Systematization of manifestations of aortic aneurysm
Currently, there is no unified approach to systematizing the manifestations of peritoneal aortic aneurysm. Most often, doctors and authors of medical works use the method of A. Pokrovsky and R. Ermolyuk, according to which aneurysms are divided:
- by etiology
– acquired (non-inflammatory or inflammatory) and congenital; - according to morphology
- into false (traumatic origin), true and stratifying; - by shape
- diffusion and saccular; - according to the course of the clinical process
- into diseases with an uncomplicated course, complicated and dissecting; - by type and location
- on the proximal segment of the peritoneal aorta, on the infrarenal section, as well as with total damage to the entire section of the abdominal aorta.
According to medical statistics, up to 95% of aneurysms are localized in the infrarenal region.
Causes of development of abdominal aortic aneurysm
- atherosclerosis, in which the appearance of cholesterol plaques on the wall of the aorta gradually reduces its strength, which contributes to protrusion in one of the areas;
- congenital predisposition, transmitted through the male line, confirmed by many years of observations: the presence of an aneurysm in the father indicates a 50% chance of this disease occurring in his son;
- an inflammatory process of a chronic, sluggish nature that occurs in the aortic wall itself or in the adipose tissue that surrounds the vessel;
- traumatic damage to the wall due to trauma or injury to the abdomen, surgery or endovascular intervention.
Atherosclerotic manifestations become the cause in 85-90% of cases of the development of acquired aneurysm in the abdominal aorta. Signs of predisposition to the development of the disease are smoking, arterial hypertension and chronic pulmonary diseases.
Symptoms of aortic aneurysm
In approximately a quarter of cases, an abdominal aortic aneurysm develops completely asymptomatically and is discovered by chance during an ultrasound or x-ray examination of the abdominal cavity. If the disease is not detected in time, there is a high probability of a sudden rupture of the aneurysm, which is externally accompanied by sudden pallor and loss of consciousness. The life of a patient with a ruptured aneurysm depends on how quickly he is taken to the hospital and placed on the operating table.
However, the asymptomatic course of the disease is not very common. As a rule, the development of an abdominal aortic aneurysm is indicated by:
- dull, aching pain in the epigastrium (in the upper abdomen) and mesogastrium (near the navel), often acquiring the character of attacks and even radiating to the lower back;
- a pulsating sensation reminiscent of a heartbeat and felt in the epigastric or mesogastric area.
These symptoms appear individually or in combination, depending on the type of aneurysm.
Who is in more danger?
- Age - 50-79 years
- Gender – male (3 times more often)
- Smoking (increases risk 4-5 times)
- Patients with uncontrolled arterial hypertension (high blood pressure);
- Overweight patients;
- Patients with atherosclerotic lesions of blood vessels supplying the brain;
- Patients with impaired blood cholesterol metabolism (dyslipidemia);
- Patients whose relatives also had an aneurysm (the risk is doubled).
Men who smoke in adulthood are at greatest risk (statistically, every 10 have an aneurysm).
Why is the procedure necessary?
This intervention helps prevent such a dangerous phenomenon as aneurysm rupture. If you ignore timely treatment, this can lead to death. According to statistics, in 40 out of 100 patients, rupture occurs during the first year of illness.
Consequently, resection saves lives and protects against various complications. In particular:
- prevents digestive tract disorders;
- relieves portal hypertension syndrome;
- prevents organic changes in the digestive system;
- does not allow intestinal ischemia to occur, etc.
Signs of RUPTURE of an abdominal aortic aneurysm:
- The appearance of abdominal pain, or a change (intensification) of pre-existing pain;
- The appearance of pain in the lower back, radiating to the groin, thighs, genitals;
- Possible clinical picture of myocardial infarction;
- Hypotension;
- Enlargement of a pre-existing pulsating mass in the abdominal cavity;
- Anemia;
- Possible bloody vomiting, etc.
More than 70 percent of patients with complicated abdominal aortic aneurysms were misdiagnosed during hospitalization.
Diagnostics
Sometimes a doctor may suspect a pathology by feeling the patient’s stomach in order to check the condition of his stomach or intestines. Often, an abdominal aortic aneurysm is detected on an x-ray or angiogram when contrast diagnostics of the digestive system or kidneys is performed. In addition, expansion of the aortic walls can be seen during echo scanning, computed tomography and magnetic resonance imaging. Even if doctors are sometimes baffled by unexpected diagnostic results aimed at completely different goals, let alone attempts at self-diagnosis - they are absolutely ineffective. Especially when the abdominal aortic aneurysm is asymptomatic.
If you suspect an abdominal aortic aneurysm, your doctor may:
- analysis of patient complaints: when signs of aneurysm appeared and how they developed;
- analysis of risk factors: does the patient use tobacco, what is his lifestyle;
- checking the family history: whether the patient’s relatives have been diagnosed with similar diseases;
- a thorough examination: what is the level of pressure, are there any signs of atherosclerosis, heart murmurs, pulmonary rales;
- general blood test: what is the cause of the disease, are there any complications;
- biochemical blood test: what is the level of cholesterol and glucose (to assess the risk of developing atherosclerosis);
- urine test: whether kidney disease is excluded;
- ultrasound diagnostics of the abdominal cavity: what is the location and size of the aneurysm;
- radiography (for a large aneurysm);
- computed tomography: what is the longitudinal and transverse size of the expansion of the aortic wall;
- magnetic resonance scanning: what is the type of aneurysm, its extent, exact location;
- color Doppler ultrasound (will give the same data as MRI, plus it will allow you to assess the speed of blood flow).
All these modern methods are good in their own way. The doctor will tell the doctor which one to choose, the patient’s condition, his age and the presence of contraindications. For example, an MRI cannot be performed if a person uses a pacemaker.
Abdominal aortic aneurysm - main diagnostic methods:
- Physical examination - includes palpation of the abdomen, percussion, i.e. tapping, listening to the peritoneum using a phonendoscope, measuring pulse and blood pressure.
- Laboratory tests of physiological fluids - urine and blood. They help diagnose and determine the cause of the aneurysm.
- Duplex ultrasound examination is the “gold standard” for screening patients (detection and follow-up);
- CT angiography is the “gold standard” of preoperative examination and in cases where information from ultrasound scanning is insufficient;
- X-ray of the abdominal organs;
- Contrast-enhanced MRI angiography;
- X-ray contrast aortography.
Treatment tactics for abdominal aortic aneurysm
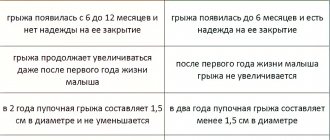
- If the size of the aortic aneurysm is less than 5.0 cm in diameter, the patient needs correction of risk factors under the dynamic supervision of a cardiologist, cardiovascular surgeon, and regular monitoring studies;
- If the size of the aortic aneurysm is ≥ 5.0 cm, then the patient requires surgical treatment to eliminate the risk of aneurysm rupture and other life-threatening complications.
- If the aneurysm is more than 3.0 cm and its size increases ≥ 6 mm per year, then the patient also needs surgical treatment.
An established diagnosis of an abdominal aortic aneurysm is an indication for surgery (at any age).
Contraindications for surgery:
- acute disorders of coronary and cerebral circulation with severe neurological deficits,
- circulatory failure stage IIB-III.
Pathogenesis
The picture of the disease unfolds gradually - day by day, month by month. Blood flow in the abdominal aorta decreases, the elastic frame of its wall is disrupted. It is noteworthy that the anterior wall of the aneurysm contains many collagen and elastin fibers. The side walls, as well as the back wall, are much thinner and more fragile. And since “where it’s thin, it ruptures,” aneurysm ruptures most often occur in the retroperitoneal area. The larger the size of the aneurysm itself, the higher, of course, the risk of rupture.
Important!
- A myocardial infarction suffered 3 months ago - with stable ECG readings, as well as a stroke - in the absence of a pronounced neurological deficit are not a contraindication to surgery.
- If there is severe coronary insufficiency, then coronary angiography is performed and the state of coronary blood flow is determined to decide on the priority implementation of coronary revascularization.
Abdominal aortic aneurysm surgery
Abdominal aorta replacement
This is a standard open surgical procedure. In our Center, this operation is performed through a mini-access - an incision on the abdominal wall 5-7 cm long (while in the standard version the incision is 15-20 cm long). After processing the surgical field and preparing a vascular prosthesis of the required length for the time required for the operation, the abdominal aorta is clamped above and below the aneurysm. The aneurysm is excised and a prepared vascular graft is sewn in place of the removed area. After checking the tightness of the seams and installing drains, the wound is sutured.
At the Clinic of High Medical Technologies named after. N.I. Pirogov St. Petersburg State University in the treatment of an aneurysm of the abdominal aorta uses vascular prostheses impregnated with silver, which differ from conventional ones in being particularly resistant to infection. The operations last on average 3-4 hours, after which the patient is transferred to the intensive care unit for observation. In the standard course of the early postoperative period, the next morning the patient is transferred to the ward of the specialized department. The total length of hospitalization for such patients is about 7 days.
It should be noted that there are various forms of the disease that complicate the standard course of treatment, which in some cases may require longer hospitalization.
Aortic endoprosthetics
- A more modern method of treating abdominal aortic aneurysm, related to hybrid surgery. This method combines open surgical technologies with endovascular ones; it represents the replacement of an aneurysmally dilated section of the aorta from the inside using a special prosthesis, made in most cases “to order” (this explains its high cost). The vascular prosthesis is specially placed in the delivery system. It is straightened directly into the cavity of the aneurysm, under the control of an X-ray machine. Thus, the prosthesis eliminates the impact of systemic arterial blood flow on the weak, stretched walls of the aorta.
This method allows you to achieve results comparable to the open surgical technique, only with fewer complications, reducing the length of hospitalization and rehabilitation of the patient by 2 times! The use of this modern method is limited only by some anatomical parameters of the aorta itself and the high cost of the endoprosthesis.
Complications during aortic surgery
Open surgery has a greater risk of early postoperative complications and mortality than endovascular aortic stent graft placement. Mortality after open surgery is about 5%, while after endoprosthetics it is 0.5%.
Other possible complications after resection of an aortic aneurysm:
- Acute renal failure
- Spinal cord stroke with leg paralysis
- High intermittent claudication (pain in the buttocks when walking) claudication
- Colon ischemia
- Embolism of the lower extremities with acute ischemia
- Bleeding from the surgical site and hemorrhagic shock
- Suppuration of the vascular prosthesis
These complications are quite rare. In our clinic, isolated cases of such complications were observed.
Prognosis and prevention
Unfortunately, abdominal aortic aneurysm is one of the most insidious and unpredictable vascular pathologies, in which the probability of death exceeds 50%. Prevention and timely detection of an aneurysm are essential for a positive outcome. Quitting nicotine addiction, as well as monitoring blood pressure and taking timely measures to normalize it, helps reduce the risk of developing an aneurysm.
Technological progress is helping to reduce the number of diagnostic errors: modern research methods make it possible to identify pathology even in the absence of symptoms. Therefore, people who are at risk - smokers, hypertensive patients, elderly people, as well as those who have a high probability of developing a congenital pathology - should consult a doctor more often for a diagnostic examination. Often, patients are unaware of the development of an aneurysm until it ruptures, but then medical care may not be provided in a timely manner.
Be sure to consult a cardiac surgeon about being examined for the presence of an abdominal aortic aneurysm. Timely detection of the disease can save your life and in any case preserve your health and performance.
Anesthesia during surgery
The operation can be performed under general anesthesia or under epidural anesthesia (injection in the back). General anesthesia is required for large aneurysms extending to the level of the renal arteries or higher. General anesthesia is required for access using a wide midline laparotomy. With retroperitoneal access to the aorta, epidural anesthesia can be limited. During operations for an aneurysm, cardiac activity and blood pressure must be monitored using special equipment. For anesthesia and intensive care, a catheter must be installed in the central vein (most often the subclavian). Kidney function is assessed by the amount of urine, for this purpose a catheter is inserted into the bladder. During anesthesia, the level of central venous pressure is monitored and drugs are administered to regulate the volume of circulating blood and electrolytes. If necessary, blood and plasma transfusions are performed to replace those lost during surgery. Special dispensers administer drugs that regulate blood pressure levels. During a long operation, a hemofiltration device may be connected to eliminate possible intoxication. Anesthesia during aortic surgery is very important and the comfort of surgeons and the immediate results of surgical intervention depend on its course.