The historical name for this condition is apoplexy. This is what the Roman surgeon Galen called a hemorrhagic stroke, denoting the main external signs of the disease - a sudden loss of consciousness, after which the person changed forever. Today, doctors know for sure that a vessel ruptures in the cranial cavity, blood flows out, after which up to 70% of patients die. However, the development of neuroimaging technologies, as well as the capabilities of neurosurgery, lead to the fact that the number of deaths from stroke is decreasing, and in some cases, rehabilitation sufficient for a good life is possible.
Why do blood vessels rupture?
The main cause is arterial hypertension, especially if untreated or during breaks in taking antihypertensive drugs. The vessels physically cannot withstand the pressure that blood exerts on their walls. A vessel breaks through at the site of thinning or damage, this happens in the presence of an atherosclerotic plaque, congenital aneurysms, head injuries, the use of certain medications that prevent blood clotting, tumors and encephalitis. Another important cause of rupture is arteriovenous malformations, when small arterial and venous vessels do not end in capillaries, but are intertwined into one large ball. Such congenital pathology can be detected during a preventive examination. If a person knows about it, he behaves more carefully and avoids unnecessary risks.
Nature has protected the brain as much as possible from damage, providing it with a mass of protective and backup systems. At a young age they work, but in the second half of life they don’t always work. Therefore, it is advisable that people at risk undergo an annual examination by a neurologist.
At CELT you can get advice from a neurologist.
- Initial consultation – 4,000
- Repeated consultation – 2,500
Make an appointment
The following people are at high risk of developing hemorrhagic stroke:
- hypertensive patients, they need to take medications daily;
- overweight people - the body grows approximately 1 kilometer of blood vessels per 1 kg of excess weight;
- people with high levels of cholesterol, namely low-density lipoproteins, which form atherosclerotic plaques on the vascular wall;
- people who eat insufficient amounts of protein and do not have the “building material” for complete tissue repair;
- those under chronic stress, often suffering from physical or emotional stress;
- alcohol abusers and smokers;
- those suffering from diabetes or heart disease;
- suffering from chronic infections that destroy the vascular wall - lupus erythematosus, vasculitis;
- people who constantly take medications to reduce blood viscosity;
- having direct relatives who died from cerebral hemorrhage.
Left-hand side
If the left side is affected, the consequences are characterized by disruption of the right side of the body. The patient experiences complete or partial paralysis, and not only the leg and arm are affected, but also half of the tongue and larynx. Such patients develop gait disturbances and a characteristic posture of the right hand (folded in a boat).
The victim experiences deterioration in memory and speech, and the ability to clearly express thoughts is impaired. Damage to the left hemisphere of the brain is characterized by problems with recognizing time sequences; it cannot decompose complex elements into components. Impairments in written and oral speech appear.
How does a hemorrhagic stroke occur?
Vascular rupture can occur at any time of the day. This is usually preceded by physical or emotional stress. The person suddenly falls, sometimes with a loud cry, and loses consciousness.
Approximately 30% of patients have warning signs that develop within a few minutes to several days. On the eve of a rupture of blood vessels, there may be severe headaches - ones that the person has never experienced. There is a feeling of a rush and a sharp reddening of the face. Sometimes the sensations of numbness in the limbs, muscle weakness, and facial asymmetry appear.
The main symptoms of hemorrhagic stroke are:
| Contralateral hemiplegia | The nerve pathways intersect, so the paralysis is located on the side opposite to the hemorrhage. During a stroke, the left arm and leg stop moving in the right hemisphere, and the right ones in the left hemisphere. |
| Contralateral hemianesthesia | In paralyzed limbs, sensitivity disappears on the side opposite to the rupture. |
| Aphasia | Loss of speech occurs when the dominant (dominant) hemisphere is damaged. For right-handers - right, for left-handers - left. |
| Spatial hemiagnosia with damage to the non-dominant hemisphere | If a right-hander's left hemisphere is affected, and a left-hander's right hemisphere is affected, then the person behaves as if half of the real space does not exist for him. A person does not realize that he has two halves of the body, that food can be eaten from the entire plate, and not from half. Half of everything that is located around a person is not perceived by him. |
| Facial asymmetry | One half of the face does not receive innervation and cannot contract. One nasolabial fold is smoothed out, the smile becomes one-sided, the tongue deviates to one side, water and food flow out of the mouth. |
From the moment these symptoms appear, there is only 3 hours to help the person as much as possible. After 3 (sometimes 6) hours, irreversible changes will occur, then nothing can be corrected.
Statistics facts from reliable sources
In the general structure of all types of strokes, hemorrhagic strokes account for 10%-15%. The frequency of its spread among the world population is about 20 cases per 100 thousand people. Experts, based on annual dynamics, report that in about 50 years all these indicators will double. Specifically in the Russian Federation, about 43,000-44,000 cases of HI are diagnosed annually. What is noteworthy is that it occurs approximately 1.5 times more often in men, but the mortality rate from its consequences predominates in women.
According to clinical observations, with this diagnosis, death occurs in 75% of people who are on mechanical ventilation, and in 25% of people who do not need it. Consolidated studies have shown that on average 30%-50% of patients die within 1 month from the moment of an attack of hemorrhage, and 1/2 of them die within the first 2 days. Disability (due to paralysis of the face and limbs, aphasia, blindness, etc.) among surviving patients reaches 75%, of which 10% remain bedridden. And only 25% of patients are independent in everyday life after 6 months.
Pathology represents a huge social problem, since the epidemiological peak occurs in working years - 40-60 years. Hemorrhagic strokes have become significantly “younger”; today they are quite common even among the youth group of people (20-30 years old). The risk category definitely includes people suffering from arterial hypertension, since in most cases this kind of hemorrhage occurs precisely because of chronically elevated blood pressure.
The primary factor that influences the prognosis of outcome is the promptness of providing adequate medical care to the patient.
Our doctors
Belikov Alexander Valerievich
Neurologist, Candidate of Medical Sciences
21 years of experience
Make an appointment
Novikova Larisa Vaganovna
Neuropathologist, Candidate of Medical Sciences, doctor of the highest category
Experience 39 years
Make an appointment
Pankov Alexander Rostislavovich
Neurologist
40 years of experience
Make an appointment
Direct surgical removal of hematoma
| Direct surgical removal of hematoma |
Direct surgical intervention is used for subcortical hematomas of medium and large sizes, for large hematomas of lateral or mixed localization, accompanied by increasing edema and dislocation of the brain, deteriorating condition of the patient, for cerebellar hematomas. The operation consists of removing the hematoma by encephalotomy, aspiration of blood, removing dense clots with fenestrated tweezers and washing the wound with saline solution. After removing the hematoma, it is necessary to examine its walls and perform thorough hemostasis using coagulation and hemostatic agents. Better results can be achieved by using microsurgical techniques, which can significantly reduce the size of the encephalotomy and thereby minimize surgical brain trauma. For large VMH, accompanied by edema and dislocation of the brain, a wide osteoplastic craniectomy is performed with plastic surgery of the dura mater with periosteum or artificial materials. In case of cerebellar hematomas, it is advisable to supplement direct removal of the hematoma with the installation of external ventricular drainage.
Types of strokes
Depending on which part of the brain the hemorrhage occurred, there are 4 types of stroke:
- Intracerebral or parenchymal, when the spilled blood saturates an area of the brain. In turn, they also have their division into:
- hemispheric, when an area of the hemispheres is affected;
- subcortical, located under the cortical (gray) matter of the brain;
- hemorrhage in the cerebellum, where the balance centers are located;
- hemorrhage in the brain stem, where the respiratory center and the area that is responsible for the functioning of the heart and maintaining the pressure in the vessels necessary to support life are located.
- Subarachnoid (bleeding into the space between the meninges).
- Ventricular (hemorrhage into the ventricle of the brain).
- Mixed: ventricular-parenchymal, subarachnoid-parenchymal, parenchymal-ventricular-subarachnoid and so on.
Survival depends not only on the location of the vessel rupture, but also on how much blood was released. Small hemorrhages are considered to be those in which from 1 to 20 ml are poured out, medium - from 20 to 50 ml, large - more than 50 ml. The greater the amount of blood shed, the more severe the consequences. A stroke is almost always accompanied by disturbances in cardiac activity, breathing and swallowing, oculomotor disturbances, and changes in the size of the pupils.
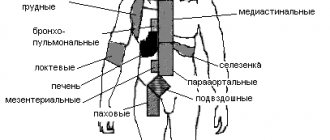
Typical location of hemorrhages
Most often, and this is about 55% of cases, hemorrhages occur in the putamental zone. Putamental bleeding occurs due to rupture of degenerated lenticulostriate arteries, which causes blood to enter the brain shell. The culprit of pathogenesis with such localization is usually long-standing hypertension. In some cases, bleeding from the putamentum breaks into the ventricular system, which is fraught with tamponade of the gastrointestinal tract and acute occlusive-hydrocephalic crisis.
The next most common location is the subcortical region (subcortical). Subcortical GIs are observed in 17%-18% of cases. As a rule, the leading sources of such hemorrhage are ruptured AVMs and aneurysms against the background of increased pressure. The subcortical zones involved in the hemorrhagic process are the frontal, parietal, occipital or temporal lobe.
The third most common place, where brain hemorrhage is determined in 14%-15% of cases, is the optic thalamus, or thalamus. Thalamic hemorrhages occur due to the release of blood from the blood vessel of the vertebrobasilar region. Pathogenesis can be associated with any etiological factor, however, as always, the involvement of hypertensive syndrome is significantly more often noted.
In fourth place (7%) in terms of frequency of development are pontine GIs. They are concentrated in the back of the brain stem, that is, in the pons. Through the bridge, the cortex communicates with the cerebellum, spinal cord and other major elements of the central nervous system. This department includes the centers for controlling breathing and heartbeat. Therefore, the bridge is the most dangerous localization of hemorrhage, practically incomparable to life.
Additional Research
MRI of the brain
- Cost: 14,000 rub.
More details
The initial diagnosis is established after examination by a neurologist, but instrumental diagnostics are always required to clarify the boundaries of the lesion. The most informative method is computed tomography, which allows a good examination of the brain matter. MRI is used for the same purpose if there is time for it.
Angiography gives excellent results, this is a study of blood vessels with contrast. It identifies malformations, dissections (dissections) and other vascular pathology. The important thing is that this study can be conducted in healthy people at risk. This is the best prevention of stroke if research is supplemented with treatment.
Lumbar puncture is used for diagnostic and therapeutic purposes.
Medical care in hospital
All patients receive intensive therapeutic care at an early stage in a neuro intensive care hospital. Initial treatment measures are aimed at:
- normalization of microcirculation, hemorheological disorders;
- relief of cerebral edema, treatment of obstructive hydrocephalus;
- correction of blood pressure, body temperature;
- functional regulation of the cardiovascular system;
- maintaining water and electrolyte balance;
- prevention of possible seizures;
- prevention of extracranial consequences of inflammatory and trophic nature (pneumonia, embolism, pulmonary edema, pyelonephritis, cachexia, DIC syndrome, endocarditis, bedsores, muscle atrophy, etc.);
- providing respiratory support (if the patient needs it);
- elimination of intracranial hypertension in HI with dislocation.
Features of treatment
Treatment of hemorrhagic stroke today is more in the purview of neurosurgeons than neurologists. The blood has already been shed, and the possibilities of medical assistance are limited. Removal of an intracerebral hematoma can save lives and maintain an acceptable level of health. Surgical removal is more successful the earlier it is performed. Optimally, the patient should be operated on on the first or, in extreme cases, on the second day after the incident.
The main intervention is aspiration (suction) of the hematoma and clipping of the aneurysm. It is only possible when the artery is in an accessible place. There is no way to help with an aneurysm deep in the medulla. In a typical case, the blood is aspirated, a clip is placed at the base of the aneurysm, and the aneurysm is isolated from the bloodstream.
Malformations are excised whenever possible. These are complex operations that require not only the skill of a specialist, but also first-class equipment.
Meningeal symptoms
Signs of irritation of the meninges can occur with parenchymal hemorrhage due to cerebral edema, but they are more characteristic of subarachnoid hemorrhage.
The most typical sign is a stiff neck, when the patient is unable to press the chin to the chest when lying down.
If the patient bends his knees while checking for rigidity, this is another sign of irritation of the meninges, which is called Brudzinski's sign.
How to help a stroke victim?
Recovery largely depends on how the people around the patient behave. First of all, you need to call an ambulance, and until it arrives, try not to move the person. You need to place a cushion or pillow under the shoulders and head, carefully turn the person on the right side, and place a basin or bag in case of vomiting. It is advisable to measure blood pressure. Anti-pressure pills should not be given before the ambulance arrives: there is a possibility of a sharp drop in blood pressure. Only specially trained medical personnel know the rules for lowering blood pressure when it rises above 150/100 mmHg. If respiratory depression occurs, you need to start resuscitation - chest compressions, mouth-to-mouth breathing.
The best prevention is timely treatment of hypertension, atherosclerosis, identification of malformations and aneurysms before they rupture.
Our neurologists see patients every day, and every patient at the clinic can find out their risk for developing a hemorrhagic stroke. Visit your doctor while you still have time.
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions
Rehabilitation objectives
The main objectives of the ongoing rehabilitation are:
- Work on restoring lost everyday and physiological functions of a person suffering from a stroke. Restoring full range of motion, the ability to independently care for oneself and perform simple household chores.
- Restoration of lost professional ability to work with a return to the previous place of activity or assistance in retraining.
- Maintaining the necessary social activity of a person, first of all, restoring his contact with loved ones and the ability to make new acquaintances;
It is very important to prevent a possible relapse and correct the patient’s current lifestyle.
Puncture-aspiration method
| Puncture removal of hematoma with administration of fibrinolytic |
It is advisable to use the puncture-aspiration method for small lateral and medial hematomas accompanied by severe neurological disorders. The method consists of puncturing the hematoma with a catheter and simultaneously evacuating the liquid part of the hematoma. For precise positioning of the catheter, it is recommended to use neuronavigation. In some cases, drainage is carried out within 24 hours. The puncture-aspiration method with the introduction of fibrinolytics is indicated for lateral and medial supratentorial hemorrhages of medium size (from 30 to 60 ml) and for cerebellar hematomas (15–30 ml) provided the patient’s condition is stable. In this case, the technique is supplemented by fractional administration of fibrinolytic drugs at certain intervals. In the case of isolated ventricular hemorrhages, external ventricular drainage is performed with fractional intraventricular administration using fibrinolytics. According to the Research Institute of Neurosurgery, this method can reduce mortality in massive IVH by up to 40%, while in the natural course of this disease it approaches 100%.
Prevention
The disease is extremely serious and dangerous. It is much easier to avoid it than to treat it later. Prevention measures include:
Blood pressure control
- proper nutrition;
- monitoring weight changes (especially when you are overweight);
- control of blood pressure, preventing its increase;
- fight against atherosclerotic phenomena;
- getting rid of bad habits - smoking, alcohol;
- If possible, avoid stress and overexertion.
To prevent relapse, restorative and vitamin preparations are prescribed. Constant supervision by a specialist is required.
Diagnostics
To accurately identify the disease and differentiate hemorrhage from ischemia, an instrumental examination is performed:
- MRI or CT scan - the images show a limited area of the hematoma. The safety of magnetic tomography allows for multiple examinations and monitoring of neuronal recovery.
- Angiography - shows the condition of blood vessels. Well displays arterial rupture, signs of atherosclerosis and congenital anomalies.
- Lumbar puncture - taking cerebrospinal fluid in the lumbar region for analysis. The diagnosis of hemorrhagic stroke is made when red blood cells are detected in the cerebrospinal fluid in high concentrations.