Flamadex, 5 pcs., 2 ml, 25 mg/ml, solution for intravenous and intramuscular administration
General types of interactions are characteristic of all NSAIDs, including dexketoprofen.
Undesirable combinations
- with other NSAIDs, including salicylates in high doses (>3 g/day): simultaneous use of several NSAIDs increases the risk of gastrointestinal bleeding and ulcers;
- oral anticoagulants, heparin in doses exceeding prophylactic ones;
- ticlopidine (increases the risk of bleeding due to inhibition of platelet aggregation and damage to the mucous membrane of the digestive tract);
- lithium preparations - NSAIDs increase the concentration of lithium in the blood plasma (decreased renal excretion of lithium), which can reach a toxic level, so the level of lithium in the blood should be monitored when prescribing, changing the dose or discontinuing dexketoprofen;
- methotrexate in high doses (at least 15 mg/week) - the toxicity of methotrexate increases due to a decrease in its renal clearance when using NSAIDs;
- GCS: increases the risk of developing ulcers and gastrointestinal bleeding;
- hydantoin derivatives and sulfonamides: the severity of their toxic manifestations may increase.
Combinations requiring caution
- with diuretics, ACE inhibitors, antibacterial drugs from the group of aminoglycosides and angiotensin II receptor antagonists. Dexketoprofen weakens the effect of diuretics and other antihypertensive drugs. Treatment with NSAIDs is associated with a risk of developing acute renal failure in patients with dehydration (decreased glomerular filtration rate due to reduced PG synthesis). When using dexketoprofen and diuretics in combination, ensure that the patient is adequately hydrated and monitor renal function before prescribing;
- methotrexate in low (less than 15 mg/week) doses - the hematological toxicity of methotrexate increases due to a decrease in its renal clearance when using NSAIDs. Blood counts should be monitored weekly during the first weeks of combination treatment. In the presence of even minor impairment of renal function, as well as in elderly people, careful monitoring is necessary;
- pentoxifylline - increases the risk of bleeding. Active clinical monitoring and frequent monitoring of bleeding time or clotting time are necessary;
- zidovudine - a toxic effect of zidovudine on reticulocytes is possible, which after the first week of NSAID use can lead to the development of severe anemia. It is necessary to count blood cells and reticulocytes 1–2 weeks after the start of combination treatment;
- oral hypoglycemic drugs - due to a possible increase in hypoglycemic effect due to the ability of NSAIDs to displace them from sites of binding to blood plasma proteins.
Combinations to consider
- with β-blockers - their antihypertensive effect may be reduced due to the inhibition of PG synthesis by NSAIDs;
- cyclosporine and tacrolimus: their nephrotoxicity may be enhanced due to the effect of NSAIDs on renal PGs. When carrying out combination therapy, it is necessary to monitor renal function;
- thrombolytic drugs - increases the risk of bleeding;
- probenecid: it is possible to increase the concentration of dexketoprofen in the blood plasma, which may be due to an inhibitory effect on tubular secretion and/or conjugation with glucuronic acid and requires dose adjustment of dexketoprofen;
- cardiac glycosides - NSAIDs can lead to an increase in their concentration in the blood plasma;
- mifepristone - due to the theoretical risk of changes in the effectiveness of mifepristone under the influence of PG synthesis inhibitors, NSAIDs should be prescribed 8-12 days after taking mifepristone;
- quinolone antibiotics: a high risk of developing seizures when using NSAIDs in combination with high doses of quinolones.
Pharmaceutical interactions
Flamadex® should not be mixed in the same syringe with a solution of dopamine, promethazine, pentazocine, pethidine or hydroxyzine (a precipitate will form).
Flamadex® can be mixed in one syringe with a solution of heparin, lidocaine, morphine and theophylline.
The prepared solution of Flamadex® for intravenous drip administration should not be mixed with promethazine or pentazocine.
The prepared solution of Flamadex® is compatible with the following injection solutions: dopamine, heparin, hydroxyzine, lidocaine, morphine, pethidine and theophylline.
Flamadex 25mg/ml 2ml 5 pcs. solution for intravenous and intramuscular administration
pharmachologic effect
NSAID, propionic acid derivative.
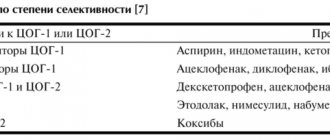
It has analgesic, anti-inflammatory and antipyretic effects. The mechanism of action is associated with inhibition of prostaglandin synthesis at the level of COX-1 and COX-2. The analgesic effect occurs 30 minutes after oral administration or parenteral administration. The duration of the analgesic effect after oral administration is 4-6 hours, after parenteral administration at a dose of 50 mg - about 4-8 hours.
When combined with opioid analgesics, dexketoprofen significantly (up to 30-45%) reduces the need for opioids.
Composition and release form Flamadex 25 mg/ml 2 ml 5 pcs. solution for intravenous and intramuscular administration
Solution for intravenous and intramuscular administration - 1 amp.
- Dexketoprofen (in the form of dexketoprofen trometamol) - 25 mg;
- Excipients: ethanol (ethyl alcohol 95% in terms of 100% substance) - 200 mg, sodium chloride - 8 mg, sodium disulfite - 2 mg, sodium hydroxide - up to pH 6.5-8.5, water for injection - up to 2 ml.
5 ampoules of 2 ml. in cardboard packaging.
Description of the dosage form
The solution for intravenous and intramuscular administration is transparent, colorless.
Directions for use and doses
Recommended dose for adults: 50 mg every 8-12 hours. If necessary, the drug can be re-administered at 6-hour intervals. The daily dose should not exceed 150 mg.
Flamadex is indicated for short-term use; treatment should be limited to the period of acute symptoms (no more than 2 days).
In patients with mild to moderately severe liver dysfunction (5-9 points on the Child-Pugh scale), the total daily dose should be reduced to 50 mg and frequent monitoring of liver function parameters should be carried out. Flamadex should not be prescribed to patients with severe liver dysfunction.
For patients with mild renal impairment (creatinine clearance - 30-60 ml/min), the daily dose is reduced to 50 mg. Flamadex should not be prescribed to patients with moderate to severe renal failure (creatinine clearance less than 30 ml/min).
Dose adjustment for elderly patients, as a rule, is not required, however, due to a physiological decrease in renal function, it is recommended to reduce the dose of the drug: for mild renal impairment in elderly patients, the total daily dose is 50 mg.
For parenteral administration.
Administer intramuscularly (deeply, slowly), intravenously in a stream (slowly for at least 15 seconds) or drip (10-30 minutes).
Rules for preparing a solution for intravenous infusion.
To prepare a solution of Flamadex for intravenous infusion, the contents of one ampoule (2 ml) are diluted in 30-100 ml of 0.9% sodium chloride solution, glucose solution or Ringer's solution. The solution should be prepared under aseptic conditions, protected from exposure to daylight. The prepared solution should be transparent and colorless.
Pharmacokinetics
Suction.
After oral administration of the drug, Cmax of dexketoprofen in serum in humans is achieved on average after 30 minutes (15-60 minutes). Concomitant food intake slows down the absorption of the drug. AUC values after single and repeated doses are similar, indicating the absence of drug accumulation.
After intramuscular administration of dexketoprofen, Cmax in the blood serum is achieved on average after 20 minutes (10-45 minutes). AUC after a single dose of 25-50 mg is proportional to the dose, both with IM and IV administration. The corresponding pharmacokinetic parameters are similar after single and repeated intramuscular or intravenous administration, indicating the absence of drug accumulation.
Distribution.
Dexketoprofen is characterized by a high level of binding to plasma proteins - 99%. The average Vd value is less than 0.25 l/kg, the half-life of distribution is about 0.35 hours.
Metabolism and excretion.
Metabolism of dexketoprofen mainly occurs by conjugation with glucuronic acid followed by excretion by the kidneys.
T1/2 of dexketoprofen trometamol is about 1-2.7 hours.
Pharmacokinetics in special clinical cases.
In elderly people, there is an increase in the duration of T1/2 (both after a single and after repeated IM or IV administration) on average up to 48% and a decrease in the overall clearance of the drug.
Indications for use Flamadex 25mg/ml 2ml 5 pcs. solution for intravenous and intramuscular administration
- Relief of pain syndrome of various origins (including postoperative pain, pain with bone metastases, post-traumatic pain, pain with renal colic, algomenorrhea, sciatica, sciatica, neuralgia, toothache);
- symptomatic treatment of acute and chronic inflammatory, inflammatory-degenerative and metabolic diseases of the musculoskeletal system (including rheumatoid arthritis, osteoarthritis, spondyloarthritis: ankylosing spondylitis, reactive arthritis, psoriatic arthritis).
The drug is intended for symptomatic therapy, reducing pain and inflammation at the time of use, and does not affect the progression of the disease.
Contraindications
- Hypersensitivity to dexketoprofen or other NSAIDs or to any of the excipients included in the drug (including sulfites);
- complete or incomplete combination of bronchial asthma, recurrent polyposis of the nose and paranasal sinuses and intolerance to acetylsalicylic acid or other NSAIDs (including a history);
- erosive and ulcerative lesions of the gastrointestinal tract and duodenum;
- history of gastrointestinal bleeding, other active bleeding (including suspected intracranial bleeding);
- anticoagulant therapy;
- inflammatory bowel diseases (ulcerative colitis, Crohn's disease) in the acute phase;
- severe liver dysfunction (10-15 points on the Child-Pugh scale);
- progressive kidney disease, severe renal dysfunction (creatinine clearance less than 30 ml/min);
- confirmed hyperkalemia;
- decompensated heart failure;
- period after coronary artery bypass surgery;
- hemophilia and other blood clotting disorders;
- pregnancy;
- breastfeeding period;
- children and adolescents under 18 years of age (there are no clinical data on the effectiveness and safety of the drug in pediatric practice).
Flamadex solution for IV and IM administration is contraindicated for neuraxial (epidural or intrathecal) administration due to the ethanol contained in the drug.
With caution: peptic ulcer of the stomach and duodenum, ulcerative colitis, Crohn's disease, history of liver disease, hepatic porphyria, chronic renal failure (creatinine clearance 30-60 ml/min), chronic heart failure, arterial hypertension, significant decrease in blood volume (including including after surgery), bronchial asthma, ischemic heart disease, cerebrovascular diseases, dyslipidemia/hyperlipidemia, diabetes mellitus, peripheral arterial disease, the presence of Helicobacter pylori infection, systemic connective tissue diseases, long-term use of NSAIDs, tuberculosis, severe osteoporosis, simultaneous use of corticosteroids ( including prednisolone), anticoagulants (including warfarin), antiplatelet agents (including acetylsalicylic acid, clopidogrel), selective serotonin reuptake inhibitors (including citalopram, fluoxetine, paroxetine, sertraline) , severe somatic diseases, elderly patients (including those receiving diuretics, weakened patients and those with low body weight), alcoholism, smoking.
Flamadex should be prescribed with caution to patients with a history of allergies.
Caution is required when prescribing Flamadex to patients with gastrointestinal disorders or a history of gastrointestinal diseases. If gastrointestinal bleeding or ulcers occur, therapy with Flamadex should be discontinued.
Application of Flamadex 25mg/ml 2ml 5 pcs. solution for intravenous and intramuscular administration during pregnancy and lactation
The use of Flamadex during pregnancy and lactation is contraindicated.
The use of the drug is contraindicated in children under 18 years of age.
special instructions
It has been clinically proven that the simultaneous use of dexketoprofen and low molecular weight heparin drugs in prophylactic doses in the postoperative period does not change coagulation rates. However, when using Flamadex with other drugs that affect blood clotting, careful medical monitoring of the blood clotting system is necessary. Dexketoprofen may cause reversible inhibition of platelet aggregation.
Like other NSAIDs, Flamadex can lead to an increase in creatinine concentrations and nitrogen levels in the blood plasma. Like other prostaglandin synthesis inhibitors, Flamadex can have side effects on the urinary system, which can lead to the development of glomerulonephritis, intestinal nephritis, papillary necrosis, nephrotic syndrome and acute renal failure.
As with the use of other NSAIDs, there may be a slight transient increase in some indicators of liver function, a significant increase in the activity of AST and ALT in the blood serum. At the same time, monitoring of liver and kidney functions is necessary in elderly patients. In case of a significant increase in the corresponding indicators, Flamadex should be discontinued.
Flamadex should be prescribed with caution to patients with chronic heart failure of NYHA functional class I-II.
Like other NSAIDs, Flamadex can mask the symptoms of infectious diseases. Isolated cases of exacerbation of infectious processes localized in soft tissues have been reported when using NSAIDs. Therefore, medical supervision is required for patients with signs of bacterial infection or worsening of their condition during treatment with dexketoprofen.
Each ampoule of Flamadex with solution for intravenous and intramuscular administration contains 200 mg of ethanol.
Influence on the ability to drive vehicles and operate machinery.
Due to possible dizziness and drowsiness during treatment with Flamadex, the ability to concentrate and the speed of psychomotor reactions may decrease.
Overdose
Cases of overdose have not been described.
Symptoms: possible nausea, vomiting, anorexia, abdominal pain, dizziness, disorientation, headache, drowsiness.
Treatment: symptomatic therapy; if necessary, hemodialysis.
Side effects Flamadex 25mg/ml 2ml 5 pcs. solution for intravenous and intramuscular administration
Frequency of side effects: often (1-10%), uncommon (0.1-1%), rare (0.01-0.1%), very rare (less than 0.01%, including individual reports).
From the hematopoietic system: rarely - anemia; very rarely - neutropenia, thrombocytopenia.
From the nervous system: infrequently - headache, dizziness, insomnia, drowsiness; rarely - paresthesia.
From the senses: infrequently - blurred vision; rarely - tinnitus.
From the cardiovascular system: infrequently - arterial hypotension, feeling of heat, hyperemia of the skin; rarely - extrasystole, tachycardia, arterial hypertension, peripheral edema, superficial thrombophlebitis.
From the respiratory system: rarely - bradypnea; very rarely - bronchospasm, dyspnea.
From the digestive system: often - nausea, vomiting; uncommon - abdominal pain, dyspepsia, diarrhea, constipation, hematemesis, dry mouth; rarely - erosive and ulcerative lesions of the gastrointestinal tract, including bleeding and perforation, anorexia, increased activity of liver enzymes, jaundice; very rarely - pancreatic damage, liver damage.
From the urinary system: rarely - polyuria, renal colic; very rarely - nephritis or nephrotic syndrome.
From the reproductive system: rarely - in women - menstrual irregularities, in men - dysfunction of the prostate gland.
From the musculoskeletal system: rarely - muscle spasm, difficulty moving in the joints.
From the skin: sometimes - dermatitis, rash, sweating; rarely - acne; very rarely - photosensitivity.
Allergic reactions: rarely - urticaria; very rarely - severe skin reactions (Stevens-Johnson syndrome, Lyell's syndrome), angioedema, allergic dermatitis, anaphylactic shock, facial swelling.
Metabolic disorders: rarely - hyperglycemia, hypoglycemia, hypertriglyceridemia.
From laboratory parameters: rarely - ketonuria, proteinuria.
Local and general reactions: often - pain at the injection site; uncommon - inflammatory reaction, hematoma, hemorrhage at the injection site, feeling of heat, chills, fatigue; rarely - back pain, fainting, fever.
Other: aseptic meningitis, occurring mainly in patients with systemic lupus erythematosus or mixed connective tissue diseases, hematological disorders (purpura, aplastic and hemolytic anemia, rarely - agranulocytosis and bone marrow hypoplasia).
Drug interactions
General interactions are common to all NSAIDs, including dexketoprofen.
Undesirable combinations.
With other NSAIDs, including salicylates in high doses (≥ 3 g/day) - simultaneous use of several NSAIDs increases the risk of gastrointestinal bleeding and ulcers.
With oral anticoagulants, heparin in doses exceeding prophylactic ones; with ticlopidine - the risk of bleeding increases due to inhibition of platelet aggregation and damage to the mucous membrane of the digestive tract.
With lithium preparations, NSAIDs increase the concentration of lithium in the blood plasma (decreased renal excretion of lithium), which can reach toxic levels, so the level of lithium in the blood should be monitored when prescribing, changing the dose or discontinuing dexketoprofen.
With methotrexate in high (at least 15 mg/week) doses, the toxicity of methotrexate increases due to a decrease in its renal clearance when using NSAIDs.
With GCS, the risk of developing ulcerative lesions and gastrointestinal bleeding increases.
With hydantoin derivatives and sulfonamides, the severity of their toxicity may increase.
Combinations requiring caution.
With diuretics, ACE inhibitors, antibacterial drugs from the group of aminoglycosides and angiotensin II receptor antagonists - dexketoprofen weakens the effect of diuretics and other antihypertensive drugs. Treatment with NSAIDs is associated with a risk of acute renal failure in patients with dehydration (decreased glomerular filtration rate due to decreased prostaglandin synthesis).
When using dexketoprofen and diuretics in combination, ensure that the patient is adequately hydrated and monitor renal function before prescribing.
When used simultaneously with methotrexate in low (less than 15 mg/week) doses, the hematological toxicity of methotrexate increases due to a decrease in its renal clearance when using NSAIDs. Blood counts should be monitored weekly during the first weeks of combination treatment. In the presence of even minor impairment of renal function, as well as in the elderly, careful monitoring is necessary.
When used simultaneously with pentoxifylline, the risk of bleeding increases. Active clinical monitoring and frequent monitoring of bleeding time or clotting time are necessary.
With zidovudine - the toxic effect of zidovudine on reticulocytes is possible, which after the first week of NSAID use can lead to the development of severe anemia. It is necessary to count blood cells and reticulocytes after 1-2 weeks. from the start of combination treatment.
With oral hypoglycemic drugs - due to a possible increase in hypoglycemic effect due to the ability of NSAIDs to displace them from sites of binding to blood plasma proteins.
Combinations to consider.
With beta-blockers, their antihypertensive effect may be reduced due to NSAID inhibition of prostaglandin synthesis.
With cyclosporine and tacrolimus, their nephrotoxicity may be enhanced due to the effect of NSAIDs on renal prostaglandins. When carrying out combination therapy, it is necessary to monitor renal function.
With thrombolytic drugs, the risk of bleeding increases.
With probenecid, it is possible to increase the concentration of dexketoprofen in the blood plasma, which may be due to an inhibitory effect on tubular secretion and/or conjugation with glucuronic acid and requires dose adjustment of dexketoprofen.
With cardiac glycosides - NSAIDs can lead to an increase in their concentration in the blood plasma.
With mifepristone - due to the theoretical risk of changes in the effectiveness of mifepristone under the influence of prostaglandin synthesis inhibitors. NSAIDs should be prescribed 8-12 days after taking mifepristone.
With quinolone antibiotics - there is a high risk of developing seizures when using NSAIDs in combination with high doses of quinolones.
Pharmaceutical interaction.
Flamadex cannot be mixed in the same syringe with a solution of dopamine, promethazine, pentazocine, pethidine or hydroxyzine (a precipitate is formed).
Flamadex can be mixed in one syringe with a solution of heparin, lidocaine, morphine and theophylline.
The prepared solution of Flamadex for intravenous drip administration cannot be mixed with promethazine or pentazocine.
The prepared solution of Flamadex is compatible with the following injection solutions: dopamine, heparin, hydroxyzine, lidocaine, morphine, pethidine and theophylline.
Flamadex solution for IM and IV injection 25 mg/ml 2 ml N5 (Sotex)
General interactions are common to all NSAIDs, including dexketoprofen. Undesirable combinations: - with other NSAIDs, including salicylates in high doses (≥ 3 g / day): simultaneous use of several NSAIDs increases the risk of gastrointestinal bleeding and ulcers; - with oral anticoagulants, heparin in doses exceeding prophylactic ones; - with ticlopidine (increases the risk of bleeding due to inhibition of platelet aggregation and damage to the mucous membrane of the digestive tract); - with lithium preparations - NSAIDs increase the concentration of lithium in the blood plasma (decreased renal excretion of lithium), which can reach a toxic level, so the level of lithium in the blood should be monitored when prescribing, changing the dose or discontinuing dexketoprofen; - with methotrexate in high (at least 15 mg/week) doses - the toxicity of methotrexate increases due to a decrease in its renal clearance when using NSAIDs; - with glucocorticosteroids: the risk of developing ulcers and gastrointestinal bleeding increases; - hydantoin derivatives and sulfonamides: the severity of their toxic manifestations may increase. Combinations requiring caution: - with diuretics, ACE inhibitors, antibacterial drugs from the group of aminoglycosides and angiotensin II receptor antagonists. Dexketoprofen weakens the effect of diuretics and other antihypertensive drugs. Treatment with NSAIDs is associated with a risk of acute renal failure in patients with dehydration (decreased glomerular filtration rate due to decreased prostaglandin synthesis). When using dexketoprofen and diuretics in combination, ensure that the patient is adequately hydrated and monitor renal function before prescribing; - with methotrexate in low (less than 15 mg/week) doses - the hematological toxicity of methotrexate increases due to a decrease in its renal clearance when using NSAIDs. Blood counts should be monitored weekly during the first weeks of combination treatment. In the presence of even minor impairment of renal function, as well as in elderly people, careful monitoring is necessary; - with pentoxifylline - the risk of bleeding increases. Active clinical monitoring and frequent monitoring of bleeding time or clotting time are necessary; - with zidovudine - the toxic effect of zidovudine on reticulocytes is possible, which after the first week of NSAID use can lead to the development of severe anemia. It is necessary to count blood cells and reticulocytes 1-2 weeks after the start of combination treatment; - with oral hypoglycemic drugs - due to a possible increase in hypoglycemic effect due to the ability of NSAIDs to displace them from sites of binding to blood plasma proteins; Combinations that need to be taken into account: - with beta blockers - their antihypertensive effect may be reduced due to the inhibition of prostaglandin synthesis by NSAIDs; - with cyclosporine and tacrolimus: their nephrotoxicity may be enhanced due to the effect of NSAIDs on renal prostaglandins. When carrying out combination therapy, it is necessary to monitor renal function; - with thrombolytic drugs - the risk of bleeding increases; - with probenecid: it is possible to increase the concentration of dexketoprofen in the blood plasma, which may be due to an inhibitory effect on tubular secretion and/or conjugation with glucuronic acid and requires dose adjustment of dexketoprofen; - with cardiac glycosides - NSAIDs can lead to an increase in their concentration in the blood plasma; - with mifepristone - due to the theoretical risk of changes in the effectiveness of mifepristone under the influence of prostaglandin synthesis inhibitors, NSAIDs should be prescribed 8-12 days after taking mifepristone; - quinolone antibiotics: a high risk of developing seizures when using NSAIDs in combination with high doses of quinolones. Pharmaceutical interaction. Flamadex® should not be mixed in the same syringe with a solution of dopamine, promethazine, pentazocine, pethidine or hydroxyzine (a precipitate will form). Flamadex® can be mixed in one syringe with a solution of heparin, lidocaine, morphine and theophylline. The prepared solution of Flamadex® for intravenous drip administration should not be mixed with promethazine or pentazocine. The prepared solution of Flamadex® is compatible with the following injection solutions: dopamine, heparin, hydroxyzine, lidocaine, morphine, pethidine and theophylline.