values: 15 - 65 pg/ml.
A normal level of PTH with low calcium in the blood is a sign of hypoparathyroidism (insufficient synthesis of PTH by the parathyroid glands). High PTH and elevated blood calcium concentration indicate hyperparathyroidism. The PTH level is assessed together with the blood calcium level.
Causes of increased parathyroid hormone levels
- Hypocalcemia (with normal function of the parathyroid glands, the level of PTH increases in order to mobilize calcium from the depot and increase its absorption).
- Primary hyperparathyroidism (accompanied by increased levels of calcium and calcitonin, the level of phosphorus in the blood is normal or reduced):
- hyperplasia of the parathyroid glands,
- adenoma or cancer of the parathyroid glands.
- chronic renal failure,
- vitamin D and calcium deficiency,
- malabsorption syndrome.
Causes of decreased parathyroid hormone levels
- Hypercalcemia (a decrease in PTH with normal function of the parathyroid glands contributes to a decrease in the concentration of calcium in the blood).
- Primary hypoparathyroidism (insufficient function of the parathyroid glands).
- Secondary hypoparathyroidism (for example, a complication of surgical treatment of thyroid diseases, a condition after removal of the parathyroid glands).
- Excess vitamins A and D.
- Idiopathic hypercalcemia.
- Autoimmune diseases with the formation of autoantibodies to calcium receptors.
- Wilson-Konovalov disease, hemochromatosis.
- Graves' disease, severe thyrotoxicosis.
- Magnesium deficiency.
- Multiple myeloma.
- Sarcoidosis.
What can influence the result?
- Drinking milk before the test may result in low PTH readings.
- An increase in PTH is observed during pregnancy and lactation.
- A false decrease in PTH is observed in milk-alkali syndrome (Burnett's disease).
- The administration of radioisotope drugs a week before the test distorts the test result.
- Medicines that increase PTH levels in the blood: phosphates, diuretics, lithium, rifampicin, furosemide, isoniazid, steroids, thiazide or anticonvulsants.
- Cimetidine and propanodol reduce PTH levels.
- PTH levels are subject to circadian rhythms and normally vary throughout the day, reaching a maximum at 2-4 p.m. and a basal value at 8 a.m.
Parathyroid hormone production
The production of parathyroid hormone is regulated by the level of ionized calcium
in blood. If calcium in the blood decreases, parathyroid hormone begins to be released more actively.
On the surface of the cells of the parathyroid glands there is a calcium-binding receptor, which is directly able to “sense” the concentration of calcium in the blood and regulate the rate at which parathyroid hormone is produced. This is the only receptor currently known to science that is “controlled” not by peptides or hormones, but by the substance itself—or rather, by its ions. Be that as it may, parathyroid hormone is normally produced by the parathyroid glands only when the concentration of calcium in the blood decreases.
Methods for correcting parathyroid hormone levels
If there are deviations of PTH from the norm to a greater or lesser extent, treatment is necessary. This is usually hormone replacement therapy. Thus, if the secretion of parathyroid hormones is insufficient, a complex of hormone-containing drugs is prescribed to correct their levels. The course can last several months, or you have to take the pills for life. It depends on the cause of the failure and the effectiveness of treatment procedures.
If parathyroid hormone is produced in excess, the disorder is corrected by eliminating the root cause (treatment of diseases that provoked hyperproduction of hormones). In some cases, partial or complete resection of the parathyroid gland is performed. If malignant tumors are present, the glands are removed.
Parathyroid hormone and calcium
There are two “friends” in the body, two substances that are inextricably linked - parathyroid hormone, calcium
.
At the same time, there is a relationship between them, which in endocrinology is described as “double feedback”. They sort of regulate each other. When the level of calcium in the blood decreases, parathyroid hormone begins to be released more, as a result of which calcium in the blood increases and acts on the cells of the parathyroid glands through the receptor, causing them to stop releasing parathyroid hormone. After the release of parathyroid hormone ceases, calcium begins to gradually decrease until it reaches a level at which the cells of the parathyroid glands are activated with the release of parathyroid hormone - and the cycle repeats. Calcium is the main thing that parathyroid hormone influences, and at the same time parathyroid hormone is one of the most important substances that calcium influences
.
Parathyroid hormone and calcitonin
Unlike substances such as calcium, parathyroid hormone and calcitonin are “enemies”, antagonists
.
Parathyroid hormone is aimed at increasing the level of calcium in the blood, and calcitonin is aimed at reducing it. Parathyroid hormone stimulates the destruction of bone beams with a prolonged increase, and calcitonin, on the contrary, causes the formation of new bone tissue and thereby strengthens the bone. The relationships between hormones, if you dig deep, are even deeper - for example, in some hereditary syndromes (multiple endocrine neoplasia syndrome, MEN), tumors simultaneously develop that produce both hormones - parathyroid hormone, calcitonin. Therefore, when examining for elevated parathyroid hormone, calcitonin is required
.
Vitamin D and parathyroid hormone
Vitamin D and parathyroid hormone are substances whose effects are similar and largely depend on each other. Both substances - vitamin D and parathyroid hormone - their main effect is to increase blood calcium levels
. As is the case with calcium, parathyroid hormone and vitamin D can influence each other. This effect is very interesting and is implemented in general terms like this. When the level of calcium in the blood decreases, the cells of the parathyroid glands begin to actively produce parathyroid hormone, which enhances the hydroxylation of vitamin D in the kidneys and the formation of calcitriol, the active form of vitamin D, which, due to the strength of its action, can be confidently recognized as a hormone. Calcitriol, on the one hand, enhances the release of a special transport protein in the intestinal wall - calmodulin, which “drags” calcium from the intestinal lumen into the blood, and on the other hand, it directly acts on a special receptor on the surface of the cells of the parathyroid glands (it is called the vitamin receptor D or VDR, vitamin D receptor). Activation of the vitamin D receptor leads to suppression of the proliferation of parathyroid gland cells, i.e. indirectly acts to reduce parathyroid hormone levels.
It is important to understand that a decrease in the intake of vitamin D into the human body leads to a “disinhibition” of the division of cells of the parathyroid glands and at the same time to stimulation of the production of parathyroid hormone by these cells. This occurs when there is little sun exposure to the skin, since vitamin D is produced in human skin. The second cause of vitamin D deficiency is insufficient intake of vitamin D from food. Low vitamin D in the blood leads to a low intake of calcium into the blood, which activates the production of parathyroid hormone by the cells of the parathyroid glands.
Vitamin D deficiency has been proven to increase the incidence of benign tumors
– adenomas of the parathyroid glands (probably due to the elimination of the inhibitory effect of vitamin D on the division of cells of the parathyroid glands due to its deficiency).
The second common situation with which patients come to the North-Western Endocrinology Center is the so-called secondary hyperparathyroidism, i.e. a condition in which parathyroid hormone is elevated in the blood, but calcium is normal
. The detection of normal or reduced calcium simultaneously with an increase in parathyroid hormone levels usually indicates a low level of vitamin D in the blood. You can, of course, conduct a blood test for vitamin D, but you can do it differently - prescribe vitamin D and calcium supplements to the patient, and after 1-2 months, repeat the blood test for parathyroid hormone and ionized calcium. If a repeated analysis reveals a decrease or normalization of parathyroid hormone, and the calcium level is normal, this will indicate with a high degree of certainty that the patient simply needs to take calcium and vitamin D supplements longer. If a repeated blood test shows that parathyroid hormone is is still high, and calcium has increased above normal - this will indicate that the patient has primary hyperparathyroidism, a tumor of the parathyroid gland.
References
1. Kiseleva, N.G. Diagnosis of osteoporosis in childhood. // N.G. Kiseleva, T.E. Taranushenko, N.K. Golubenko. – Medical Council, 2021. – pp. 186-193. 2. Lysenko, I.M. Diseases of the parathyroid glands. Hyperparathyroidism and hypoparathyroidism. – Protection of motherhood and childhood, 2012. – pp. 60-67. 3. Leder, B. Parathyroid hormone and parathyroid hormone-related protein analogs in osteoporosis therapy. Current osteoporosis reports, 2021. – Vol.15(2). – P.110-119. Doi: 10.1007/s11914-017-0353-4. 4. Clinical recommendations “Primary hyperparathyroidism” / approved. Ministry of Health of the Russian Federation, 2021. – URL: https://www.endocrincentr.ru/sites/default/files/specialists/science/clinic-recomendations/kr88.pdf.
Blood test for parathyroid hormone
Analysis for parathyroid hormone
is one of the most important in the list of examinations prescribed for suspected calcium metabolism disorders, including the development of osteoporosis.
Blood for parathyroid hormone is usually donated simultaneously with an analysis for ionized calcium, phosphorus, calcitonin
, since such a block of studies allows the endocrinologist to most fully assess the metabolic state. It is also highly advisable to immediately perform densitometry - a study of bone tissue density, which shows the likelihood of developing bone fractures.
Parathyroid hormone - analysis
, the quality of which varies greatly between different laboratories. Currently, the most common methods of performing a blood test for parathyroid hormone are enzyme immunoassay (the so-called 2nd generation method) and immunochemiluminescence (3rd generation method).
Most laboratories analyze parathyroid hormone using a 2nd generation method
, since equipment and reagents for enzyme-linked immunosorbent assay (ELISA) are inexpensive, you can even use domestically produced reagents. At the same time, the use of the ELISA method leads to a decrease in the accuracy of the analysis of parathyroid hormone in the blood and an increase in error.
The specialized laboratory of the North-Western Center for Endocrinology uses a 3rd generation automatic immunochemiluminescent analyzer DiaSorin Liaison XL (Italy) to perform analysis for parathyroid hormone.
– a device with exceptionally high analytical accuracy. In the work of endocrinologists at our center, the accuracy of a test such as a blood test for parathyroid hormone is the main diagnostic component, so we take issues of research quality very seriously. The specialized laboratory of the center NEVER performs parathyroid hormone analysis using the 2nd generation method and NEVER uses either domestic or Chinese reagents - only reagents made in Italy by the DiaSorin company.
If you are deciding where to donate parathyroid hormone
, and are not sure what tests should be taken additionally -
do the following blood test: parathyroid hormone and calcium (ionized is very desirable), phosphorus, calcitonin
. If you also donate your daily urine test for calcium, that will be simply wonderful; any endocrinologist will appreciate your erudition in matters of taking tests.
In the laboratory of the Endocrinology Center, the analysis for ionized calcium is carried out using an automatic biochemical analyzer Olympus AU-680 (Japan) - a high-performance, high-precision automatic machine capable of conducting up to 680 biochemical tests per hour! Combined with the high accuracy of parathyroid hormone and calcitonin tests, an accurate calcium test will provide optimal diagnostic results.
Parathyroid hormone and anemia
Anemia is a common complication of chronic kidney disease. There are various causes of renal anemia, such as decreased erythropoietin production, erythropoietin (EPO) resistance, decreased red blood cell survival, and bone marrow fibrosis, thereby decreasing hematopoiesis. Secondary hyperparathyroidism (SHPT) is a lesser known but potentially significant cause of renal anemia in patients with chronic kidney disease. Parathyroid hormone (PTH) is considered a uremic toxin that has many side effects, and elevated levels are associated with renal anemia in hemodialysis patients. Moreover, clinical studies have shown that treatment of SHPT with vitamin D receptor activators, calcimimetics, or parathyroidectomy results in improvement of anemia, supporting the role of parathyroid hormone in renal anemia. New evidence also implicates bone-derived fibroblast growth factor 23 in renal anemia. Patients with a poor response to EPO had a higher percentage of osteoclastic and eroded bone surface and a higher degree of bone marrow fibrosis combined with higher PTH levels compared with patients with a good response to erythropoietin. This finding indicates that the severity of SHPT and the degree of bone marrow fibrosis increase the dose of EPO required to achieve an adequate hematocrit response.
Evidence from several studies suggests that high levels of parathyroid hormone suppress endogenous erythropoietin synthesis and thereby contribute to renal anemia, although the molecular mechanisms by which PTH negatively regulates EPO synthesis are largely unknown. An early study by Meytes et al. showed that PTH at concentrations comparable to those found in the blood of uremic patients causes a marked inhibition of murine bone marrow forming unit erythroid (BFU-E) bursting, and increasing EPO concentrations overcome this effect of PTH.
The effect of PTH on the osmotic fragility of red blood cells was studied by Bogin et al. They demonstrated that PTH increases the osmotic fragility of red blood cells due to increased calcium entry into the red blood cells. A follow-up study by Akmal et al. further showed that 51 Cr-labeled RBC survival was reduced in 5/6 nephrectomy dogs, but reduced RBC survival was normalized in parathyroidectomized uremic dogs. These data suggest that PTH is one of the factors responsible for the reduction in red cell survival in renal failure. Coe et al. showed that FGF23 negatively regulates erythropoiesis by suppressing EPO production and EPO receptor expression. One study demonstrated that FGF23 directly targets hepatocytes to cause inflammation. Since chronic inflammation is a common cause of anemia, FGF23-induced inflammation may also contribute to renal anemia and hyporesponsiveness to EPO. In support of these experimental findings, a recent report from the Chronic Renal Insufficiency Cohort Study (CRIC) demonstrated a significant association of elevated FGF23 levels with widespread anemia, changes in hemoglobin over time, and the development of anemia. Gaweda et al. reported a modest but significant association between increased PTH levels and decreased erythropoietic response.
Parathyroidectomy (PTx) is the most radical treatment for SHPT, and early studies focused on the effect of PTx on EPO doses or hemoglobin levels to examine the role of PTH in renal anemia. One of the most representative studies was conducted by Trunzo et al. The researchers analyzed data from 37 patients who underwent PTx for severe SHPT and found that PTx resulted in a significant reduction in EPO doses with an increase in hemoglobin levels. Similar results have been reported by several independent groups, and these highly consistent results may indicate a significant beneficial effect of PTx on renal anemia.
The calcimimetic Cinacalcet hydrochloride is the latest option for the treatment of SHPT. This agent allosterically modulates the parathyroid calcium-sensing receptor (CaSR) and increases its sensitivity to extracellular calcium, thereby reducing PTH synthesis and secretion. Since the introduction of cinacalcet, several small studies have examined the effect of cinacalcet on renal anemia. These studies reported increased hemoglobin levels or decreased doses of erythropoiesis-stimulating agents (ESAs) following the use of cinacalcet for SHPT. The researchers found that each additional 6-month period of cinacalcet was associated with a 1.1-fold increase in the likelihood of achieving target hemoglobin levels.
There are several possible mechanisms by which cinacalcet may improve renal anemia. The most plausible mechanism is that lowering PTH levels with cinacalcet attenuates the multiple inhibitory effects of PTH on erythropoiesis. Additionally, since cinacalcet also inhibits FGF23 secretion, cinacalcet-induced reduction in FGF23 levels may help improve renal anemia. In addition, it should be noted that CaSR is also expressed in hematopoietic stem cells and has the function of keeping these cells in close physical proximity to the endosteal surface of the bone marrow and components of the regulatory niche. Thus, it is possible that the allosteric effect of cinacalcet on CaSR improves the placement of hematopoietic stem cells in the endosteal niche and thereby facilitates erythropoiesis.
Treatment with vitamin D supplementation agents (VDRAs), such as calcitriol and maxacalcitol, has long been the main treatment strategy for SHPT. A non-randomized study examined the effect of VDRAs on renal anemia and demonstrated reduced EPO doses or improved hemoglobin levels among patients receiving VDRAs. The most likely mechanism of action of VDRA is a decrease in PTH levels, but accumulating evidence suggests potential health benefits of vitamin D beyond suppression of PTH secretion. Indeed, several observational studies have shown an independent association between lower 25-hydroxyvitamin D (25[OH]D) levels and lower hemoglobin concentrations in populations with chronic kidney disease. In this context, some researchers hypothesize that such pleiotropic effects of vitamin D require local production of 1,25(OH)2D by extrarenal 1α-hydroxylase, and thus dietary vitamin D may enhance erythropoiesis. To test this hypothesis, Miskulin et al. recently conducted a randomized clinical trial in hemodialysis patients with vitamin D deficiency or insufficiency. The researchers demonstrated that 6 months of ergocalciferol supplementation increased serum 25(OH)D levels but had no effect on EPO dose. These data indicate that vitamin D has no role in the treatment of anemia in hemodialysis patients. However, it remains unknown whether systemically administered VDRAs directly affect erythropoiesis independent of the effect on PTH.
Literature
Akmal M, Telfer N, Ansari AN, Massry SG. Erythrocyte survival in chronic renal failure. Role of secondary hyperparathyroidism. J Clin Invest 1985; 76:1695–8.
Coe LM, Madathil SV, Casu C, Lanske B, Rivella S, Sitara D. FGF-23 is a negative regulator of prenatal and postnatal erythropoiesis. J Biol Chem 2014; 289:9795–810.
Singh S, Grabner A, Yanucil C et al. Fibroblast growth factor 23 directly targets hepatocytes to promote inflammation in chronic kidney disease. Kidney Int 2016; 90: 985–96
Mehta R, Cai X, Hodakowski A, Lee J, Leonard M, Ricardo A, Chen J, Hamm L, Sondheimer J, Dobre M, David V, Yang W, Go A, Kusek JW, Feldman H, Wolf M, Isakova T , CRIC Study Investigators. Fibroblast growth factor 23 and anemia in the chronic renal insufficiency cohort study. Clin J Am Soc Nephrol 2017; 12: 1795–1803
Dunn CDR, Trent D. The effect of parathyroid hormone on erythropoiesis in serum free cultures of fetal mouse liver cells. Proc Soc Exp Biol Med 1981; 166:556–61.
Miskulin D, Majchrzak K, Tighiouart H et al. Ergocalciferol supplementation in hemodialysis patients with vitamin D deficiency: a randomized clinical trial. J Am Soc Nephrol 2015; 27: 1801–10.
Meytes D, Bofin E, Ma A, Dukes PP, Massry SG. The effect of parathyroid hormone on erythropoiesis. J Clin Invest 1981; 67:1263–9
Trunso J., et al. Effect of parathroidectomy on anemia and erythropoietin dosing in end‐stage renal disease patients with hyperparathyroidism. Surgery 2008; 144:915–8. (2008)
Where to get parathyroid hormone
The specialized laboratory of the North-Western Endocrinology Center takes tests for parathyroid hormone and calcium, phosphorus and calcitonin
, as well as receiving other analyzes (more than 1000 studies) at the following addresses in St. Petersburg and Vyborg:
— Petrograd branch of the endocrinology center
– center of St. Petersburg, 200 meters to the left on foot from the Gorkovskaya metro station, Kronverksky Prospekt, building 31. Branch opening hours: 7.30-20.00, seven days a week. Phone: 498-10-30. There is parking for cars.
— Primorsky branch of the endocrinology center
– Primorsky district of St. Petersburg, 250 meters to the right from the Begovaya metro station. Branch address: st. Savushkina, house 124, building 1. Branch opening hours: 7.00-20.00, seven days a week. Phone: 565-11-12. There is parking for cars.
— Vyborg branches of the Endocrinology Center:
- Vyborg, st. Gagarina, 27A, tel., from 7.30 to 20.00, seven days a week. There is parking available for cars.;
- Vyborg, Pobedy Ave., 27A, tel. (81378) 36-306, from 7.30 to 20.00, seven days a week. There is parking for cars.
The branches of the endocrinology center provide everything for the comfort of patients who came to take parathyroid hormone, calcium and other tests
– no queues, comfortable treatment rooms with comfortable chairs and cartoons for a positive attitude, air conditioning and deep air purification systems, modern vacuum blood collection systems.
You can receive the results of a blood test for parathyroid hormone and other indicators by email
immediately after they are completed. In the vast majority of cases, tests are performed within 1 day (often the test for parathyroid hormone and calcium is ready in the evening of the day the patient came for the test).
You can find a complete list of laboratory branches in the Leningrad region (the cities of Luga, Gatchina, Kingisepp, Svetogorsk) here.
If you are not yet sure where to take parathyroid hormone in St. Petersburg or the Leningrad region
– contact the Northwestern Endocrinology Center. You will be confident in the quality of the research and conduct it with comfort. It is important that in the same center you can get a consultation with an endocrinologist who has significant experience in treating disorders of parathyroid hormone production.
Parathyroid hormone is normal
When you donate blood in a specialized modern laboratory and receive the result of a test for parathyroid hormone, the norm is indicated on the laboratory form
immediately after your individual result.
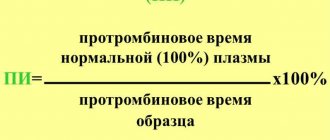
Parathyroid hormone levels can be expressed in two different units of measurement - pg/ml and pmol/l. Recalculation between them is possible using the following formula:
parathyroid hormone level in pmol/l x 9.8 = parathyroid hormone level in pg/ml
Parathyroid hormone is normal
, when it fits within the boundaries specified as reference limits (standards).
This indicator is not dependent on gender - if you take a parathyroid hormone test, the norm for women will not differ from the norm for men
.
Parathyroid hormone during pregnancy
Pregnant women should periodically donate blood to determine PTH levels, as the risk of abnormalities increases. Monitoring the hormone will allow timely detection of disorders and prevent the development of abnormalities in the fetus.
As a rule, pregnant women experience a slight decrease in parathyroid hormone, which is associated with a decrease in albumin concentration. This occurs due to the active production of vitamin D by the placenta, which activates the absorption of calcium by the intestinal walls (hypercalciuria). If too much of it is produced, muscle cramps (tetany) appear, so women in this position often have “cramped legs.” Sometimes children have seizures. But it responds well to treatment with a vitamin D2 supplement.
PTH levels in pregnant women vary depending on the trimester. So, in the 1st trimester the norm is 10-15 pg/ml, in the second – 18-25 pg/ml, in the third – 9-26 pg/ml.
Parathyroid hormone is elevated
Increased parathyroid hormone
is one of the most common reasons for patients to visit an endocrinologist - and rightly so, since high parathyroid hormone in the blood always means the presence of a disease that needs to be treated.
An increase in parathyroid hormone is referred to as “hyperparathyroidism”
. High parahormone is the main symptom of hyperparathyroidism. There are two main variants of this condition: primary hyperparathyroidism and secondary hyperparathyroidism. Tertiary hyperparathyroidism is also identified, which occurs in patients with chronic renal failure receiving hemodialysis - but we will not consider it in this article.
Primary hyperparathyroidism is a condition when at the same time parathyroid hormone and calcium are elevated in the blood
. Additional symptoms of primary hyperparathyroidism are a decrease in blood phosphorus (not found in all cases) and an increase in the level of calcium in daily urine (also not in all cases). High parathyroid hormone in the blood in primary hyperparathyroidism is associated with the formation of a parathyroid adenoma - usually a benign tumor that produces parathyroid hormone uncontrollably. The increase in parathyroid hormone in the blood directly depends on the size of the adenoma - the larger it is, the higher the parathyroid hormone is detected. If a patient has primary hyperparathyroidism and parathyroid hormone is elevated - treatment is always surgical - removal of the adenoma gives excellent results, returning all components of phosphorus-calcium metabolism to normal limits.
When a patient has high parathyroid hormone, the causes of this condition may be associated with vitamin D deficiency (we talked about this earlier). If parathyroid hormone is increased in the blood, and calcium is normal or decreased
– most likely, we are talking about secondary hyperparathyroidism, associated with a low amount of vitamin D entering the body. Treatment of such an increase in parathyroid hormone is always carried out in a conservative way, taking vitamin D and calcium supplements.
It is very important, when understanding the reasons why parathyroid hormone is elevated, not to confuse secondary hyperparathyroidism with primary hyperparathyroidism - otherwise the patient will undergo an absolutely unnecessary surgical intervention, the results of which, of course, will not please either the doctor or the patient.
Norms and deviations from the norm
The production of PTH depends on the age of the person. So, the hormone norm for older men and women is:
- from 20 to 22 is 12-95 pg/ml;
- 23-70 years – 9.5-75 pg/ml;
- 71 years and older – 4.7-117 pg/ml.
During pregnancy, the rate ranges from 9.5-75 pg/ml.
If the result of the analysis showed that the PTH content is increased, this may indicate primary or secondary hyperparathyroidism as a result of oncology, Crohn's disease, excess vitamin D, renal failure, rickets, colitis, pancreatic tumor. Thus, primary hyperparathyroidism is indicated by an increase in the hormone by 2-4 times, and secondary hyperparathyroidism by 4-10 times. Also in medicine there is the concept of tertiary hyperparathyroidism. It manifests itself in the form of adenoma of the parathyroid glands and an excess of hormone production - the concentration level exceeds the norm by 10 times or more. This occurs when the need for PTH is low and it is produced in excess.
A reduced concentration of parathyroid hormone indicates magnesium deficiency and hypoparathyroidism (primary, secondary), vitamin D deficiency, sarcoidosis, osteolysis (destruction of bone tissue). Also, a similar result is often found in patients who have undergone thyroid surgery.
Elevated parathyroid hormone - how to cure, where to cure?
For an accurate diagnosis, all patients are recommended to contact specialized centers for endocrinology and endocrine surgery, such as the North-Western Center for Endocrinology in St. Petersburg, the Russian leader in the treatment of hyperparathyroidism.
In our center, we annually consult several thousand patients whom doctors (!) refer for surgery to remove a parathyroid adenoma, but in fact the patients only have a deficiency or insufficiency of vitamin D, which is easily eliminated by taking pills. True, there are also the opposite situations, when patients with large parathyroid adenomas come to us for surgery, for whom the diagnosis has not been established for several years, which simply leads to catastrophic consequences for the body. Every year, several patients with increased parathyroid hormone due to adenoma require resuscitation due to the threat of coma. There are situations when patients undergo surgery on the very first day, the adenoma is removed, and then a two to three month course of resuscitation and restorative treatment is required - that is how far the pathological process goes.
In the vast majority of cases, patients from other regions of Russia at the North-Western Endocrinology Center undergo surgical treatment free of charge, under the federal quota system or simply under a compulsory health insurance policy. Outpatient examinations are carried out for a fee, but their cost is rarely high.
So, if you have elevated parathyroid hormone, it is wiser to come for examination and treatment to a specialized endocrinology center
where you will receive qualified assistance.
Parathyroid hormone is low
The situation when parathyroid hormone is low
, occurs rarely in life. The main reason for a decrease in parathyroid hormone in the blood is a previous operation on the thyroid gland, during which the nearby small and not always clearly visible parathyroid glands were accidentally removed or deprived of blood supply.
Typically, when parathyroid hormone is low, symptoms
include numbness of the fingers and toes, the appearance of an unpleasant feeling of “goose bumps” on the skin, and the appearance of convulsive muscle contractions. The severity of these symptoms depends on the level of calcium in the blood - the lower they are, the worse the patient feels. In severe cases, generalized seizures may develop. If left untreated, the patient may die.
For a condition where parathyroid hormone is low, there is a special term - “hypoparathyroidism”. Many patients with a similar problem are trying to figure out how to increase parathyroid hormone
, however, whether an increase in parathyroid hormone will occur in the future or not after surgery usually depends only on how much injury was caused to the parathyroid glands. If restoration of the function of the parathyroid glands is possible, then it will certainly occur. However, during the entire time that parathyroid hormone is low, patients need to take vitamin D and calcium supplements - sometimes in quite large doses.