Lymph is the living water of our body. The lymphatic system permeates a person completely and is responsible for one of the most important functions - cleansing and immunity. Without lymph, the body would turn into a fetid swamp. But, despite the fact that for the most part she copes well with her responsibilities herself, sometimes she still needs help. Because modern realities are such that the amount of rubbish entering the body significantly prevails over the cleansing capabilities of lymph.
The structure of the human lymphatic system
Since the lymphatic system is part of the vascular system, its structure is very similar. It consists of capillaries, nodes, vessels, trunks, ducts and intercellular fluid, which removes all dirt from the body.
Trunks, vessels and capillaries are a lymph network. It is a plexus of tubes that permeate almost the entire body. It is along them that the very living water moves.
Nodes are formations that are the primary filter. They cleanse the body of dangerous pathogens - a kind of sump.
Ducts are places where the lymph system connects to the circulatory system.
Lymph is a liquid that constantly moves through the trunks, vessels and capillaries.
Anatomy of Human Lymph - information:
Lymph (from Latin lympha - clean water, moisture) is a type of connective tissue. Lymph is a clear, colorless liquid that does not contain red blood cells or platelets, but contains many lymphocytes. Lymph released from small wounds is popularly called ichor. From the capillaries, lymph enters the lymphatic vessels, and then into the ducts and trunks: on the left into the thoracic duct (the largest duct), the left jugular and left subclavian trunks; on the right into the right lymphatic duct, right jugular and right subclavian trunks. The ducts and trunks flow into the large veins of the neck, and then into the superior vena cava. Along the path of the lymphatic vessels there are lymph nodes that perform a barrier and immune role.
The functions of lymph are the return of proteins, water, salts, toxins and metabolites from tissues to the blood. The human body contains 1-2 liters of lymph. The lymphatic system is involved in creating immunity and protecting against pathogens. Through the lymphatic vessels, with dehydration and a general decrease in the protective forces of the immune system, parasites can spread: protozoa, bacteria, viruses, fungi, etc., which is called the lymphogenous route of infection, invasion or metastasis of tumors. Branching inside the organ, lymphatic capillaries pass into small vessels, which, merging and increasing in diameter, form two main lymphatic ducts - the thoracic and right. These ducts flow into the right and left innominate veins of the neck, where the lymph, mixing with venous blood, enters the general bloodstream.
The rate of lymph formation depends mainly on two factors: the permeability of the walls of the lymphatic capillaries and the blood pressure in the venous bed. It has been noticed that when blood pressure in the veins increases (which may be due to impaired outflow of venous blood and the development of edema), the volume of lymph increases. Lymphatic vessels are not compressed even with tissue swelling, due to which excess fluid is removed.
Thus, the lymphatic system performs a drainage function and prevents further development of edema. Experts, not without reason, believe that lymph could tell about what the blood is “silent” about, because many waste products of cells first enter the lymph and then into the blood. The endocrine glands enrich it with hormones, the intestines with nutrients, primarily fats, the lymph flowing from the liver contains a lot of protein, etc. In addition, substances that cannot be absorbed into the venous capillary enter the lymph from cells and tissues . First of all, these are large protein molecules. For them, the wall of the venous capillary is impenetrable, since the pores in it are small, and in the lymphatic capillary they are larger. It is no coincidence that the path to the venous capillary is closed for large protein molecules. After all, these proteins can always turn out to be bacteria, microbes, and toxins that are harmful to the body. Therefore, before entering the bloodstream, they pass through unique checkpoints - lymph nodes located along the lymphatic vessels. There are about five hundred of them. They are small in size - from millet grain to walnut - but they do a very necessary job. Lymph is filtered in them: for example, dust particles that enter the lungs with the air settle, as well as large fragments of cell membranes, tiny pieces of various tissues, which, if they penetrate the blood, could cause the formation of blood clots and blockage of blood vessels. Many pathogenic microbes and their toxins are retained here. And they are not only delayed, but also rendered harmless. Lymphocytes take a big part in this - cells that can almost accurately distinguish “self” from “foreign” and fight the enemy. Lymph nodes are literally stuffed with lymphocytes. They get here with blood and find here very fertile ground for reproduction. After all, lymph is very rich in proteins, fats, and carbohydrates necessary for the construction of new cells. It has been established that after passing through the lymph node, the lymph loses some of the fat and fat-like substances.
There is reason to believe that this part is precisely used to build the cell membranes of lymphocytes. The ability of lymph nodes to utilize fats has recently attracted increasing attention from specialists. And this is due to the role that lymph nodes play in atherosclerotic processes. There is evidence that with atherosclerosis, a violation of lymph flow is often observed, and the lymph nodes seem to be saturated with fat-like substances, in particular cholesterol. Experts have made attempts to normalize lymph flow by using lymphatic and lymphostimulating drugs. It turned out that with increased lymph flow, fat was washed out of the lymph nodes, but - surprisingly - its content in the blood did not increase. It was possible to significantly normalize fat metabolism. This allowed us to assume that not just mechanical washing of tissues from fat and cholesterol occurs, but, obviously, deep mechanisms of regulation of fat metabolism are also included. Researchers are striving to understand the details of these mechanisms in order to then learn how to influence them specifically.
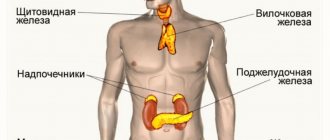
Organs of the human lymphatic system
The main organs of the lymphatic system are the bone marrow and thymus. Secondary - spleen, tonsils, appendix, Peyer's patches, lymph nodes. The main function of these organs is the formation of immune cells in the body.
The spleen monitors the condition of the blood, removes all dead cells and antigens (compounds dangerous to the body) from it.
Secondary organs are connected to other tissues and lymphocytes (such cells) move between them. They pass from the blood to the lymph nodes, spleen and other tissues, and then return back to the blood through the tubes of the lymphatic system. Lymphocytes are formed in the bone marrow, and are also divided in the thymus.
Human immune system
Ph.D. Goldinberg B.M., Vasyuk Ya.V.
City Center for Transfusiology of the health care institution "6th City Clinical Hospital", Minsk,
healthcare institution "7th city children's clinic", Minsk
HUMAN IMMUNE SYSTEM
Introduction
A group of organs that have a common origin, a common structural plan and perform a common function is called an organ system. Five of all ten organ systems are regulatory (control): nervous, circulatory, endocrine, lymphatic and immune. Let us clarify that the lymphatic organs and lymph nodes, of which there are about 600, are functionally part of the immune system, and the lymphatic system itself includes an extensive network of vessels that passes through almost all of our tissues, ensuring the movement of a fluid called lymph.
The word “immunity” comes from the Latin “immunis” (in English – immunity), which means “clean from anything”, immune to anything. The immune system appeared along with multicellular organisms and developed as an assistant to their survival. It unites organs and tissues that guarantee the body’s protection from genetically foreign cells and substances coming from the environment.
The immune system is represented at three levels: organ, cellular and molecular.
Organs of the human immune system
The immune system includes central and peripheral organs.
The central organs of the immune system are the red bone marrow and the thymus.
The bone marrow is the repository of stem cells from which blood cells are formed (Fig. 1). Depending on the situation, stem cells are transformed into immune B lymphocytes. If necessary, a certain part of B-lymphocytes turns into plasma cells, which are capable of producing antibodies.
Fig.1. Bone marrow contains stem cells
The thymus (or thymus gland) is one of the main organs of the immune system, located in a person behind the sternum below the collarbone, which is responsible for the formation of T-cells of the immune system in the lymphoid tissues of the body (Fig. 2).
Fig.2. Thymus
Peripheral organs include the spleen, tonsils and lymph nodes, which contain areas of maturation of immune cells.
Tonsils, which got their name because of their external resemblance to almonds, are a collection of lymphoid tissue in the upper part of the nasopharynx. A person has six tonsils: two palatine, two thoracic, and one each nasopharyngeal and lingual.
The largest of them are the palatine tonsils, or tonsils, which can be easily examined independently in the mirror if you open your mouth wide enough (Fig. 3).
Rice. 3. Palatine tonsils
The spleen is the largest lymphoid organ (Fig. 4). In addition, it can accumulate some blood. In emergency situations, the spleen is able to send its reserves into the general bloodstream. This allows you to improve the quality and speed of the body's immune reactions. The spleen cleanses the blood of bacteria and processes all kinds of harmful substances. It completely destroys endotoxins, as well as the remains of dead cells from burns, injuries or other tissue damage. In people who are left without a spleen for any reason, their immunity deteriorates.
Rice. 4. Spleen
Lymph nodes are small round-shaped formations (Fig. 5), located in the chest cavity (bronchopulmonary, bronchotracheal) and abdominal cavity (Peyer's patches, appendix and others), perithoracic on the surface of the chest, on the neck and on the limbs. The lymph node is one of the barriers to infections and cancer cells, playing the role of a kind of customs (Fig. 5). It produces lymphocytes - special cells that take an active part in the destruction of harmful substances.
Rice. 5. Lymph node
The central organs of the immune system are responsible for the formation and maturation of cells, and the peripheral organs provide protection, that is, the immune response. The peripheral and central organs of the immune system perform their work only together, and if any one of these organs fails, the body will lose its protective barrier.
Components of the immune system
Modern immunology distinguishes between two interacting components of the immune system - innate and acquired types of immunity , which ensure the development of an immune response to genetically foreign substances (entities).
Innate (species) immunity is a hereditarily fixed system of protecting the human body from pathogenic and non-pathogenic microorganisms, as well as products of tissue decay. Innate immune cells recognize pathogens by molecular markers specific to them—the so-called “pathogenicity patterns.” These markers do not allow one to accurately determine whether a pathogen belongs to one species or another, but only signal that the immune system has encountered troublemakers: a stranger or one’s own, but who has become a traitor to the body (Fig. 6).
Fig.6. Innate immunity: the main thing is calm!
Innate immunity at the cellular level is represented by:
- monocytes are the precursors of macrophages (cells that devour foreign particles). They are formed in the bone marrow, then enter the blood, but quickly leave it, turning into tissue macrophages and dendritic cells (Fig. 7);
Fig.7. Monocyte
- macrophages and dendritic cells are located in the skin and mucous membranes. They have mobility and are transported through the blood and lymph. They absorb (phagocytose) the pathogen, and within themselves, using the contents of the vacuoles, dissolve it. Dendritic cells branch like a tree. Thanks to the antenna branches, they work as communicators between the innate and acquired types of immunity (Fig. 8);
Fig.8. dendritic cell and
and macrophage
- blood cells containing granules (granulocytes) in the cytoplasm: neutrophils, eosinophils and basophils (Fig. 9);
Fig.9. Granulocytes
Neutrophils are the most numerous immune cells in human blood. They circulate in the blood for only 8-10 hours and spend most of their lives traveling through body tissues. When they encounter a pathogen, they capture it and digest it, after which they usually die themselves. Granules containing antibiotic substances are released from the destroyed neutrophils.
Granules of eosinophils and basophils provide chemical defense of the body against large pathogens, for example, parasitic worms, fungi, and extracellular bacteria. However, with excessive activity they can also participate in the development of an allergic reaction;
- natural killer cells or NK cells (English Natural killer cells, NK cells) are a type of cytotoxic lymphocytes involved in the functioning of innate immunity. They destroy cells infected with bacteria and viruses, as well as tumor cells, at high speed.
Fig. 10. Natural killer
Natural killers act with the help of aggressive substances perforin and granzyme, which, like gimlets, “bite” and destroy the affected cell that has become their target (Fig. 11)
Fig. 11. Penetration of perforin and granzyme into a cancer cell and its destruction
The molecular (humoral) factors of innate immunity are (Fig. 12):
- proteins that bind metal ions (iron, zinc) necessary for the life and reproduction of pathogens - lactoferrin, calprotectin, membrane protein and others;
- enzymes that generate oxidizing agents - oxygen and nitric oxide:
- enzymes capable of breaking down the cell membrane of pathogens - lysozyme, chitinase, phospholipase A2;
- proteins and peptides that violate the integrity of the cell membrane of a microorganism - complement, eosinophilic protein, defensins and others.
Fig. 12. Humoral factors of innate immunity
The complement system is a multicomponent, self-assembled system of more than 20 serum proteins that are normally inactive.
After activation, the biological effects of complement appear: the formation of a membrane attack complex for the lysis of pathogens, the release of inflammatory mediators to attract phagocytes and enhance their absorption capacity.
Cytokines are a system of low molecular weight proteins of the body, synthesized mainly by active cells of the immune and hematopoietic systems, regulating intercellular interactions (a “universal” language for all cells), presented in Fig. 13 and 14.
Rice. 13. Cytokines: IL – interleukins, of which there are currently 34 varieties;
Rice. 14. Multidirectional action of cytokines using the example of interferon gamma
As a result of activation of humoral and cellular factors of innate immunity, a basic reaction of infectious inflammation is formed within several hours after the introduction of a pathogen into the internal environment of the body (Fig. 15)
Rice. 15. Infectious inflammation of tissue at the site of foreign body insertion for the purpose of its removal
Acquired immunity (or adaptive – from the French adapter “ to adapt ” ) is formed individually during life under the influence of antigenic stimulation and, in turn, is divided into natural and artificial (Fig. 16).
Fig. 16. Adaptive
immunity
Natural immunity is formed when encountering a pathogen, as a result of which protective immune factors are produced in the body (active natural immunity), or they come ready-made from maternal orgasm during fetal development or during breastfeeding (passive natural immunity).
Artificial immunity is created by administering vaccines or toxoids that stimulate the production of antibodies against specific pathogens or their poisons. At the same time, for preventive purposes, the process of the patient’s immune system’s reaction to the pathogen is reproduced, but in an asymptomatic or mild clinical form, while maintaining their protective immune power for several months, years, or even for life (artificial active immunity). When it is necessary to quickly and for a short time protect a patient from the real risk of encountering a pathogen during an epidemic or neutralize a pathogen that has already entered his body, immunoglobulins (antibodies) are used both in purified form and in dosed volumes of plasma or serum obtained from the blood of a donor ( person or animal). The use of ready-made antibodies forms passive artificial immunity that lasts 2-3 weeks.
Adaptive immunity is based on three main processes:
- recognition of antigens (usually foreign to the body) using receptors;
- removal (elimination) of recognized foreign agents (Fig. 17);
- the formation of an immunological memory of contact with an antigen, allowing for faster and more efficient removal of this antigen when it is recognized again.
Fig. 17. Options for the response of the immune system to organ or tissue transplantation, the occurrence of malignant neoplasms and infections
The immunocompetent cells of adaptive immunity are lymphocytes that live in the human body from several months to several years. According to their functions, cells are divided into T-lymphocytes - 80% and B-lymphocytes - 20%.
The fact that the T lymphocyte recognizes only foreign antigens, and not molecules from its own body, is a consequence of a process called selection, which occurs in the thymus, where T cells complete their development. The essence of selection is this: the cells surrounding the young, or naive, lymphocyte show (present) to it the peptides of their own proteins. The lymphocyte that recognizes these protein fragments too well or too poorly is destroyed. The surviving cells (and this is less than 1% of all T-lymphocyte precursors that came to the thymus) have an intermediate affinity for the antigen, therefore, they, as a rule, do not consider their own cells to be targets for attack, but have the ability to react to a suitable foreign peptide.
To activate a T-lymphocyte, it needs to receive special signals from the receptors of the leukocyte antigen system and a cocktail of many pro-inflammatory cytokines.
Using special reagents, markers of surface proteins of leukocytes of a certain type are determined, which are called clusters of differentiation (CD). Currently, 350 CD antigens and their subtypes are known (Table 1).
Table 1. Main identification CD markers of cells
| Cluster designation | Cells |
| CD 10, CD34 | Lymphoid stem cell |
| CD3 | T lymphocyte |
| CD4 | T helper |
| CD8 | T-killer |
| CD19, CD72, CD79, etc. | B lymphocyte |
| CD16/ CD56 | NK cells |
| CD14, CD64 | Monocyte/macrophage |
T lymphocytes recognize cells carrying foreign antigens and destroy them after direct contact (attack), and also perform the function of regulating the immune response.
T lymphocytes have subtypes (Fig. 18):
Rice. 18. Subtypes of T-lymphocytes and their functions
- Killer T cells (also called CD8+ T lymphocytes), which, like an NK cell (natural killer), secrete the proteins perforin and granzyme, which leads to lysis of the target cell;
- T-helpers (from English helper - assistant). They are also referred to as Th cells, CD4+ T lymphocytes. Activated T helper cells produce chemokines and cytokines involved in the immune process (Fig. 19);
Rice. 19. Activation of different subpopulations of T-helper cells by cytokines
- Suppressor T cells (Ts) inhibit (suppress) B cell responses and block helper T cells. Moreover, these cells do not sabotage immune processes and do not harm health. They simply regulate the strength of the immune response, which allows the immune system to respond to stimuli with restraint and with moderate force (putting out a fire, not a fire);
- T-regulatory cells (Tr1) influence the formation of granular leukocytes (granulocytes), which we have already introduced as macrophages.
The ratio of CD4/CD8 cells is called the immunoregulatory index (IRI). If the patient’s IRI is increased (more than 2.2), this indicates excessive activity of T-helper cells and a weakening of the regulatory function of T-killer cells. At this rate, immune cells can destroy the body’s own tissues. Increased IRI is most often observed in patients with autoimmune diseases (systemic lupus erythematosus, scleroderma, rheumatoid arthritis, etc.). The cause of excessive activity of T-helper cells can also be a tumor of the thymus gland. With this pathology, an excessive number of lymphocytes are produced. High rates of IRI are observed in acute lymphoblastic leukemia. This severe oncological disease is accompanied by an uncontrolled increase in the number of immature lymphocytes.
If the immunoregulatory index is reduced (less than 1.6), then this indicates a serious deterioration in the functioning of the immune system. Low levels of IRI indicate that the function of protective cells in the body is weakened, and regulation by T-killers is excessive. This is usually observed in the following pathologies accompanied by immunodeficiency: infectious diseases (including HIV infection); congenital immunodeficiency; any protracted and chronic diseases; bone marrow tumors.
B lymphocytes are responsible for the humoral component of immunity - the production of antibodies. After an antigenic stimulus, the B lymphocyte turns into a lymphoblast, a cell capable of dividing. Some lymphoblasts differentiate into memory B lymphocytes, the other part turns into plasma cells that produce antibodies.
B lymphocytes carry the B cell receptor on their surface. Upon contact with an antigen, these cells are activated and turn into a special cell subtype - plasma cells , which live up to three weeks and have the unique ability to secrete thousands of antibodies .
The antibody has an affinity for the antigen it recognizes and, as it were, “sticks” to it. This allows antibodies to envelop (opsonize) cells and viral particles coated with antigen molecules, attracting macrophages and other immune cells to destroy the pathogen. Antibodies are also able to activate a special cascade of immunological reactions called the complement system, which leads to perforation of the pathogen’s cell membrane and its death.
Rice. 20. Antibody production and pathogen marking
There are several classes of antibodies (immunoglobulins). The first to appear after antigenic irritation, causing agglutination of bacteria and neutralization of viruses, are immunoglobulins M (IgM). Immunoglobulins G (IgG) are involved in long-term immunity.
Table 2 provides an interpretation of laboratory tests for the presence of a pathogen at the molecular level and using tests for immunoglobulins M and G.
Table 2. Interpretation of laboratory tests for the presence of a pathogen at the molecular level
| Result of molecular research | Antibody test | Interpretation | |
| IgM | IgG | ||
| Positive | Negative | Negative | Acute infection |
| Positive | Positive | Negative | Acute infection |
| Positive | Positive | Positive | Infected patient |
| Positive | Negative | Positive | Infected or re-infected patient |
| Negative | Positive | Negative | Early stages of infection. More research needed |
| Negative | Positive | Positive | Infection. More research needed |
| Negative | Negative | Positive | Post-infectious period |
| Negative | Negative | Negative | Uninfected patient |
Innate and acquired types of immunity have points of contact, which represent two triads (Fig. 21)
Rice. 21. Two triads combining innate and acquired types of immunity
The development of an adaptive immune response takes quite a long time (from several days to two weeks), and in order for the body to defend itself against an already familiar infection faster, so-called memory cells . They, like veterans, are present in the body in small quantities, and if a pathogen familiar to them appears, they are reactivated, quickly divide and come out as an entire army to defend the borders (Fig. 22).
Fig.22. Memory T cells quickly form a secondary immune response
Immunological tolerance
Immunological tolerance (tolerance, arereactivity) is understood as the absence of an immune response to a specific antigen. The list of antigens to which tolerance can develop is practically indistinguishable from the set of antigens against which a specific immune response develops (Fig. 23).
Rice. 23. Immune tolerance
Tolerance mechanisms are necessary because the immune system produces a huge variety of antigen-specific receptors, and some of them are specific to the body's own antigens; Tolerance prevents unwanted reactions against one’s own organs and tissues, also for the normal course of pregnancy.
Immune system disorders in humans
Immune system disorders can be divided into three categories: immunodeficiencies, autoimmune diseases, and hypersensitivity reactions.
Immunodeficiencies
Immunodeficiency is a decrease in the quantitative indicators and/or functional activity of the main components of the immune system, leading to a disruption of the body’s defense against pathogenic microorganisms and manifested by an increased incidence of infectious diseases.
Primary immunodeficiencies (PIDs) are hereditary diseases caused by defects in genes that control the immune response. In general, PIDs manifest themselves already in early childhood, but sometimes only by the age of 30-40.
- symptoms that may be signs of primary immunodeficiencies:
- 4 or more cases of otitis during the year;
- 2 or more sinusitis during the year;
- low effectiveness of antibiotics for two or more months of use;
- 2 or more cases of pneumonia during the year;
- the child’s inability to gain weight and grow normally;
- frequent and deep abscesses of the skin and internal organs
- constant candidiasis of the oral cavity and skin;
- the need for intravenous antibiotics to resolve the infection;
- two or more systemic infections, including sepsis;
- hereditary predisposition.
According to development mechanisms, there are 4 main groups of PIDs (Table 3):
- Group 1 – predominantly humoral or B-cell PIDs;
- Group 2 – combined PID (all T-cell immunodeficiencies have impaired B-cell function);
- Group 3 – PID caused by defects in phagocytosis;
- Group 4 – PID caused by defects in the complement system.
Table 3. Some primary immunodeficiencies
| Pathology | Symptoms | Diagnostics | Treatment |
| Defects in antibody formation | |||
| Agammaglobulinemia | Frequent bacterial infections | Deficiency or complete absence of B lymphocytes | Antibiotics, lifelong administration of IgG |
| General variable immune deficiency | Frequent respiratory infections, otitis | Defects of T- and B-lymphocytes | Antibiotics, lifelong administration of IgG |
| Combined PIDs | |||
| Ataxia-telangiectasia (Louis-Bar syndrome) | Abnormal motor function, muscle weakness, speech impairment | Deficiency of T- and B-lymphocytes | Symptomatic |
| PID caused by defects in phagocytosis | |||
| Chronic granulomatous disease | Frequent pneumonia, purulent infections | Genetic defect | Lifelong antibacterial and antifungal therapy, interferon gamma |
| PID caused by defects in the complement system | |||
| Hereditary angioedema | Swelling of the lips and eyelids without itching. Swelling of the larynx, nose, tongue is life-threatening | Low concentration of C1 esterase inhibitor | Administration of C1 esterase inhibitor concentrate |
As follows from Table 3, the main and often the only treatment method for most patients with primary B-cell immunodeficiencies are immunoglobulins. These are medicines obtained from human blood plasma. They are designed to replace protective antibodies missing in the immune system in order to prevent or stop the development of severe infectious diseases. Today, a doctor’s arsenal includes immunoglobulins that differ in the concentration of the active substance (5 and 10%), as well as in the method of administration (intravenous and subcutaneous).
PID can appear at any age. Depending on this, the patient has unique problems that require certain types of support throughout his life (Table 4).
Table 4. Need for types of support for patients with PID in different age groups
| Age, years | Types of support | |||
| families | doctor | psychologist | society | |
| 0-14 | +++ | + | + | +++ |
| 14-18 | +++ | + | +++ | +++ |
| 18-65 | + | ++ | + | +++ |
| Over 65 | + | ++ | ++ | +++ |
Between the ages of 0 and 14 years, parental care is required to prevent infections and during the treatment period. May require: home training; providing psychological assistance; social support in purchasing medicines.
In adolescence (14-18 years), additional needs may arise for continued continuous education, vocational guidance, establishing relationships with peers, and organizing leisure time.
At the age of 18 to 65 years, patients more often experience infectious complications, and with them the costs of purchasing medications that are not subject to replenishment, as well as problems with employment.
In old age (over 65 years), there are needs for material, social and psychological support for a patient with PID.
Autoimmune pathology
Damage to the body's own organs and tissues by the immune system is called an autoimmune process . About 5% of humanity suffers from diseases of this type. The patient’s body develops hostilities reminiscent of a civil war: “friends against friends” go on the attack. There are no winners in this struggle - only suffering.
The selection of T lymphocytes in the thymus, as well as the removal of autoreactive cells in the periphery (central and peripheral immunological tolerance), which we discussed earlier, cannot completely rid the body of autoreactive T lymphocytes. As for B lymphocytes, the question of how strictly their selection is carried out still remains open. Therefore, in the body of every person there are necessarily many autoreactive lymphocytes, which, if an autoimmune reaction develops, can damage their own organs and tissues.
As an analogue, we can cite the Janissary infantry created by the Turks in the 14th century, which recruited Christian youths aged 8-16 who fought against their relatives.
T-cell autoimmune aggression has been well studied in rheumatoid arthritis, type 1 diabetes, multiple sclerosis and many other diseases.
The same Janissary cells, which do not remember their kinship, can be traced among B-lymphocytes:
- autoantibodies can cause cell death by activating the complement system on their surface or attracting macrophages;
- Receptors on the cell surface can become targets for antibodies.
For example, due to a breakdown of immunological tolerance, B-lymphocytes that produce antibodies are activated. This leads to a marked increase in the production of thyroid hormones (T4 and T3), as well as an increase in the size of the thyroid gland (hypertrophy). The pathology is called Graves' disease.
Another example would be myasthenia gravis, which is characterized by skeletal muscle weakness due to the formation of autoantibodies against structures responsible for cholinergic transmission and muscle fiber contraction;
- autoantibodies, together with soluble antigens, can form immune complexes that settle in various organs and tissues (for example, in the renal glomeruli, joints, on the vascular endothelium), disrupting their function and causing inflammatory processes.
Typically, an autoimmune disease occurs suddenly, and it is impossible to determine exactly what caused it. It is believed that almost any stressful situation can serve as a trigger, be it an infection, injury or hypothermia. A significant contribution to the likelihood of an autoimmune disease is made by both a person’s lifestyle and genetic predisposition - the presence of a certain variant of a gene.
Hypersensitivity
Hypersensitivity refers to an excessive immune response to an antigen. Hypersensitivity reactions are divided into several types depending on their duration and the mechanisms underlying them:
- Type I hypersensitivity involves immediate anaphylactic reactions, often associated with allergies. This type of reaction can range from mild discomfort to death. The basis of type I hypersensitivity is immunoglobulin E (IgE), which causes degranulation of basophils and mast cells;
- Type II hypersensitivity is characterized by the presence of antibodies that recognize its own proteins and mark the cells that express them for destruction. Type II hypersensitivity is also called antibody-dependent or cytotoxic hypersensitivity and is based on immunoglobulins G (IgG) and (IgM);
- type III hypersensitivity is caused by immune complexes consisting of antigens, complement proteins, IgG and IgM;
- Type IV hypersensitivity, also known as delayed hypersensitivity, develops over 2-3 days. Type IV hypersensitivity reactions are observed in many autoimmune and infectious diseases and are based on T cells, monocytes and macrophages.
Effective methods of influencing the immune system:
- Regular vaccination in terms of speed and quality of reaction exceeds the natural process of developing immunity to a specific infection;
- a balanced diet that ensures the maintenance of normal metabolism;
- regular physical activity ensuring the physiological functioning of all body systems and maintaining optimal body weight;
- giving up bad habits that lead to addiction (alcohol, nicotine, drugs, toxic, computer);
- daily routine, especially the influence of circadian rhythms (day and night): during wakefulness, the number of T-killer and NK cells peaks, as well as the concentration of anti-inflammatory substances such as cortisol and catecholamines; During sleep, the formation of memory T cells reaches its peak.
Speculative methods around immunity:
- taking immunostimulants is not clinically justified. If you constantly stimulate the production of leukocytes with drugs, the immune system will begin to lose its direct functions. This is when the moment of serious problems with immunity begins. Natural adaptogens do not affect the immune system at all: Schisandra chinensis, ginseng, eleutherococcus, radiola rosea. They act as amplifiers of RNA and protein synthesis (the basis of human cells), activate metabolic enzymes and the work of the endocrine and vegetative systems;
- Taking vitamins is clearly overrated. Vitamin D has a positive effect on the immune system, which stimulates the formation of T-killer cells. All other groups of vitamins do not directly participate in the functioning of the immune system;
- bath procedures and sauna do not affect the immune system;
- folk remedies such as honey and garlic have a mild bactericidal but not immunogenic effect.
Conclusion
The immune system is represented by three levels: organ, cellular and molecular with complex interactions between them.
Modern immunology distinguishes two interacting components of the immune system - innate and acquired (adaptive) types of immunity, which ensure the development of an immune response to genetically foreign substances, which are microorganisms, malignant tumor cells, transplanted organs and tissues.
Adaptive immunity is based on three main processes: recognition of antigens, their removal (elimination) and the formation of immunological memory.
Failures in the structure of the immune system lead to the development of immunodeficiencies, autoimmune diseases or hypersensitivity reactions.
Immunodeficiency at the genetic level (primary) or acquired (secondary) can appear at any age and lead to increased infectious morbidity. In recent years, replacement therapy has become available to prolong the lives of these patients. To improve their quality of life, it is necessary not only to provide expensive treatment, but also to organize support from family, psychologists and social institutions.
Autoimmune diseases and hypersensitivity are the body’s inability to resist a raging immune system that has confused its own and someone else’s.
Unfortunately, medicine has not yet learned to cure any of the diseases of the immune system, but only to use replacement therapy.
Effective preventive methods of influencing the immune system are vaccination and a healthy lifestyle. No one has yet been able to buy immunity at the pharmacy.
Composition of lymph
Lymph is very rich in composition. It contains:
- a huge number of lymphocytes;
- red blood cells, which in normal times are not contained in very large quantities, but during injuries they multiply rapidly. If you look at your wound, which begins to slowly heal, you will see a thin film - it appeared thanks to this reproduction;
- granulocytes - activated during infectious infections;
- proteins, lipids, amino acids, glycerin, glucose, electrolytes and other compounds - their quantity depends on how much water you drink. For lymph to work properly, the body needs a normal and regular supply of moisture;
- Lipoproteins - in common parlance these are cholesterol and phospholipids. Their quantity depends on nutrition. The better you eat, the fewer of them there are.
How does the human lymphatic system work?
Every day, through air and food, “enemies” enter our body - toxic substances, bacteria, viruses and infections. In addition, cells are constantly renewed. And so that all this unpleasant bouquet does not accumulate inside, there is a lymphatic system that removes everything. But cleansing is not the only function of the lymphatic system.
It also helps protect the body by producing immune cells, which determine how a particular virus will affect us and how long we will be sick if damage to our health is caused.
Humoral function once again proves that our body works as a coherent integral mechanism, where one thing depends on the other. It is responsible for transmitting impulses that tell what substances need to be synthesized for proper functioning.
The lymphatic system also transports nutrients. Delivery of lipids and albumin molecules into the blood. On average, every day about 100 grams of protein enters the blood from lymph, without which the body cannot function normally.
Excess fluid is removed from the body with lymph. This function is called drainage and, if it is disrupted, swelling may appear, sometimes so severe that it interferes with movement.
Human lymphatic system: pattern of lymph movement
Lymph flow is strictly coordinated by the anatomy of the human lymphatic system: even a slight change in this case can lead to irreversible consequences. Normally, lymph flows along the channel from bottom to top, that is, from the smallest capillaries to large ducts, and only in this direction; the reverse flow of lymph is a serious pathology and is normally impossible in principle.
Lymphatic capillaries are the smallest units of the lymphatic system; they begin the lymph flow cycle. On the one hand, they have a closed end, on the other, they flow into larger capillaries and vessels of the lymphatic bed. The capillary walls have a very thin, almost transparent structure, due to which liquid and larger protein molecules seep inside freely, which distinguishes them from blood capillaries, which do not have such a high throughput.
Lymphatic vessels are larger tubes through which lymph moves from the capillaries to the trunks. Their structure is somewhat reminiscent of the veins of the circulatory system, however, as in the case of capillaries, the walls of the lymph vessels are thinner. In addition, inside these vessels there are a large number of tightly closed valves that prevent the flow of lymph in the opposite direction.
On the way from the capillaries to the trunks, lymph enters the lymph nodes located along the vessels. Such formations are divided into groups depending on location. As a rule, each lymph node looks like a small spherical or oval formation about 2 cm in diameter, into which several vessels flow, and only 1-2 exit. This is where the main filtration of lymph occurs - foreign bodies are separated and lymphocytes are produced when pathogens are detected.
Departing from the lymph nodes, the efferent vessels gradually flow into 2 key trunks of the lymphatic system, resulting in the formation of the same number of ducts - the thoracic and the right:
- The thoracic lymph duct begins in the capillaries of the left arm, the left side of the head and internal organs located below the costal line. Its terminal point is the left subclavian vein.
- The right lymphatic duct, accordingly, starts from the right arm, the right half of the head and chest and flows into the right subclavian vein.
In the circulatory system and liver cells, immune processes that began in the lymph nodes are completed, as a result of which the main pathogens are neutralized, and toxins and poisons are eliminated from the body. In addition to the immune reaction, in this way most of the fluid is transferred from tissue cells and interstitial space into the bloodstream. The driving force of lymph flow directly depends on the physiology and anatomy of the human lymphatic system:
- The different diameters of the tubes of the lymphatic system, from the smallest capillaries to large ducts, provide a noticeable difference in hydrostatic pressure, which lifts the lymph: if at the initial stage of the channel the pressure is from 2 to 5 mm Hg. Art., then closer to the ducts this figure gradually approaches zero.
- The vascular walls of the human lymphatic system include smooth muscle cells capable of alternate contraction and relaxation. Thanks to this, lymph can move towards the duct.
- Contraction of the muscle fibers surrounding the lymphatic vessels periodically increases the pressure within the lymphatic system, causing the fluid to flow faster.
Any malfunction, blockage or other disturbance leads not only to the development of a disease against the background of reduced immunity, but also to tissue swelling up to the formation of a non-malignant tumor.
Lymph cleansing points
Cleansing usually occurs through the excretory and digestive systems. But sometimes they fail and the body begins to use other organs.
Vagina in women and urethra in men
Some dangerous microorganism entered the body, the lymphatic system quickly dealt with it and begins to get rid of the “corpses” of these bacteria. In women, this is usually accompanied by copious vaginal discharge (in severe cases, itching may occur); in men, the discharge is accompanied by pain when urinating.
What do people usually do in this case? Without dealing with the problem, they swallow pills. But this does not help solve the root cause, but only removes the effect. The tablets extinguish the body’s ability to cleanse itself, but it does not save you from dangerous microorganisms - they hide in other organs and cause harm there. In addition, the pills have a strong effect on the liver and ultimately only harm us.
It is necessary to fight not with the discharge, but with what caused it.
Gastrointestinal tract
The gastrointestinal tract is penetrated by many lymph nodes, so it is also involved in cleansing. The intestines not only release leftover food, but also poison that somehow got inside us.
Various disorders, pain, flatulence are the result of the fight between the lymphatic system and bacteria. If all this bothers you quite often, take care of your immunity urgently!
Sweat glands
Various poisons, toxins and hormones are released through sweat. And the main concentration of this power is the armpits. And instead of letting them work normally, we use deodorants. As a result, not finding a way out, the lymph drives all the dirt further and ends up in the chest. And this is where mastopathy occurs.
If you absolutely cannot do without deodorant (this is logical, no one wants to smell bad), then at least stop using them 24/7. And replace it with organic options. For example, mineral deodorant from Beauty 365. It does not block the work of the sweat glands, but gently regulates it.
If possible, shower and wash off cosmetics more often. You should sweat - it's normal!
Nose
The nose is one of the main filters. It cleans the inhaled air from dust and bacteria. Excessive mucus production may not be a symptom of a cold, but only a protective reaction of the body. In this case, you should not treat the snot, but you need to find out the reason why it appeared.
Tonsils
Previously, tonsils (and adenoids too) were considered unnecessary organs and doctors calmly cut them out. But it's not right! They are an important part of the lymphatic system. This is where the fight between viruses and lymphocytes occurs, and immune cells are released.
If the functioning of the tonsils is disrupted, then the person is constantly sick, and the tonsils become inflamed. We start treating them with antibiotics, but they either fail or their effect wears off quickly. As a result, they are removed, but the problem does not go away. Viruses go further, capturing the trachea, larynx, bronchi and lungs. Before removing inflamed tonsils or adenoids, try to cleanse the lymphatic system. This should help.
Airways
When the mucous membranes of the nasal cavity are unable to cope with the infection, it can pass on. Laryngitis occurs in the larynx. If it was not possible to cope with the virus there, then it goes further and can cause tracheitis, bronchitis and, at the end of its journey, even pneumonia.
How to preserve the lymphatic system: prevention of pathologies
If the lymphatic system is overloaded or clogged, then health problems are sure to appear. Try to minimize negative influence from the outside - don’t miss anything that can cause harm. At a minimum, you can start with proper nutrition. Be sure to include foods that stimulate intestinal function in your diet.
Lymphatic drainage massage is a wonderful technique that allows you to disperse stagnant fluid, which means it improves the removal of toxins.
Special exercises and breathing exercises also help cleanse the lymph nodes and ducts.
A sedentary lifestyle harms all organs, but the lymph suffers first. Have you been sitting at work for a long time? Get up and walk around the office, do some light exercises. Try to walk outdoors every day.
Lymph nodes are very sensitive to temperature changes. Avoid hypothermia or overheating - they can lead to inflammation.
And, of course, avoid stress! Depressive states cause the release of a hormone that slows down all processes and leads to spasms. Sleep at least 7-8 hours, meditate, take vitamins and smile more often.
Inner Britain: what should healthy lymph flow look like?
The lymphatic system does not have a heart. The movement of lymph is created not by a powerful pump, but by a thin, delicate, vulnerable valve system. Its work depends on the fluidity of lymph, vascular tone, tissue turgor, blood pressure, temperature, degree of dehydration... And our health and well-being also largely depend on the lymph itself. Let's figure out what lymph likes, what it doesn't like, how it moves and how we can take care of it.
Lymph is a clear or slightly yellowish liquid substance with a slightly alkaline reaction. It includes:
- lymphocytes,
- single red blood cells,
- protein compounds,
- lipids,
- glucose,
- cholesterol,
- phospholipids,
- and also fat-soluble toxins, cellular breakdown products and pathogens that the lymph has removed from the tissues.
All this is contained in the lymph in one concentration or another, but the main carrier component is the universal natural solvent - water. Water balance for lymph is extremely important, because its volume in the human body is 5 times greater than the volume of blood.
If there is not enough water, the concentration of protein compounds in the lymph increases. Normally, the speed of lymph flow is 0.5-0.8 cm/sec, but if the lymph becomes thicker, it flows slower, and this threatens stagnation.
One of the signs of an existing lymph flow disorder is cellulite . The loose, uneven structure of subcutaneous fat tissue indicates not so much the deposition of fat, but rather the fact that the lymph cannot cope with the removal of toxins and “hides” them in fats, where they can be stored for years. And with sudden weight loss, it comes out, enters the bloodstream and causes disease.
Also, a problem with the lymphatic system is indicated by swelling and depressed red stripes from the bed in the morning. When the body has enough fluid, the turgor (elasticity) of the tissues is normal, and the excretory systems (in particular, the kidneys) are in order, such symptoms are absent.
What slows down lymph?
- Drinking alcohol, coffee, soda
- Smoking
- Unhealthy and difficult to digest food
- Lack of clean water
- Excess salt and sugar in the diet
- Wearing tight, tight clothing or high-heeled shoes
- Taking medications
- Physical inactivity
What speeds up lymph?
- Drinking clean water
- Normalization of diet
- Rejection of bad habits
- Lymphatic drainage massages
- Exercises for the lymphatic system
- Competent herbal medicine
The movement of lymph should not be too slow, but it should not be too fast either. Lymph needs time to wash every cell. She is not a sprinter, but a tireless slow mover who slowly collects garbage and carries it away so that the tissues can function safely.
useful for the lymphatic system to carry out unloading from time to time first of all, food. During these periods, you should give up complex culinary delights to help yourself.
An important note for those who are looking for a way to effectively cleanse the lymphatic system. The lymphatic system is itself a means of cleansing. It does not need total cleansing, and it is impossible to free it 100% of toxins, because a number of toxins are produced and released by our own cells. Naturally.
But mild detoxifications are acceptable and beneficial. Those who want to do this competently are recommended to take a short series of “Dietetics Light” lessons from immunodietologist™, nutritionist with 30 years of experience, Marina Nikolaevna Vnukova. This will help you prepare properly, personalize your cleansing regimen, and avoid worsening your condition due to improper, abrupt detoxification of the body.
Lymph formation: what is it and how does it happen?
Oxygen and other nutrients are supplied to tissues and organs through the blood. But they need to be cleansed so as not to clog the body. So, through the walls of the capillaries, filtration occurs into the intercellular space, where a special tissue fluid is formed. But it not only cleanses the blood, but also additionally nourishes it with necessary elements.
This fluid then enters the lymphatic vessels, where it is saturated with lymphocytes and turns into lymph. All lymph moves in one direction - towards the heart.
Diagram of the lymphatic system: what does the human lymphatic system consist of?
The lymphatic system is a global cleansing structure that removes poisons and pathogens from all tissues and organs of the body.
Ignorance of the principles of its work in everyday life leads to serious consequences for health: going to baths and saunas at the wrong time for the lymphatic system, incorrect massage techniques, and incorrect drinking balance.
In clinical practice, an approach to therapy without taking into account the state of the lymphatic system leads to incorrect prescriptions and damage to the patient’s health, in particular, disruption of the microbiota as a result of improper withdrawal from antibiotic therapy.
To prevent this from happening, it is extremely important to understand how the lymph system works. Therefore, first we will talk about the structure of the lymphatic system and where it originates.
Globally, the lymphatic system consists of lymph itself and two sections:
- transport - including lymphatic capillaries, postcapillaries, vessels, trunks and ducts; ensures the movement of lymph;
- lymphoid organs - including lymph nodes, spleen, thymus, tonsils and red bone marrow; provide filtration of lymph, study of pathogens and production of blood and immune system cells.
Lymph flow begins in the intercellular space, from where lymph is collected by microscopic vessels ( capillaries ) consisting of a thin layer of endothelial cells. Lymphatic capillaries have no valves. It moves along them from the bottom up due to the contractile movements of the microfilaments of the cells surrounding the vessels.
Then the lymph enters the postcapillaries - vessels with a double layer of endothelium and valves that promote the movement of lymph. Their functional unit is called lymphangion - a segment from one valve to another. Thanks to these valves and the contractile activity of the lymphangions, further upward flow of lymph is ensured.
In total, there are about 500 lymph vessels in the body. They are divided into:
- collecting,
- diverting,
- main lines.
Collecting vessels are a capillary network that draws lymph from the extracellular matrix. The drainage vessels are larger and carry lymph from the organs to the lymph nodes.
Collecting and discharging lymph vessels follow the blood vessels, often along the veins. The main vessels are part of the neurovascular bundles and are located inside the common fascial sheath.
After passing through the lymph nodes, the lymph enters the lymphatic lines (or trunks), which drain lymph from the head, upper and lower extremities, chest and abdominal cavity.
On the thoracic duct is located one of the most important lymph collectors in the body - cisterna chyli or milk cistern. From it, as well as through other, smaller lymphatic ducts, lymph centrally enters the venous bloodstream, and the blood is sent to the liver for purification.
So lymph - “the living water of the human body” - goes through a full cycle and, in fact, washes our body from bottom to top. The exception is the head: here the lymph flows from top to bottom, and in addition, the brain does not have its own lymph nodes, it uses “neighboring” ones - the cervical and submandibular ones.
When working properly, such a “ filter ” is able to resist any infections that try to attack our body. But if everything were that simple, you and I wouldn’t get sick. Let's figure out how the lymphatic system works and what we should never do if we want to keep it healthy.
Why do we need lymph nodes? What happens if the lymphatic system fails?
The tonsils became inflamed, the splinter caused suppuration of the finger - this is all the work of the lymphatic system. She is responsible for destroying and bringing out everything that can harm a person.
If the cleaning function fails, dirt may begin to come out through the skin. This is how various inflammations, acne, redness, and rashes form. In addition, there is additional pressure on the liver, intestines and kidneys. But that's not the worst thing.
With severe disorders, all toxins not only remain inside, but are carried through the blood throughout the body. And this is already fraught with serious consequences.
Just about the complex: why do we need the lymphatic system?
Much that seems self-evident today was not always so. The gradual accumulation of knowledge in any field was sometimes the result of specially planned, thoughtful experiments, and sometimes simply chance or human observation.
How did you search for the “milky way”? History of the discovery of the lymphatic system
People have long known about the presence of blood vessels in animals. Despite the fact that the first harmonious and consistent explanation of the circulatory system was made only in the 17th century, some idea of its role appeared among humanity long before that.
William Harvey vs. Claudius Galen: how was the human circulatory system discovered? Find out here
At the same time, there were also plenty of mysteries. The ancient Greek physician Erasistratus, who lived in the 3rd century BC, noticed that in goats that were sacrificed, it was not blood flowing from some vessels, but a whitish liquid reminiscent of milk.
At first these white vessels were called “milky ways”. The largest of them is the so-called thoracic lymphatic duct. Around the middle of the 16th century, the Italian anatomist Bartolomeo Eustachius first identified this duct on the corpse of a horse. Apparently, the scientist himself did not realize the significance of his discovery, giving this structure the name “white thoracic vein.” Smaller lymphatic vessels and capillaries are transparent, so they are difficult to see during a routine anatomical examination.
Later, another researcher, Gaspare Azelli, establishes that the contents of vessels then still incomprehensible to science are formed in the intestines; lymph accumulates in the lymph nodes of the mesentery and moves through the vessels to the liver, i.e. represents "white blood". As might be expected, this discovery was met with disbelief. Even Harvey himself likened lymphatic vessels to veins.
With the invention of the microscope, the situation in morphological studies changed dramatically. In the 40s of the 18th century, German anatomist Johann Lieberkühn discovered the initial sections of the lymphatic channel - capillaries - in the intestinal villi.
What is known about this once mysterious part of the body today?
Lymphatic system in questions and answers
What is the lymphatic system?
In the process of blood circulation, arterial blood, passing through tissues and organs, delivers oxygen and nutrients to them. In turn, they “give” various metabolic products into the blood, which, already in the venous blood, go towards the heart.
Along with the blood vessels themselves, the so-called lymphatic system is found in various parts of the body (with some exceptions). It is part of the vascular system. It consists of lymphatic capillaries, small and large lymphatic vessels, as well as lymph nodes (lymph nodes) located along their course.
Lymph formation: what is it and how does it happen?
Various substances brought by arterial blood must reach their “targets” - tissues and organs. Here, among other things, fluid is filtered through the capillary wall into the intercellular space and tissue fluid is formed. Cells receive nutrients from it and excrete waste products here.
Next, the tissue fluid enters the lymphatic vessels, nodes, is enriched with lymphocytes and turns into lymph. Lymph is also the name given to the fluid circulating in the lymphatic system.
Lymph moves through lymphatic vessels in one direction - from the periphery to the center. In this it is helped by contractions of the muscles between which the lymphatic vessels lie, as well as the valves present in the lumen of the vessels.
Why do we need lymph nodes? What happens if the lymphatic system fails?
Are your tonsils inflamed? Did a splinter in your finger cause suppuration? What do lymph nodes have to do with this?
As it turned out, the most direct thing is related to the functions of the lymphatic system.
When pathogenic microorganisms (bacteria, viruses) penetrate into one place or another in the human body, after some time they themselves and parts of the cells destroyed by them enter the lymph nodes through the lymphatic vessels.
Here they are neutralized by special cells - macrophages, which capture and “digest” them.
In addition, cells of the immune system - lymphocytes and plasma cells - are formed in the lymph nodes, and antibodies are synthesized.
Thus, lymph nodes are a kind of “filter” on the path of various potentially dangerous microorganisms and substances. The lymph purified in this way, moving through all the larger lymphatic vessels, ultimately enters the venous system, i.e. into the blood.
It is easy to imagine that if the filtering, neutralizing function of the lymphatic system “breaks down,” the entire mass of harmful substances and pathogens will directly enter the blood and spread unhindered throughout the body.
How to cleanse the lymphatic system? Truth and fiction
Methods for cleansing the lymphatic system exist. These include, in particular, lymphpheresis and lymphosorption.
During lymphpheresis, a certain amount of lymph is removed from the body, followed by replenishment of lost fluid.
The resulting lymph can also be passed through special filters that retain toxic substances, after which it is returned back to the body through intravenous infusion. Components that are useful and necessary for the body, “retained” by filters, are also introduced.
These methods are used, in particular, in toxicology when there is an increased content of toxic substances in the body - both those formed during pathological processes in the body itself and those coming from outside.
Important:
To carry out such cleaning, surgery is performed to access the thoracic lymphatic duct located in the chest cavity and insert a catheter into it.
The method is used only as an auxiliary method in addition to other methods of removing toxins.
The methods of cleansing the lymphatic system using folk remedies available in open information sources are not commented on by official medicine.
Quite often, recipes for this purpose mention licorice root. In particular, it has been shown that licorice is generally not recommended for use by people with high blood pressure.
For what reasons does blood pressure increase? Therapist, cardiologist at Clinic Expert Voronezh, Kalinina Angelina Anatolyevna, tells
What to do if the lymph nodes are swollen?
There is only one answer: see a doctor immediately. You should not waste time thinking about possible “contamination” of the lymphatic system/nodes, ways to “clean” them, etc.
Diseases of the lymphatic system
Conventionally, several groups of diseases of the lymphatic system are distinguished.
Injuries. Like other organs and tissues, the lymphatic system can be injured during accidents, accidents, surgeries and other similar situations.
Developmental defects. They include insufficient development of lymphatic vessels and nodes (hypoplasia), congenital dilatation of lymphatic vessels (lymphangiectasia; also acquired), primary obliterating lymphangiopathy, lymphangiomatosis, etc.
Inflammatory diseases. These include lymphangitis (inflammation of the lymphatic vessel), regional lymphadenitis (inflammation of the lymph node/lymph nodes).
Tumors. Benign tumors of the lymphatic vessels are called lymphangiomas, and malignant tumors are called lymphangiosarcomas.
Tumors of the lymph nodes are usually malignant. These include both neoplasms emanating from the tissue of the lymph node itself, and metastases of tumors from other organs.
What symptoms should prompt you to see a doctor?
General: unusual, often unmotivated general weakness, malaise; spontaneous weight loss; loss of appetite; increase in body temperature, even to small numbers; sweating
Local - from the lymph nodes: increase in size; soreness; compaction; decreased mobility, “soldering” them together; changes in the skin over the “problem” lymph node.
What matters is the increase in volume of one or another limb, its swelling.
You should consult a doctor if there is even one manifestation - for example, with a painless enlargement of the lymph node.
Where to run?
Any symptoms from the lymphatic system require mandatory consultation with a medical specialist. What kind of doctor treats diseases of the lymphatic system?
Since it is initially unknown what the cause of changes in a person’s lymph nodes is, it is advisable to first contact a pediatrician or therapist (depending on the patient’s age).
You can make an appointment with a therapist here
Please note: consultations are not available in all cities
Since the diseases in which manifestations of the lymph nodes are detected are different in nature, additional studies may be prescribed, as well as consultations with related specialists. You may be referred to an infectious disease specialist, TB specialist, oncologist, hematologist, or surgeon.
To clarify the diagnosis, methods such as ultrasound, CT, MRI, etc. can be used; puncture, biopsy, and removal of a lymph node for subsequent microscopic examination; lymphography.
You might be interested in:
Is it possible to cleanse the liver?
Vegetarianism: pros and cons
How to cleanse the lymphatic system? Truth and fiction
To get rid of excess liquid and remove all toxins, mechanical cleaning is necessary. Everything is safe and very easy. The best remedy is licorice. It must be taken together with enterosgel or activated carbon.
Licorice liquefies the lymph, which speeds up the removal of toxins. And activated carbon prevents them from being absorbed back into the cell.
In addition, licorice has a whole complex of essential oils and vitamins that provide an anti-inflammatory effect.
This cleaning is carried out over two weeks. And if you regularly do drainage massage and gymnastics, the effect will become most noticeable.
Lymphatic drainage massage
Drybrushing is a massage with a dry brush. It not only saves from cellulite, but also disperses lymph, removes swelling and improves blood circulation. Beauty 365 has a good brush.
Vacuum massage with miracle cans is also very good - swelling goes away, intercellular fluid accelerates and waste and toxins are eliminated faster. Choose what you like best.
Healthy foods for lymph
- Walnuts - thanks to phytoncide, protective properties increase.
- Carrots - beta-carotene, which is contained in huge quantities in this vegetable, slows down aging, helps produce antibodies and prevents lymphocytes from being destroyed.
- Sea kale - iodine also increases the protective properties of lymph.
- Eggs - they contain lutein, which is involved in the formation of building material for our cells.
- Fatty fish - the right fats make blood vessels healthy and elastic.
And now a little about those foods whose consumption should be limited:
- Alcohol causes vasospasm, and it disrupts the movement of fluid through the vessels.
- Salt – large amounts of salt cause hypertension.
- Canned food, sausages and other semi-finished products are food waste for humans. They cause clogging of our internal filters, which provokes the formation of stagnation and swelling.