Anonymously
Around the clock
Attention! The material contains information about substances, the use of which can cause serious harm to your health!
Neuroleptics are antipsychotic drugs that are used to treat severe mental conditions such as mania, hallucinosis, or psychosis. Despite their widespread use in medical practice, tranquilizers are also used to achieve a drug “high”: this leads to the development of severe pharmaceutical dependence.
- What are neuroleptics?
- The effect of neuroleptics on the body
- Signs of antipsychotic drug use
- Side effects from antipsychotics
- Contraindications
- Types of antipsychotics
- Typical antipsychotics
- Atypical antipsychotics
- New generation neuroleptics
- The safest antipsychotic
- Neuroleptics without sedation
- List of antipsychotics
- First generation neuroleptics
- Second generation neuroleptics
- Neuroleptics of the latest generation
- Consequences of neuroleptics
- Neuroleptics and alcohol
- Antipsychotic drug poisoning
- Dyskinesia from neuroleptics
- Insomnia
- Disorders of the nervous system
- Overdose of antipsychotics
- FAQ
- When are antipsychotics prescribed?
- What is neuroleptic syndrome?
- Can you buy antipsychotics without a prescription?
- How to get off antipsychotics? Help from specialists at the Zdravnitsa clinic
Treatment prices:
| Service | Price, rub) |
| Types of therapies | |
| Standard detoxification therapy | 3 500 ₽ |
| Double Detox Therapy | 6 000 ₽ |
| Enhanced Detoxification Therapy | 7 500 ₽ |
| Maximum detoxification therapy | 9 500 ₽ |
| Quick sobering up at home | 7 500 ₽ |
| Hospital at home 1 day | 22 000 ₽ |
| Advanced hospitalization | 15 000 ₽ |
| Treatment in hospital | |
| Accommodation | |
| Economy chamber (6 beds) | 2 000 ₽ |
| Standard room (4 beds) | 3 000 ₽ |
| Increased comfort (2 seater) | 5 500 ₽ |
| VIP chamber (1 person) | 12 500 ₽ |
| Individual post 24/7 | 5 000 ₽ |
| Medical and social rehabilitation 21 days | 140 000 ₽ |
| Service | Price, rub) |
| Initial consultation with a narcologist | for free |
| Consultation with a psychologist | 3 000 ₽ |
| Psychiatrist consultation | 5 000 ₽ |
| Coding at home Torpedo | 7 500 ₽ |
| Express output and encoding (doublet) | 13 500 ₽ |
| Coding using the Dovzhenko method | 12 000 ₽ |
| Hypnosis classic session | 13 000 ₽ |
| Ericksonian hypnosis session (NLP) | 8 000 ₽ |
| Coding method Torpedo | 5 500 ₽ |
| Double block | 8 000 ₽ |
| Esperal injection for 1 year | 9 900 ₽ |
| Tetlong for 3 months | 10 500 ₽ |
| Esperal gel for 1 year | 15 000 ₽ |
| Selincro course of therapy | 12 500 ₽ |
| Implantation of Disulfiram for 1 year | 18 000 ₽ |
| Vivitrol injection for 1 month | 26 000 ₽ |
| Naltrexone stitching for 3 months | 35 000 ₽ |
| Neuroimplantation Prodetoxon for 6 months | 47 500 ₽ |
| Narcopsychotherapy session | 50 000 ₽ |
| Neutralization of encoding | specify |
| Psychodiagnostics / pathological diagnostics | 7 500 ₽ |
| Psychotherapy session | 5 000 ₽ |
| Family psychotherapy | 6 000 ₽ |
| Outpatient rehabilitation in Moscow | 33 000 ₽ |
Expand
We will select an individual treatment plan
Free consultation 8-800-200-27-23
Drug therapy
As already mentioned, the use of special drugs is the main method of treating schizophrenia. They are prescribed by a doctor and they are usually from the line of antipsychotics (neuroleptics). Usually this is one or, very rarely, two drugs, but three - under no circumstances.
The advent of antipsychotics in the mid-twentieth century literally revolutionized the treatment of schizophrenia. Before this, weaker and less effective bromides, plant extracts, opiates, antihistamines, and also a very radical lobotomy were used.
Antipsychotics block dopamine receptors, which cause the main symptoms of schizophrenia – hallucinations and delusions. In addition, they also have the following effects:
- hypnotic;
- sedative;
- antiemetic;
- anti-anxiety;
- relieve cognitive impairment and negative disorders.
Treatment with antipsychotics is a long process, since they have an effect in no less than a month, or even six. And such a long period is not reduced, even if the elimination of the attack was successful.
Taking such medications does not stop during the period of stabilization and prevention.
If a patient has 1 attack, supportive pharmacological treatment continues for two years, 2 attacks - five years, and 3 or more - throughout life.
The dosage can be reduced by a specialist at the preventive stage, but you cannot stop taking the medication without his recommendation - this can cause a relapse.
List of tablets and other forms of medication:
- Chlorpromazine (Aminazine) is the “elder” among antipsychotics. Relieves manic and psychomotor agitation, paranoid state, hallucinations. Has a strong sedative effect. Available in the form of 0.25 and 0.5 g tablets, injection solution. Contraindicated for elderly people.
- Haloperidol is an equally well-known drug, a selective blocker of dopamine receptors. The maximum permissible dose per day is 100 mg, the dosage is determined by the doctor. Available in 1.5 mg tablets, solution, drops.
- Risperidone is a benzisoxazole derivative, the optimal dose is 0.5–6 mg. Affects serotonin and dopamine receptors. Suitable for relief of attacks and prevention.
- Clozapine is a very powerful drug that also has sedative, antidepressant and anxiolytic effects. It is used only if the patient is immune to other antipsychotics, but not to relieve attacks, as it can lead to a decrease in the body's resistance to infections.
- Quetiapine or Seroquel. Its effects are similar to Haloperidol, but it has fewer side effects. Daily dose 150–170 mg.
- Amilsupride (Solian) – acts selectively on dopamine receptors, bypassing alpha-adrenaline, histamine and serotonin receptors. It also has a calming effect. Relieves symptoms of schizophrenia.
- Thioridazine (Sonapax) is a classic antipsychotic, very mild compared to others, has few side effects, calms, relieves depression, suicidal thoughts, etc. Suitable for children from two years old.
This is not the entire list of pharmacological agents for the treatment of schizophrenia.
The doctor selects the drug based on the patient’s health status, age, symptoms, and drug compatibility. Thus, for a certain category of patients, he considers the traditional strong haloperidol more suitable, and for others, the gentle risperidone.
If antipsychotics do not have the necessary effect (and this happens), then other drugs are prescribed, which, unfortunately, are more toxic. If this does not have any effect, then insulin coma, cytokines, and electroconvulsive therapy are used.
Side effects of antipsychotics
Drugs of this group, for all their excellent therapeutic qualities, unfortunately, have many negative side effects. That is, they are unsafe, and such manifestations depend on:
- type of antipsychotic (typical, atypical);
- doses;
- patient's age;
- the patient's condition;
- duration of therapy;
- compatibility with other drugs.
The biggest possibility is parkinsonism, that is, trembling and muscle spasms. Especially often, such a reaction can be caused by first-generation antipsychotics; this is less common for the second.
Other side effects include:
- drowsiness;
- disorders of the gastrointestinal tract;
- anxiety;
- depression;
- increased muscle tone;
- weight gain, change in appetite;
- fear.
Also possible:
- allergy;
- cholestatic jaundice;
- pneumonia;
- epileptic seizures;
- enlargement of the mammary glands;
- decrease in hemoglobin level.
Long-term treatment with antipsychotics risks menstrual irregularities for women, sexual dysfunction for men, and both:
- infertility;
- development of diabetes;
- stroke, ischemia, heart attack;
- osteoporosis;
- constipation;
- dizziness;
- blurred vision, etc.
Taking such drugs for more than 5 years reduces brain weight.
Too high doses of neuroleptics lead to a very dangerous neuroleptic syndrome, manifested by fever, muscle rigidity, and leukocytosis. The result can be terrible - death.
There are no antipsychotics that do not have side effects, even if they are the latest generation. But more effective medications have not yet been invented. Therefore, it is very important that the treatment is carried out by experienced psychiatrists who are able to select the correct medications and their correct dosage. And the patient should strictly follow the specialist’s instructions.
Ancillary drugs
Levodopa will help reduce the parkinsonian effect produced by antipsychotics.
To reduce anxiety and eliminate depression that accompany schizophrenia, tranquilizers - antidepressants are used:
- Phenazepam;
- Diazepam;
- Chlordiazepoxide;
- Sertraline;
- Fluoxetine.
To improve cerebral circulation, nootropics are prescribed: Pantogam and Piracetam.
Lithium salts and carbamazepine help stabilize the emotional state.
No folk remedies can help in the treatment of schizophrenia, but in some cases the doctor may allow tincture of lemon balm, motherwort, and valerian as a sedative.
Signs of antipsychotic drug use
To reduce the side effects of antipsychotic drugs, antidepressants and other stimulants are used in psychiatric practice. The selection of relevant pharmaceuticals requires a long time and careful monitoring by medical personnel.
Recreational use of tranquilizers leads to dramatic changes in a person's appearance and behavior. If the behavior and appearance of a loved one has changed, you should pay attention to the following symptoms of drug addiction:
- Reduced reaction speed, general inhibition;
- Slow speech;
- drooping eyelids;
- Drowsiness, hypersomnia;
- Sudden weight loss or gain;
- Pallor of the skin and mucous membranes;
- Decreased intellectual abilities;
- General negligence of appearance. Due to weakness, the addict neglects personal hygiene, cleaning the apartment, and so on.
Some drug addicts combine taking tranquilizers with alcohol. As a result of this combination, the liver is destroyed, which leads to serious illness and changes in appearance: brittle hair, nail plates, yellowing of the skin, and so on.
MOTIVATION OF A DEPENDENT FOR TREATMENT
Effect on the body
The list of atypical antipsychotics is quite large. Their choice in a particular case is determined by many factors, including the characteristics of the course of the disease. This group of drugs is characterized by an antipsychotic sedative effect. The effect of the drug is manifested in the restoration of a normal emotional state, a decrease in motor excitability, mental and physical relaxation. The patient gets rid of hallucinations, delusions, and automatisms.
Although antipsychotics are not used as sleeping pills, they put a person into a drowsy state, which makes it easier to fall asleep after serious overstimulation. In addition, atypical antipsychotics help increase the effect of various sedatives. They are also used to increase the effectiveness of analgesics and drugs for local anesthesia. They are also prescribed in cases where it is necessary to reduce the strength of the action of mental stimulants.
Who is prescribed antipsychotics?
Drugs in this group are intended for patients with neuropsychiatric disorders, most often accompanied by behavioral and thinking disorders, increased excitability, hallucinations, mania and aggressiveness. In some cases, antipsychotics are used in the treatment of depression, apathy, autism and other diseases with deficiency symptoms. The list of pathologies for which antipsychotic drugs are prescribed begins with the following diseases:
- manic-depressive disorder;
- dementia accompanied by behavioral disorders;
- overexcitation of hysterical type;
- schizophrenia;
- alcoholic, stimulant psychosis.
In small doses, psychotropic drugs are used to treat neurosis-like disorders.
Kinds
Antipsychotics are classified according to various criteria. But in clinical practice, it is customary to subdivide such drugs according to their leading action. Modern antipsychotics include three groups of psychotropic drugs:
- Sedatives . These are mainly sedative medications that eliminate anxiety, promote muscle relaxation, normalize sleep processes, and inhibit mental activity. They are not used if the patient has delusions and hallucinations. One example of such drugs is Aminazine.
- Antipsychotic . The action of these chemicals is aimed at eliminating delirium, mental overexcitation, increased motor activity, and hallucinations. Some medications in this group are prescribed as a sedative. But there are also those that increase disinhibition, activate thinking and motor functions. Representative of antipsychotic drugs Sulpiride.
- Proofreaders . Their purpose is to restore behavioral factors, relieve emotional arousal, eliminate hot temper and aggressiveness. Area of application: severe psychopathic disorders and psychoneuroses. Periciazine is an effective behavior corrector.
Important! Using the above medications without a doctor’s prescription can lead to serious health problems!
Side effects from antipsychotics
The doctor prescribes antipsychotics based on the patient's medical history and current condition. Vigilance helps minimize the harm of antipsychotics. Independent, inept use of drugs leads to adverse reactions, the development of addiction and undesirable mental states. Due to recreational use, addicts face the following side effects:
- General excitement;
- Anxiety;
- Uncontrollable desire to move due to discomfort in the limbs;
- Impaired liver and kidney function;
- Hypersomnia;
- Sleep disturbances;
- Endocrine disorders, incl. development of metabolic disorders leading to weight gain;
- Diseases of the cardiovascular system.
Side effects of antipsychotics
When treated with antipsychotics, neuroleptic syndrome may occur. Extrapyramidal disorders of the syndrome are expressed in hypo- or hyperkinetic disorders. The former are characterized by a decrease in motor activity, stiffness of the muscular skeleton, tremors of the limbs, problems with maintaining balance; the second - tremors, involuntary movements, muscle twitching, spasms of the masticatory muscles, stiffness of movements, slow speech, motor activity. Typically, the neuroleptic syndrome includes both hypo- and hyperkinetic disorders.
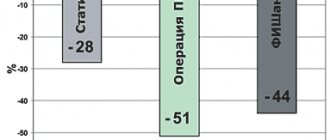
Rice. 3. Side effects of neuroleptics.
In neuroleptic syndrome, muscle spasms are paroxysmal in nature. They usually affect the facial and neck muscles - the muscles of the lips, tongue, jaws, eyes, pharynx, and throat contract. In some cases, autonomic disorders appear, even to the point of fainting.
Restlessness, physical activity
In addition to extrapyramidal disorders, akathisia may occur while taking antipsychotics:
- anxiety, restlessness;
- excited state;
- emotional indifference;
- sleep disorders, insomnia;
- feeling of restlessness;
- "restlessness in the legs";
- need to move.
Tardive dyskinesia
If treatment with antipsychotics is carried out long enough (from 2 years), there is a risk of developing tardive dyskinesia. It is expressed in involuntary movements of the lips, tongue, facial expressions, and limbs that are beyond control.
Autonomic nervous system disorders
Disorders of the autonomic nervous system can manifest themselves in postural hypotension (a drop in blood pressure when taking an upright position), dysuric disorders (painful, difficult urination), gastrointestinal disorders (diarrhea, constipation), increased sweating, weight gain, blurred vision, disorders functioning of the cardiovascular system.
Women may develop dysmenorrhea (with an increase in prolactin in the blood), cycle disruption, and manifestations of pseudohermaphroditism; in men - gynecomastia, decreased libido, delayed ejaculation, galactorrhea (secretion of milk from the mammary glands), hirsutism (excessive hair growth). In rare cases, increased sensitivity of the skin to sunlight and ultraviolet rays, dermatitis, pigmentation and allergic reactions occurs.
Severe complications of neuroleptic therapy
In cases where the patient is not observed by the attending physician (does not make follow-up visits, does not notify the doctor about changes in health status that cause anxiety and concern, does not follow recommendations for control and diagnostic measures), there is a risk of developing severe complications of antipsychotic therapy, for example:
- allergic reactions;
- toxic reactions;
- hepatitis;
- pathologies of the organ of vision;
- disorders of blood biochemistry.
In addition, when treated with antipsychotics, there is a risk of developing mental disorders (for example, asthenic type depression), severe sleep disorders, delirium (patients with organic pathology of the central nervous system, the elderly, children fall into the risk category), epileptiform seizures.
Antipsychotics of any generation should be taken in accordance with the recommendations of the attending physician. Refusal to take or increase the dosage unilaterally is unacceptable. Monitoring visits are mandatory, including unplanned ones, if there are signs of deterioration in health. Diagnostic recommendations, including a biochemical blood test, make it possible to assess the effectiveness of therapy and prevent the development of complications.
Contraindications
Antipsychotics should not be taken simultaneously with alcoholic beverages. Some drugs should not be used during pregnancy and lactation, or for people with acute heart, kidney or liver diseases. Each drug has its own list of contraindications. In this regard, the over-the-counter sale of antipsychotics is strictly prohibited.
Ambulatory treatment
Neuroleptics in the treatment of mental disorders in children
The increase in the number of prescriptions of antipsychotics, medications that eliminate delusions, hallucinations, motor and mental agitation, is due to several reasons.
One of the main ones is the emergence of a new generation of antipsychotics on the global pharmaceutical market. We are talking about drugs that provide highly effective therapy and are characterized by relative safety for patient health and a minimum number of side effects. Another reason is the possibility of prescribing antipsychotics not only by psychiatrists, but also by pediatricians and neurologists. However, it is difficult to call the popularization of antipsychotics an unambiguously positive trend. Yes, these drugs can effectively relieve severe symptoms, but the risk of adverse reactions remains, especially since long-term treatment is required, and side effects can develop into persistent diseases.
Types of antipsychotics
There are several types of tranquilizers that are used to treat mental disorders, as well as for premedication before surgery.
Typical antipsychotics
Typical antipsychotics are effective in suppressing severe mental conditions but cause chronic fatigue syndrome. These include Haloperidol, Chlorprothixene, Sulpiride, Chlorpromazine and other medications.
Find out treatment recommendations without leaving home for free
To select a treatment plan, you just need to leave a request, we will contact you to select the time and specialist you need
Submit your application
Atypical antipsychotics
Unlike typical ones, such antipsychotics have a milder effect and are easier to tolerate. Due to the peculiarities of their effect on the dopamine system, atypical drugs do not cause severe inhibition and have a less extensive list of side effects.
New generation neuroleptics
The pharmaceutical market is replenished with new generation drugs that have a gentler effect on the patient. The fact is that in severe mental illnesses, antipsychotics are taken for life. To minimize side effects, newer drugs combine CNS depression and low hepatotoxicity.
The safest antipsychotic
To select the safest group of tranquilizers, the doctor relies on the following factors:
- Preference for new generation drugs;
- Presence of kidney, liver, etc. diseases;
- Tendency to develop certain pathologies;
- Determination of a safe dose of the drug.
The doctor prescribes the safest tranquilizers that do not harm the patient and help normalize well-being. Taking antipsychotics without taking into account the rules for using such drugs only leads to adverse reactions.
Neuroleptics without sedation
Second generation drugs do not cause severe sedation. Taking them promotes healthy sleep and relief from mania: at the same time, a person’s sanity is preserved. Despite this, excessive use leads to the development of pharmaceutical addiction.
Neuroleptics – friends or enemies?
Doctors prescribe antipsychotic drugs and antipsychotics very often for a variety of diseases - schizophrenia, autism, dementia, obsessive-compulsive disorder and others. At the same time, it is known that these drugs are by no means safe and lead to the development of severe side effects - hormonal imbalance, weight gain, heart problems and even encephalopathy. How justified is such a wide prescription of antipsychotics, what can replace them and how to maintain your health?
Differences between neuroleptics and antipsychotics
Let's start with how the different groups of drugs under consideration differ. There are three generations of medications that affect the brain's dopamine system. The first, oldest generation is antipsychotics (it would be more correct today to talk about first-generation antipsychotics). Antipsychotics include Haloperidol, Chlorprothixene, Aminazine, Trifluoperazine (Triftazine), Tioproperazine (Mazeptil), Chlorpromazine, Levomepromazine (Tizercin), Flupenthixol and others. These drugs cause multiple side effects - muscle stiffness, restlessness (it is difficult for the patient to sit in one place), involuntary contractions of the body muscles, jaw spasms, "rolling of the eyes", "turning of the neck", other involuntary movements, increased levels of the hormone prolactin, decreased production of corticotropic hormones. and somatotropic hormone, cardiac dysfunction, decreased cognitive function, weakened motivation (apathy, indifference, weakened will), loss of interest in the world around us. It is about neuroleptics that they usually say that these drugs “turn a person into a vegetable.” To overcome the side effects of neuroleptics, corrector drugs are prescribed, for example, Biperiden (Akineton - safer than Trihexifemidyl (Cyclodol)). The latter drug not only causes addiction, impairs vision, and interferes with urination, but is also capable of causing acute psychosis with visual hallucinations. Today, neuroleptics are used extremely rarely.
Today, the most commonly used antipsychotic is Haloperidol. This drug, along with Olanzapine, is best able to stop acute psychosis. However, its neurological side effects (from stiffness and drooling to convulsions and spasms) make this drug more cautious. I do not recommend combining it with other psychotropic drugs, prescribing too large doses and administering Haloperidol intramuscularly for more than 5 days.
The second generation of drugs - atypical antipsychotics, cause fewer side effects. The predominant symptoms are an increase in the production of prolactin, an increase in body weight, an increase in blood sugar and, much less frequently, disturbances in the functioning of the heart. Second generation drugs include Olanzapine, Risperidone, Quetiapine, Ziprasidone.
The third generation of drugs - Aripiprazole, Brexpiprazole and Cariprazine - have minimal side effects, but also weaker activity, most often insufficient to relieve psychosis, but are suitable for maintenance therapy. One of the typical mistakes of patients is the race for new antipsychotics (Lurasidone, Cariprazine, Serdolect, etc.). By and large, these drugs are intended for maintenance therapy, not for the relief of acute psychosis, and also have their own nuances of action and their side effects, which, by the way, psychiatrists still know little about.
Clozapine (Azaleptin) stands apart. This drug is quite strong, has a rare but potentially dangerous side effect - agranulocytosis, but is used in cases where other drugs have not worked for the patient.
When are antipsychotics prescribed?
Antipsychotic drugs are prescribed for a wide range of conditions in adults, children and the elderly. For children with mental retardation, antipsychotics are prescribed to reduce motor agitation, irritability, aggression or self-aggression. Children with autism, severe ADHD, and Tourette's syndrome are also prescribed antipsychotics. Often, prescriptions are made without attempts to solve the problem using other, safer methods: work by a clinical psychologist with triggers of anxiety or aggression in children with developmental delays and autism, biophysical methods of therapy (tDCS, tACS), taking mood stabilizers in cases where they are indicated. The prescription of antipsychotics in many cases occurs without a preliminary examination, even an EEG and MRI. This approach is wrong. It is worth prescribing antipsychotics only in extreme cases after a thorough diagnosis, when other treatment options have been ineffective or there is a need for emergency care, there is no cooperation with the patient (prolongations) and we see a clear benefit from maintenance therapy, despite the side effects of the antipsychotic. Sometimes children come to our clinic who have tested positive for hydrocephalus or epi-activity. The children took antipsychotics for a long time, although, obviously, in such cases completely different drugs are needed.
For adults, antipsychotics are prescribed for schizophrenia, schizoaffective, bipolar disorders, various types of psychoses, and less often for psychotic or resistant depression, OCD and PTSD. Just as in the case of children, antipsychotics are often prescribed without prior diagnosis. Unfortunately, many psychiatrists focus only on symptoms (hallucinations, delusions, etc.), ignoring the actual results of research and not understanding that these symptoms may themselves be a consequence of neurological diseases or damage to internal organs. As a result, many patients spend years taking medications they don't need. Read more about the treatment of schizophrenia here >>
Finally, antipsychotics are often prescribed to older people for various types of dementia, delirium, hallucinations, and delirium. This category of patients is the most vulnerable to side effects. Antipsychotics (1st generation antipsychotics) should not be prescribed to elderly patients, as this increases the risk of neurological disorders, such as stroke and heart damage (heart failure), not to mention deterioration of vision and liver damage. In cases where the prescription of an antipsychotic cannot be avoided, you need to carefully select the drug and start with the minimum dosage. It is extremely important to control the concentration of the drug in the blood (treatment in the “therapeutic window”, below a certain limit the drug does not work, above a certain limit side effects dominate), and ideally also the products of its metabolism, especially in patients with impaired liver function and encephalopathy, in order to avoid dangerous accumulation of the drug in the body.
Neuroleptics are easier to prescribe than to stop
If you came to a psychiatrist and he immediately prescribed you antipsychotics, then do not rush to take them right away, try to find a psychiatrist who will give you an accurate diagnosis, not based on “conversations” and observation of your “wrong behavior”, but as a result of research brain Unfortunately, antipsychotics are easier to prescribe than to stop. If the first takes a few minutes, then the second takes more than one month.
Truly, the skill of a psychiatrist is noticeable in the way he cancels neuroleptics (usually in a tapered manner over 1-3 months). Discontinuation of antipsychotics is associated with a risk of withdrawal effects and exacerbation of the disease. To understand what this is, imagine that your neurons (brain cells) are springs of water (“keys”). During psychosis, they are active and throw out too many impulses (by analogy - “water”). Antipsychotics act like a dam, blocking the flow of water and stopping the exacerbation. If you suddenly remove the dam (antipsychotics), you will get a large “wave” or exacerbation of psychosis.
Antipsychotics for the treatment of acute psychosis
Most psychiatrists believe that the benefits of antipsychotics are greater than the harm, but in fact, there is still no answer to this question. Unless, of course, the patient has acute psychosis, psychomotor agitation, acute delirium or imperative hallucinations (a danger to himself and others) and there is no time to make a diagnosis, in other words, there is no choice, and one must act quickly. In such cases, the prescription of antipsychotics is justified. However, if a mental disorder lasts for several months or even years, it is worth spending a few days to clarify the diagnosis and find the cause of the mental disorder.
It is better to relieve an acute condition with one antipsychotic than several. With this treatment (monotherapy), fewer side effects are achieved, which will then need to be eliminated over a long period of time.
Treatment without antipsychotics
Today it is known that there is no better antipsychotic and no worse one. A qualified psychiatrist knows that each patient has its own diagnosis, each diagnosis has its own drug, and each drug has its own dose. However, let’s ask one more question: can we do without antipsychotics today? Apparently yes, at least that's what I'm striving for. There are biophysical treatments such as transcranial magnetic stimulation (TMS) that are effective for auditory hallucinations. For autoimmune neuropsychiatric disorders, plasmapheresis has proven itself well (it is important that it is carried out on high-quality modern equipment that allows the isolation of certain blood cells or substances that cause inflammation of the brain). Another option for pathogenetic treatment aimed at the mechanisms of occurrence of mental disorders is biotherapeutic drugs, including cytokine therapy, interferons and natalizumab. Neuroviruses, which often cause mental disorders, are also successfully treated with antiviral drugs, usually in combination with drugs that strengthen the immune system (Acyclovir, Genciclovir and other representatives of this class of drugs + Immunofan, Lykopid, etc.).
How long to take antipsychotics?
In classical psychiatry, it is generally accepted that after an exacerbation, antipsychotics are prescribed for a certain long period of time or even for life. I am against this opinion. Where does the figure in years come from for how long a person should take an antipsychotic? This is similar to the average temperature in the hospital. To make a decision about stopping a drug, you need actual research data that makes it clear what is happening to the brain. If everything is fine, you should try to stop the drug or switch to maintenance courses.
In general, I would like neuroleptics to be taken less frequently and prescribed for a short period of time, and if they were prescribed, then the concentration of the drug in the blood, side effects and complications would be monitored, and the antipsychotic would be selected using a pharmacogenetic study, and not by the “trial and test” method. mistakes."
Intramuscular and long-term
Is it worth using prolonged forms (prolongs) - those antipsychotics that are administered intramuscularly for a long time? From my point of view, it is better not to use Haloperidol-decanoate, Fluanxol-depot, and especially Moditen-depot. Risperidone, Paliperidone or Aripiprazole prolongs are more suitable for maintenance therapy.
In all cases, before introducing prolong, a thorough examination and gradual preparation of the patient for the introduction of long-acting antipsychotics is necessary (in my experience - at least a month). However, I emphasize once again that I am not a supporter of treatment with antipsychotics for years, especially without monitoring the effectiveness and safety, determining the concentration of the drug in the blood, collaborating with the patient and working together with clinical and social psychologists, and ideally, social and labor rehabilitation. And yet, prolongations are necessary when there is no cooperation with the patient, when it is important to maintain an even concentration of the drug in the blood, and when it is clear that the treatment will last long enough.
Drug combinations
Often, psychiatrists prescribe several antipsychotics at once. Very rarely such appointments are justified. It is optimal to select one drug that is suitable for a particular patient with his individual characteristics of response to the drug and the rate of drug elimination by the liver. For selection, it is worth using a pharmacogenetic study.
Is it possible to combine an antipsychotic with an antidepressant or mood stabilizer? In most cases, yes, but not always, and with a very good understanding of pharmacological genetics and drug metabolism. For example, Carbamazepine sharply reduces the effectiveness (concentration level) in the blood of many antipsychotics. In general, it is better to protect the patient from a large number of drugs.
To summarize, it is worth saying that any drug in the hands of a competent doctor, with the correct diagnosis and correctly prescribed treatment, can be useful.
Also, you may be interested in the following materials on our website:
1.
2.
3.
4.
List of antipsychotics
Neuroleptics are classified not only by the characteristics of their effect on dopamine receptors, but also by the generation of the drug.
First generation neuroleptics
First generation drugs include derivatives of thioxanthene, phenothiazine, and butyrophenone. They quickly relieve unwanted mental states and are often used to treat psychosis. Such drugs include Fluphenazine, Haloperidol, Chlopromazine, etc.
Second generation neuroleptics
Second generation drugs have a milder effect on dopamine receptors and low hepatotoxicity. According to research, taking such drugs (especially Quetiapine) has a lesser effect on metabolic processes. Second generation drugs include:
- Risperidone;
- Quetiapine;
- Clozapine;
- Sertindole;
- Ziprasidone.
Neuroleptics of the latest generation
The latest generation of drugs have less impact on the endocrine, cardiovascular systems, and liver. The most popular new antipsychotics include Clopixol-acufase and Clopixol-depot.
Mechanism of action of antipsychotics
The therapeutic mechanism of action of antipsychotics is associated with the relief of increased dopamine activity in the mesolimbic pathway, one of the dopaminergic nerve pathways. The mesolimbic pathway connects the substantia nigra and the ventral tegmental area of the brain with the structures of the limbic system. This pathway is responsible for processes in the body associated with neuroendocrine regulation, emotions, memory, the ability to learn and experience pleasure. In addition, this system is partially responsible for controlling the onset of motor responses and their affective variations.
Rice. 2. The mechanism of action of neuroleptics.
Blockade of dopamine receptors
Elevated levels of dopamine in the mesolimbic pathway cause psychotic states and productive symptoms (for example, hallucinations, delusions, active manifestations of anxiety states). Typical antipsychotics, by reducing dopamine activity by blocking more than 65% of D2 receptors, reduce positive psychotic symptoms.
The mechanism of action of first-generation antipsychotics can cause non-core effects - motor restlessness, involuntary muscle contractions, contributes to the development of a depressive or anxious state, emotional depression, and anhedonia. Such effects, as they appear, can be stopped by adjusting the dosage or introducing symptomatic therapy.
Long-term blockade of D2 receptors in the mesolimbic structures leads to an increase in the sensitivity of the receptors or an increase in their number, and attempts by neurons to restore intersynaptic connections. This results in hypersensitivity to dopamine and the potential danger of developing psychosis even with a slight increase in the level of the neurotransmitter. “Hypersensitivity” psychosis (positive symptoms) can be triggered by alcohol consumption, smoking and other dopamine-increasing substances, including medications.
Partial blockade of dopamine receptors
Some atypical antipsychotics, which block 2D dopamine receptors partially, mimic the neurotransmitter in its “attenuated form.” Thus, the mechanism of action of second-generation antipsychotics is associated with a “mild” correction of dopamine levels, which contributes to a moderate reduction of positive symptoms and reduces the risks of non-core effects.
Treatment with second-generation antipsychotics reduces the risk of anhedonia, hyperprolactinemia, hypersensitivity psychosis, tardive dyskinesia and extrapyramidal disorders. However, the drugs are still not without side effects, in particular, when they are taken, norepinephrine activity in the substantia nigra remains, which can cause the development of akathisia (internal restlessness, desire for physical activity) with long-term use.
Blockade of serotonin 5-HT2A-, 5-HT1A-, 5-HT2C receptors
The mechanism of action of another group of atypical antipsychotics is associated with the ability to bind to serotonin 5-HT2A receptors, indirectly affecting dopamine levels. 5-HT2A receptors connect the serotonin and dopamine systems, and their blocking leads to a decrease in the activity of the dopamine neuron directly and indirectly by reducing the release of GABA.
When serotonin levels increase, 5-HT1A receptors, which are responsible for the self-regulation of the serotonin neuron, inhibit their activity. This stops the effect of serotonin on 5-HT2A receptors and reduces the activity of the dopamine neuron. A similar, but “mild” effect can be achieved using an agonist that imitates the effect of serotonin on 5-HT1A receptors.
Some second-generation antipsychotics block serotonin 5-HT2C receptors, increasing dopamine levels and decreasing serotonin. The resulting processes in intermediate GABA neurons reduce the production of dopamine. Drugs that act on α2-adrenergic receptors (analogs of 5-HT1A receptors) work on the same principle. Their blockade with an antipsychotic leads to the release of norepinephrine, inhibiting its reuptake and, accordingly, increasing its activity.
These processes explain the therapeutic effect of second-generation antipsychotics, aimed not only at relieving psychotic symptoms, but also at improving cognitive functions, reducing negative symptoms and depressive states. In other words, second-generation drugs are able to correct the levels of dopamine, norepinephrine and serotonin in the brain (mainly in the prefrontal cortex).
Multireceptor blockade
Third-generation neuroleptics have the property of multireceptor blockade, affecting dopamine, serotonin, cholinergic, adrenergic and other systems associated with the occurrence of psychotic states. They have an expanded profile of therapeutic effect, stopping positive symptoms and reducing negative ones; non-core effects occur extremely rarely in clinical practice.
Consequences of neuroleptics
Self-administration of tranquilizers leads to the development of severe mental syndromes. As a result of prolonged, uncontrolled and excessive use of antipsychotics, mental retardation, loss of memory, and intellectual functions develop; Severe pathologies of the liver, brain, and central nervous system develop.
Group classes in
Neuroleptics and alcohol
Taking alcohol together with tranquilizers leads to complications such as poisoning leading to coma, toxic liver damage, psychosis, and even sudden cardiac arrest.
Antipsychotic drug poisoning
There are several symptoms of antipsychotic poisoning:
- Nausea, vomiting;
- Severe weakness and dizziness;
- Dry mouth;
- Ataxia;
- Impaired reflexes and reactions;
- Decreased or absent reaction to light;
- Loss of consciousness;
- Pulse depression;
- Reduced blood pressure;
- Convulsive attacks, foaming at the mouth.
If symptoms of poisoning appear, seek immediate medical attention.
Dyskinesia from neuroleptics
Uncontrolled use of antipsychotics (especially the first generation) leads to the development of dyskinesia, non-infectious hepatitis, cirrhosis and other damage to the liver and gallbladder.
Insomnia
Akathisia, a common side effect due to the use of antipsychotics, can include anxiety, panic, and insomnia. As a result of disturbances in the biochemical processes of the brain, disturbances in sleep and alertness occur.
Workbooks
Disorders of the nervous system
Other consequences of recreational use of tranquilizers include disorders of nervous activity. Lethargy, memory deterioration, and suppression of natural reflexes occur. Due to the lack of regular use of an antidepressant, psycho-emotional disorders occur, including depression.
Rehabilitation specialists
Overdose of antipsychotics
Symptoms of an overdose of antipsychotics include:
- Deterioration in coordination of movements;
- Decreased blood pressure and pulse;
- Dizziness;
- Nausea, vomiting;
- Loss of consciousness;
- Coma;
- Heart failure.
In case of an overdose, it is necessary to urgently rinse the stomach using the “restaurant” method, but only if the person is conscious. You should call an ambulance doctor to your home.
List of drugs without prescriptions
Some ataractic medications are sold without a prescription, these include:
- Glycine, Afobazole;
- Novo-passit;
- Stressovit, Persen;
- Magnesium B6, Tenoten.
Sedatives, which are dispensed without a doctor's opinion, are not complete medications for people with clinical depression. But they will help improve your psycho-emotional well-being. However, it is not recommended to prescribe any treatment on your own. Therefore, it is worth contacting a specialist to select a therapeutic agent that is suitable for its effectiveness, taking into account individual characteristics, assessing the consequences and setting the dose.
Literature
- “SIDE EFFECTS OF NEUROLEPTICS. MALIGNANT NEUROLEPTIC SYNDROME.” Esina A.I., Purveev S.S., Nekrasov M.S. (2019);
- “The use of neuroleptics and poisoning with them in medical practice.” Arustamyan O.M., Tkachishin V.S., Kondratyuk V.E., Alekseychuk A.Yu. (2019);
- “Pharmacoepidemiological analysis of the effectiveness and safety of classical and atypical antipsychotics.” Andreev Boris Vladimirovich, Vilyum Irina Alexandrovna, Kurylev Alexey Alexandrovich (2010);
- “Atypical neuroleptics risperidone and paliperidone in pharmacological and chemical-toxicological terms.” Bulatov Ruslan Maratovich (2011);
- “Current trends in drug addiction in Russia and Western countries.” Shulgina Elena Viktorovna (2019);
- “The drug situation in Russia and new patterns of drug use.” Pozdnyakova Margarita Efimovna (2016).
Article verified by an expert
Terekhova Anna Vladimirovna
psychologist-consultant on socio-psychological work with addicted clients and their families. More than 10 years of experience.
Similar articles:
How long does heroin stay in the body?
Addiction to nasvay
Can an addict stop using drugs forever?
Signs and consequences of using spice
Treatment methods for alcoholism: comparison of effectiveness
List of used literature
1. Jones P.B., Buckley P.F. "Schizophrenia. Clinical guidelines".
2. Smulevich A.B. "Treatment of low-grade schizophrenia."
3. Snedkov E.V. "Atypical antipsychotics: searching for solutions to old and new problems."
4. Krasnov V.N., Gurovich I.Ya., Mosolov S.N., Shmukler A.B. "Standards of care for patients with schizophrenia."
5. Ivanov S.V., Smulevich A.B., Voronova E.I. “New generation antipsychotic cariprazine in the treatment of schizophrenia: spectrum of clinical efficacy and safety.”
6. Geddes J., Freemantle N., Harrison P., Bebbington P. “Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis.”
7. Jindal RD, Keshavan MS “Classifying antipsychotic agents. Need for new terminology."
8. Correll CU, Rubio JM, Inczedy-Farkas G. “Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia.”
9. Wang S.M., Han C., Lee S.J. “Investigational dopamine antagonists for the treatment of schizophrenia.”
10. K.S. Raevsky. "Modern neuroleptics: interaction with brain neurotransmitter systems."
Share
Share
Good news
A new antipsychotic for the maintenance treatment of schizophrenia from the Janssen company, part of the Johnson & Johnson pharmaceutical division, Trevicta, has been registered in Russia. It has a long-lasting effect and can be used only 4 times a year, that is, every three months, which is much better than monthly injections of long-standing antipsychotics.
Trevicta is now an antipsychotic with the longest dosing interval registered in our country. It maintains its optimal concentration of paliperidone in the patient’s blood for a long time, which is why it requires such rare use.
Prescribe three months of Trevicta to patients with a stable condition after treatment with other drugs. It helps reduce the risk of relapse due to its prolonged action, has a low risk of side effects, and does not create withdrawal syndrome if treatment is abruptly stopped. This makes it possible for a patient with schizophrenia to socialize and maintain his constant normal state.
Clopixol tablets (zuclopenthixol hydrochloride) - oral form
This form of the drug has a much longer history of use than Clopixol Akufaz and is widely used throughout the world for the treatment of schizophrenia and other mental illnesses.
To date, a large amount of information has been accumulated on the experience of using zuclopenthixol tablets in the treatment of acute psychoses, exacerbations of chronic psychoses and acute manic states. Many direct and comparative, including double-blind, tests of this drug have been carried out, confirming its high therapeutic effectiveness, comparable to the effectiveness of haloperidol and chlorpromazine.
In the UK, a multicentre study compared, using a double-blind method, the effect of tablet forms of Clopixol and chlorpromazine in acute psychoses (schizophrenia and schizoaffective psychoses). The study included patients aged 18 to 65 years who began receiving Clopixol 25–150 mg/day (average 75 mg/day) or chlorpromazine 100–600 mg/day. Starting from the second week of treatment in most patients, without compromising the therapeutic effect, the daily dose of Clopixol was reduced to 50 mg. Chlorpromazine was used mainly at a dose of 600 mg/day throughout the study (10 weeks). Both drugs showed high antipsychotic activity. According to this indicator, there was a tendency towards an advantage of Clopixol, but it did not reach the level of statistical significance.
Another multicenter study compared the effects of tablet forms of Clopixol and haloperidol on acute psychosis using a double-blind method. The average daily dose of clopixol was 33.5 mg, haloperidol - 10.3 mg. Both drugs showed equally high therapeutic activity, however, patients taking Clopixol were discharged from the psychiatric hospital earlier, which reflected the more rapid development of the antipsychotic effect of Clopixol compared to haloperidol. Clopixol caused a significantly more pronounced reduction in the anxiety-depressive component of psychosis than haloperidol. In addition, extrapyramidal symptoms in those taking Clopixol were, as a rule, transient, while in patients receiving haloperidol they were almost permanent.
Significant improvement while taking Clopixol tablets was observed in 69 - 87% of patients with acute and subacute manic conditions. A significant reduction in the acute manifestations of manic disorder was observed according to various data during the first 1 to 4 weeks of therapy. In some studies, in some of the most severe cases, treatment of the acute condition began with the use of Clopixol Acufase for the first 3 to 6 days of treatment, and then continued with Clopixol tablets. It is important to note that the use of high doses (up to 130 - 150 mg/day) was not more effective than the use of medium therapeutic doses for mania (20 - 50 mg/day). About 80% of patients received the drug at a dose of 20 - 30 mg/day, and increasing the dosage above 50 mg/day did not increase the effectiveness of therapy, but only led to an increase in the severity of side effects. Most researchers have concluded that, with a good therapeutic effect, dose reduction can begin on average 2 weeks after the start of treatment without the risk of exacerbation. It has been suggested that the treatment of mania requires slightly lower doses than for the treatment of schizophrenia.
The use of Clopixol for agitation and aggressiveness in the elderly is of particular interest. Clopixol was compared in a double-blind manner with thioridazine and the combination of haloperidol and levomepromazine. Both studies were conducted in Scandinavia and were multicenter. The first of them included inpatient dementia patients (mainly with Alzheimer's disease) aged 64 to 97 years. Their mental state was characterized by “the presence of restlessness, hostility, as well as accompanying anxiety, confusion, irritability, insomnia, delusions, hallucinations, hypochondria, and screams.” A higher effectiveness of Clopixol on insomnia was found (the difference between the drugs is statistically significant). Side effects of Clopixol occurred rarely, their severity was insignificant, and no serious adverse effects on the cardiovascular system associated with the drug were observed.
A patient population similar in demographic and clinical characteristics was used to compare Clopixol tablets with a combination of haloperidol and levomepromazine (tizercin, nozinan). The study lasted 4 weeks. The starting dose for Clopixol was 4 mg (one 2 mg tablet twice a day). In another group of patients, 1 mg of haloperidol was prescribed in the morning and 5 mg of levomepromazine in the evening. The average daily drug doses at the end of the study were slightly higher: 4.8 mg clopixol; 1.6 mg haloperidol + 7.6 mg levomepromazine. The authors concluded that for the treatment of aggression and agitation in the elderly, it is preferable to use Clopixol tablets because it acts faster and allows monotherapy.
It should be noted that, in accordance with the average dosages used for a particular mental pathology, tablets of different dosages are produced: 2, 10 and 25 mg, which makes the use of the drug more convenient.
Thus, literature data indicate that Clopixol tablets can be successfully used both in the treatment of acute and subacute psychoses, including acute manic states, and in the treatment of agitation and aggressiveness in the elderly, as well as for the correction of behavioral disorders in persons with intellectual disabilities .
Classification of antipsychotics
There are several classifications of antipsychotics - according to their chemical structure, as well as according to the characteristics of their action.
Based on their ability to cause drug-induced parkinsonism (a syndrome associated with a lack of dopamine, which is manifested by stiffness of movements, increased muscle tone, trembling of the hands and head, and postural disturbances), antipsychotic drugs are divided into “typical” (which cause it) and “atypical” (which do not cause drug-induced parkinsonism). parkinsonism):
Typical antipsychotics:
- phenothiazine derivatives: aliphatic derivatives (chlorpromazine, levomepromazine);
- piperazine derivatives (perphenazine, trifluoperazine, fluphenazine);
- piperidine derivatives (thioridazine, pipothiazine);
Atypical antipsychotics:
- derivatives of dibenzodiazepine, oxazepine, thiazepine and oxepine: clozapine, olanzapine, loxapine, quetiapine;
- benzisoxazole derivatives: risperidone;
- benzamide derivatives: amisulpride, sulpiride, tiapride;
- indole derivatives: sertindole, ziprasidone;
- others: risperidone, aripiprazole, paliperidone, cariprazine.
In addition, the antihypertensive drug raunatin, which contains reserpine, has an antipsychotic effect.