In this article, medical doctors will help you understand the symptoms of stroke and micro-stroke and tell you what to do if a person has an attack.
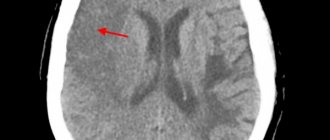
A stroke is a cerebrovascular accident that causes a blood vessel to become blocked or ruptured when a blood clot disrupts the flow of blood to the brain. Brain cells die from lack of nutrition and oxygen, which leads to impaired speech, cognitive and motor functions. If a person does not receive timely assistance, death occurs within 2–3 hours.
Symptoms of a stroke
- Sudden clouding of consciousness. Slurred thoughts, confusion and delirium of speech, difficulty understanding speech.
- Vision problems - blind spots, blurred vision.
- Impaired coordination and balance. The gait may look strange, as if the person has weakness in one or both legs, difficulty moving in space, lost, or dizzy.
- Facial asymmetry: one side of the face relaxes, a person cannot smile from both corners of the mouth.
- Weakness in arm and leg on one side. Ask the person to raise both arms straight in front of them and to the sides.
- A sharp, severe headache for no apparent reason.
A stroke develops quickly. A person himself can identify symptoms within a minute and call for help. If you see the above symptoms in a person near you, immediately call an ambulance and provide first aid.
Speech rehabilitation
To restore speech skills, the patient will need to consult a speech therapist, who will prescribe exercises for training facial muscles, language, as well as help and certain behavior from loved ones.
The patient's relatives should constantly communicate with him, while pronouncing words slowly and clearly, avoiding complex long sentences. The patient must first train the pronunciation of individual sounds, gradually moving on to syllables and words. Sometimes it is easier for a person to pronounce words in a sing-song manner than in the usual way.
Recommended exercises:
- stretch out your lips like a tube and “bar your teeth”;
- lick and lightly bite lips;
- stick your tongue out of your mouth, stroke your cheeks with your tongue, “click” your tongue;
- puff out one's cheeks;
- smile, trying to use both sides of the mouth symmetrically.
Symptoms of a microstroke
- Sharp and severe headache.
- Sudden memory loss, difficulty understanding and constructing speech.
- Loss of balance and coordination.
- Numbness in an arm or leg, numbness in one part of the face.
- Severe sound and photophobia.
In case of a micro-stroke, a person can be helped within 4 hours. It is necessary to seek help as soon as possible - either go to the vascular center or call an ambulance.
65% of patients subsequently develop a full-fledged stroke after a mini-stroke, so it is necessary to promptly treat and restore normal blood circulation in the brain.
Restoring everyday skills
All everyday skills should be developed under the supervision of a loved one, an assistant who will control the patient’s movements and, if necessary, support and guide his hand.
Nutrition
To prevent spoons and forks from slipping out of the patient’s hand, you can wrap their handles with thin foam rubber. If paralysis/paresis affects the leading hand, then when eating, you should help the patient - support and guide his hand towards the mouth.
Using the tap and washing your face
A chair should be placed in front of the sink so that the patient can wash while sitting. He should open the tap with the affected hand and, if necessary, should be assisted by guiding his hand towards the tap. In this case, the patient should check the temperature of the water with a healthy hand with preserved sensitivity. Once a comfortable temperature has been established, the patient should attempt to wash the affected hand.
Combing
You should choose combs made from non-slip materials, or wrap the comb handle with thin foam rubber. If possible, you should try to comb your hair with the hand with impaired function.
Dressing
Clothes (jacket, shirt) should be loose, fastened with buttons. It is placed on the knees, between which the sleeve for the affected arm is lightly fixed. With the help of the healthy one, she gradually moves into the sleeve.
What to do if a person has a stroke?
- First of all, call an ambulance. Sometimes the minutes count.
- Provide fresh air, open windows and doors, and free the person’s neck from constricting clothing.
- Leave the person where the attack occurred. The patient cannot be moved.
- Elevate the person's head and upper body 30 degrees by placing several pillows under the thoracic spine.
- If vomiting occurs, turn the person's head to the side and ensure that the vomit passes away so that the person does not suffocate.
- In the event of an epileptic attack, carefully hold the person, turn his head to the side and insert an object wrapped in cloth into his mouth - a stick, a comb, a spoon.
- In case of cardiac arrest, immediately begin compressions through the chest and perform artificial respiration.
- Wait for the ambulance.
Diet
Diet for stroke
- Efficacy: therapeutic effect after 1 month
- Timing: constantly
- Cost of food: 1700-1900 rubles per week
In cases of high blood pressure and hyperlipidemia, dietary restrictions on table salt and fats are indicated. cholesterol increases to more than 6.5 mmol/l, and the level of high-density lipoproteins decreases to less than 0.9 mmol/l, it is necessary to adhere to a more strict diet with a reduction in fat to 20% of the daily calorie intake. For atherosclerotic lesions, a very low-fat diet and a cholesterol intake of no more than 5 mg per day are used. At the same time, fiber is introduced into the diet - vegetables, fruits, dried fruits, bran. If a strict diet fails to reduce cholesterol levels within 6 months, antihyperlipidemic drugs are recommended.
Dangerous age and consequences of stroke
After age 55, the risk of stroke increases significantly. For men, the most dangerous age is considered to be from 45 to 55 years, since during this period they have a stroke 2 times more often than women.
If a person can be saved, the stroke still does not go away without leaving a trace. The person may be left partially paralyzed and lose control of urination and bowel movements. Cognitive functions decrease—problems with memory, speech, and information perception appear.
Recovery after a stroke is possible, but it often requires a lot of time and effort from both the patient and his loved ones. Therefore, it is better to prevent a stroke than to deal with its consequences later.
General rules of care
The recovery period after a stroke is divided into early (up to 6 months), late (6-12 months) and residual effects (after 1 year). Ideally, in the early recovery period, the patient is recommended to be treated in palliative hospitals, sanatoriums, in the late recovery period and during the period of residual effects - in a day hospital, rehabilitation department, or by a visiting team at home. In reality, most often patients are at home after an acute period of stroke, and the main question that arises among their loved ones is where to begin rehabilitation. One of the main tasks of the rehabilitation process is to create comfortable conditions that promote relief and speedy recovery.
Preparing the premises
To exclude the impact of external traumatic factors (light, sound, temperature stimuli) on the patient’s psyche, he should be placed in a bright, well-ventilated room, where no extraneous noise can be heard from the street. The room should maintain a comfortable temperature within +18-22 °C.
The room should not be cluttered with furniture or objects that are easily moved out of place. A good alternative to a regular bed would be a functional one - with adjustable height and backrest position, side rails, and lockable wheels. Near the bed you need to place a bedside table with hygiene items, a blood pressure monitor, other necessary things, a wheelchair or other mobility aids (walkers, canes), a portable toilet or a bedpan.
If the person caring for the patient is not always with him, you can equip the room with a call button that the patient can easily reach, or replace it with a regular bell. Patients who can move independently or are beginning to train the skill of walking will find handrails along the walls very useful, and anti-slip mats in the bathroom will prevent injuries.
Body hygiene and bedsore prevention
Adequate prevention of bedsores can prevent their occurrence in 80% of cases.
Preventive measures:
- a special anti-bedsore or foam mattress with a thickness of at least 10 cm;
- soft bed linen without wrinkles;
- special cushions or pads made of foam rubber for vulnerable parts of the body (back of the head, shoulder blades, elbows, sacrum, heels, ankles);
- changing body position every 2-3 hours;
- comfortable underwear;
- prevention of skin trauma - carefully moving or turning over the patient.
It is important to carry out proper hygiene measures and skin care. At least once a day, during hygienic procedures, you should examine the entire surface of the patient’s body, vulnerable areas - every time you turn over. You should use waterproof diapers and diapers and change them as needed. It is necessary to wash the patient with warm water without soap after each bowel movement, washing with soap - no more than once a day, it is better to use liquid soap. After washing, the skin is thoroughly dried with a soft towel. For dry skin, moisturizing and nourishing creams are used; for diaper rash, powders without talc are used.
Nutrition
Food should be comfortable to swallow and easily digestible. The patient needs a sufficient amount of fluid - at least 1.5 liters. in the absence of restrictions. Drinking should not be limited even with urinary incontinence, since with a lack of fluid, urine becomes concentrated and irritates the skin.
The patient's diet should contain a sufficient amount of protein. It can be a soufflé, minced chicken, beef, rabbit, or fish. Patients who have difficulty chewing or swallowing semi-solid foods may be given meat or fish broth.
The menu should include dishes rich in vitamin C, iron, zinc, fermented milk products, fruits and vegetables.
Food is prepared boiled or baked and must be freshly prepared. You should not eat fried foods, pickles, smoked foods, spicy foods, canned food, fast food, carbonated and sweet drinks. You need to eat 4-5 times a day, in small portions.
How to avoid stroke and mini-stroke?
Stroke and its precursor, microstroke, are most often caused by features of a person’s lifestyle. The risk of developing an attack increases:
- Hypertension.
- High cholesterol.
- Diabetes.
- Overweight.
- Smoking, drinking alcohol and drugs.
- Cardiovascular diseases.
- Atherosclerosis of cerebral vessels.
This can be avoided if you undergo preventive examinations on time, treat chronic diseases and modify your lifestyle. Giving up bad habits, losing weight and maintaining normal blood pressure are the three main steps towards healthy blood vessels.
At the medical level, you can visit a general practitioner, cardiologist and neurologist, as well as undergo a Holter study and 24-hour blood pressure monitoring. If you are already worried about health problems, do not expect a miracle - consult a doctor to avoid serious consequences.
Call the number listed on the website and make an appointment with a doctor today!
Pathogenesis
The key point in the pathogenesis of this condition is reversible cerebral ischemia, which occurs when there is a mismatch between the needs of the brain and the currently existing blood supply. Local anemia of brain tissue develops when perfusion decreases below 18-22 ml of blood per 100 g/min.
A transient drop in blood flow, due to various reasons, causes the development of ischemia in the brain tissue and is accompanied by reversible focal symptoms. The main pathogenetic mechanisms for the development of transient disorders are: microembolism ; hypotonic and hypertensive crisis , pathological tortuosity of the main vessels of the brain, as well as disorders of the anticoagulation system of the blood.
The outcome of ischemic cerebral circulatory disorders is determined by the caliber of the artery, the rate of development of blockage, localization, and the development of collateral circulation. If cerebral perfusion is restored, regression of symptoms is observed and the episode of transient ischemic attack ends. In the event of a further drop in blood supply to 8-10 ml per 100 g/min, which causes irreversible changes in brain tissue, cerebral infarction ( ischemic stroke ) develops.
List of sources
- Gusev E.I., Skvortsova V.I. Cerebral ischemia. 2001, 327 pp., p. 6.
- Gudkova V.V., Meshkova K.S., Volkova A.V., Stakhovskaya L.V. Transient ischemic attack. Issues of diagnosis, treatment and prevention. Zemstvo doctor. 2013;3(20):18-21.
- Parfenov V.A., Ragimov S.K. Prognosis for transient ischemic attacks based on the results of one-year observation. Neurol. magazine. 2011; 2:23–26.
- Piradov M.A., Rumyantseva S.A. Neuroprotective therapy in angioneurology. Russian medical journal. 2005; 13: 980-983.
- Fedin A.I., Rumyantseva S.A. Antioxidant therapy for cerebrovascular disorders. Treatment of nervous diseases. 2001; 2: 7-12.