Pharmaceutical action
pharmacodynamics. The active substance, pregabalin, is an analogue of GABA ((S)-3-(aminomethyl)-5-methylhexanoic acid).
Mechanism of action. Pregabalin binds to the auxiliary subunit (α2-δ protein) of voltage-gated calcium channels in the central nervous system, actively replacing [3H]-gabapentin.
Clinical experience
Neuropathic pain. The effectiveness of the drug has been demonstrated in studies for diabetic neuropathy and postherpetic neuralgia. The effect on other types of neuropathic pain has not been studied.
Pregabalin was studied in 9 controlled clinical studies of up to 13 weeks with twice daily dosing and in studies of up to 8 weeks with twice daily dosing. Overall, the safety and efficacy profiles were similar for the 2- and 3-times-daily dosing regimens.
In clinical studies lasting up to 13 weeks, pain reduction was observed in week 1 and was maintained throughout the treatment period.
In controlled clinical trials, 35% of patients in the pregabalin group and 18% in the placebo group experienced a 50% improvement in pain scores. Among patients who did not experience drowsiness, this improvement was observed in 33% of patients in the pregabalin group and 18% in the placebo group. Among patients who experienced drowsiness, efficacy rates were 48% in the pregabalin group and 16% in the placebo group.
Fibromyalgia. Pregabalin monotherapy was studied in 5 placebo-controlled studies: 3 fixed-dose studies lasting 12 weeks, 1 fixed-dose study lasting 7 weeks, and a 6-month long-term efficacy study. In all fixed-dose studies, pregabalin (300–600 mg twice daily) provided a significant reduction in pain associated with fibromyalgia.
In 3 12-week fixed-dose studies, 40% of patients in the pregabalin group experienced a 30% improvement in pain scores compared with 28% in the placebo group; 23% of patients in the pregabalin group had a 50% improvement in their score compared with 15% in the placebo group.
Pregabalin provided significantly better patient global impression of change (PGIC) scores in 3 12-week fixed-dose studies compared with placebo (41% of patients in the pregabalin group felt much better or reported significant improvement compared with 29 % in the placebo group). According to the Fibromyalgia Impact Questionnaire (FIQ), pregabalin provided statistically significant improvements in function compared with placebo in 2 of 3 fixed-dose studies that assessed this measure.
Pregabalin provided significant improvements in sleep in 4 fixed-dose studies, as measured by patient-reported sleep disturbance subscale scores on the MOS-SS (Medical Sleep Study Scale), MOS-SS Total Sleep Problems Index, and sleep quality diaries.
In the 6-month pain reduction study, improvements in global score (PGIC), functioning (FIQ total score), and sleep (MOS-SS sleep disturbance subscale) were maintained significantly longer in patients in the pregabalin group than in patients in the placebo group.
When using pregabalin 600 mg/day, patients reported additional improvement in sleep compared to those taking 300 and 450 mg/day; the mean effects on pain, global score, and FIQ were similar to those of 450 and 600 mg/day, although the 600 mg/day dose was slightly less well tolerated.
Epilepsy. Pregabalin was studied in 3 controlled clinical studies lasting 12 weeks at dosing 2 or 3 times daily. The safety and efficacy profiles for the 2 or 3 times daily dosing regimens were similar.
A decrease in the frequency of attacks was noted in the 1st week of treatment.
Generalized anxiety disorder (GAD). Pregabalin was studied in 6 controlled studies of 4–6 weeks duration, in elderly patients for 8 weeks, and in a long-term relapse prevention study with a 6-month double-blind relapse prevention phase.
A decrease in the severity of GAD symptoms according to the Hamilton Anxiety Scale (HAM-A) was noted at week 1. In controlled clinical trials of 4 to 8 weeks, 52% of patients in the pregabalin group and 38% in the placebo group had at least a 50% improvement in HAM-A total score from baseline to endpoint.
Pharmacokinetics. The pharmacokinetics of pregabalin were similar in healthy volunteers, patients with epilepsy using antiepileptic drugs, and individuals with chronic pain.
Absorption. Pregabalin is rapidly absorbed when administered orally on an empty stomach and reaches Cmax in blood plasma within 1 hour after single or multiple doses. The estimated oral bioavailability of pregabalin is ≥90% and is independent of dose. After repeated administration, steady state is achieved within 24–48 hours. The extent of absorption of pregabalin is reduced when administered concomitantly with food, resulting in a decrease in Cmax by approximately 25–30% and Tmax by approximately 2.5 hours. However, administration of pregabalin with food is not recommended. had a clinically significant effect on the volume of its absorption.
Distribution. Preclinical studies have shown that pregabalin readily crosses the blood-brain barrier in animals, as well as the placenta in rats, and is excreted in milk during lactation. In humans, the conventional volume of distribution of pregabalin after oral administration is approximately 0.56 L/kg. Pregabalin does not bind to plasma proteins.
Metabolism. In humans, pregabalin is slightly metabolized. After a dose of radiolabeled pregabalin is administered, approximately 98% of it is excreted in the urine as unchanged drug. N-methylated pregabalin derivative (the main metabolite of pregabalin, which is determined in urine) constituted 0.9% of the administered dose. Preclinical studies have shown that there is no racemization of the S-enantiomer into the R-enantiomer.
Excretion. Pregabalin is eliminated from the systemic circulation primarily through renal excretion as unchanged drug. The average half-life of pregabalin is 6.3 hours. Plasma and renal clearance of pregabalin are directly proportional to creatinine clearance. Patients with impaired renal function or those on hemodialysis need to adjust the dose of the drug.
Linearity/nonlinearity. The pharmacokinetics of pregabalin are linear over the entire recommended dose range. Intersubject pharmacokinetic variability for pregabalin is low (<20%). Multiple-dose pharmacokinetics are predicted from single-dose data. Thus, there is no need for regular monitoring of pregabalin plasma concentrations.
Pharmacokinetics in selected patient groups
Floor. The results of clinical studies indicate that there is no clinically significant effect of gender on the concentration of pregabalin in blood plasma.
Renal dysfunction. Pregabalin clearance is directly proportional to creatinine clearance. In addition, pregabalin is effectively eliminated from blood plasma during hemodialysis (after 4 hours of hemodialysis, the concentration of pregabalin in blood plasma decreases by approximately 50%). Since the drug is mainly excreted by the kidneys, in patients with impaired renal function it is necessary to reduce its dose, and after hemodialysis, take an additional dose.
Liver dysfunction. No special pharmacokinetic studies have been conducted in patients with liver dysfunction. Because pregabalin is not significantly metabolized and is excreted primarily as unchanged drug in the urine, it is unlikely that hepatic dysfunction would affect pregabalin plasma concentrations.
Elderly patients (over 65 years old). Pregabalin clearance tends to decrease with age. This decrease after oral administration is consistent with the decrease in creatinine clearance also associated with age. Patients with age-related renal impairment may require a reduction in the dose of pregabalin.
Preclinical safety data. In conventional animal safety pharmacology studies, pregabalin was well tolerated when administered at clinically relevant doses. In toxicity studies in rats and monkeys, CNS effects including hypoactivity, hyperactivity and ataxia were noted. An increase in the incidence of retinal atrophy was found, as a rule, in old albino rats after chronic administration of pregabalin at doses more than 5 times higher than the average exposure in humans when used at the maximum recommended clinical doses.
Teratogenicity. Pregabalin was not teratogenic in mice, rats or rabbits. Fetal toxicity in rats and rabbits was observed only at exposures significantly higher than in humans. In a prenatal/postnatal toxicity study, pregabalin caused developmental toxicity in rat offspring at doses greater than 2 times the maximum recommended human exposure.
Mutagenicity. Based on in vitro and in vivo assays, pregabalin is not genotoxic.
Carcinogenicity. A 2-year study of the carcinogenicity of pregabalin was conducted in rats and mice. The development of tumors was not observed in rats when the drug was administered in doses 24 times higher than the average exposure in humans, when used at the maximum recommended clinical dose of 600 mg/day. In mice, there was no increase in the incidence of tumor development at exposures similar to the average exposure in humans, but an increase in the incidence of hemangiosarcoma was noted at higher doses. The nongenotoxic mechanism of pregabalin-induced tumor development in mice involved platelet changes and corresponding endothelial cell proliferation. In short-term studies and limited data from long-term studies, such changes in platelets have not been detected in either rats or humans. There is no evidence to suggest a risk to humans associated with this.
In young rats, the types of toxicity were not qualitatively different from those detected in adult animals, although young rats are more sensitive. During therapeutic exposures, clinical signs of hyperactivity and bruxism on the part of the central nervous system and some developmental changes (temporary inhibition of body weight gain) were noted. The effect on the period of estrus was detected when using doses 5 times higher than the therapeutic exposure in humans. Neurobehavioral/cognitive effects were observed in young rats 1–2 weeks after exposure to 2 times (response to acoustic stimulus) or 5 times (learning/memory) the human therapeutic exposure. A decrease in the response to an acoustic stimulus was noted in young rats 1–2 weeks after administration at doses 2 times higher than therapeutic doses for humans. After 9 weeks this phenomenon was not observed.
Neogabine instructions for use
COMPOSITION AND RELEASE FORM Caps. 75 mg blister, No. 30, No. 60 Caps. 150 mg blister, No. 30, No. 60 Active ingredient - pregabalin 75 mg or 150 mg. Pharmacodynamics The active substance, pregabalin, is an analogue of GABA ((S)-3-(aminomethyl)-5-methylhexanoic acid). Mechanism of action. Pregabalin binds to the auxiliary subunit (α2-δ protein) of voltage-gated calcium channels in the central nervous system, actively replacing [3H]-gabapentin. Clinical studies have demonstrated the effectiveness of pregabalin in neuropathic pain, fibromyalgia, epilepsy and generalized anxiety disorders.
Pharmacokinetics The pharmacokinetics of pregabalin were similar in healthy volunteers, patients with epilepsy using antiepileptic drugs, and individuals with chronic pain. Absorption. Pregabalin is rapidly absorbed when administered orally on an empty stomach and reaches Cmax in blood plasma within 1 hour after single or multiple doses. The estimated oral bioavailability of pregabalin is ≥90% and is independent of dose. After repeated administration, steady state is achieved within 24–48 hours. The extent of absorption of pregabalin is reduced when administered concomitantly with food, resulting in a decrease in Cmax by approximately 25–30% and Tmax by approximately 2.5 hours. However, administration of pregabalin with food is not recommended. had a clinically significant effect on the degree of its absorption. Distribution. Preclinical studies have established that pregabalin easily penetrates the BBB in animals, as well as the placenta in rats, and is excreted in milk during lactation. In humans, the conventional volume of distribution of pregabalin after oral administration is approximately 0.56 L/kg body weight. Pregabalin does not bind to plasma proteins. Metabolism. In humans, pregabalin is slightly metabolized. After a dose of radiolabeled pregabalin is administered, approximately 98% of it is excreted in the urine as unchanged drug. N-methylated pregabalin derivative (the main metabolite of pregabalin, which is determined in urine) constituted 0.9% of the administered dose. Preclinical studies have shown that there is no racemization of the S-enantiomer to the R-enantiomer. Excretion. Pregabalin is eliminated from the systemic circulation primarily through renal excretion as unchanged drug. The average half-life of pregabalin is 6.3 hours. Plasma and renal clearance of pregabalin are directly proportional to creatinine clearance. Patients with impaired renal function or those on hemodialysis need to adjust the dose of the drug (see APPLICATION). Linearity/nonlinearity. The pharmacokinetics of pregabalin are linear over the entire recommended dose range. Intersubject pharmacokinetic variability for pregabalin is low (<20%). Multiple-dose pharmacokinetics are predicted from single-dose data. Thus, there is no need for regular monitoring of pregabalin plasma concentrations. Pharmacokinetics in certain groups of patients Gender. The results of clinical studies indicate that there is no clinically significant effect of gender on the concentration of pregabalin in blood plasma. Renal dysfunction. Pregabalin clearance is directly proportional to creatinine clearance. In addition, pregabalin is effectively eliminated from blood plasma during hemodialysis (after 4 hours of hemodialysis, the concentration of pregabalin in blood plasma decreases by approximately 50%). Since the drug is mainly excreted by the kidneys, in patients with impaired renal function it is necessary to reduce its dose, and after hemodialysis, take an additional dose. Liver dysfunction. No specific pharmacokinetic studies have been conducted in patients with impaired liver function. Because pregabalin is not significantly metabolized and is excreted primarily as unchanged drug in the urine, it is unlikely that hepatic dysfunction would affect pregabalin plasma concentrations.
INDICATIONS Neuropathic pain in adults with damage to the peripheral and central nervous system; epilepsy (as a means of additional therapy for partial convulsive seizures in adults with/without secondary generalization); generalized anxiety disorder in adults; fibromyalgia.
APPLICATION The drug is prescribed at a dose of 150–600 mg/day, divided into 2 or 3 doses. The medicine can be used regardless of food intake. Neuropathic pain. The initial dose of pregabalin is 150 mg/day. Depending on the patient’s individual response and tolerability of the drug, the dose can be increased after 3–7 days to 300 mg/day and, if necessary, to the maximum (600 mg/day) after another 7 days. Fibromyalgia. Typically, the dose of the drug for most patients is 300–450 mg/day, divided into 2 doses. For some patients, a dose of 600 mg/day may be necessary. The drug should be started with a dose of 75 mg 2 times a day (150 mg/day) and increased, depending on effectiveness and tolerability, to 150 mg 2 times a day (300 mg/day) for 1 week. For patients in whom dosing of 300 mg/day is not effective enough, the dose can be increased to 225 mg 2 times a day (450 mg/day). If necessary, you can increase it after another week to a maximum of 600 mg/day. Epilepsy. The initial dose of pregabalin is 150 mg/day. Depending on the patient's individual response and tolerability of the drug, the dose can be increased to 300 mg/day after 1 week. After another 1 week - up to a maximum of 600 mg / day. Generalized anxiety disorders. The daily dose varies between 150–600 mg, divided into 2 or 3 doses. The need for pregabalin treatment should be reviewed regularly. Pregabalin therapy can be started at a dose of 150 mg/day. Depending on the individual response and tolerability of the drug, the dose can be increased to 300 mg/day after the 1st week of treatment. Over the next week, the dose can be increased to 450 mg/day. After another 1 week - up to a maximum of 600 mg / day. Discontinuation of the drug. If pregabalin must be discontinued, it is recommended to gradually discontinue the drug over at least 1 week. Patients with impaired renal function. Reducing the dose of the drug in patients with impaired renal function should be carried out individually, taking into account creatinine clearance (CLcr), as indicated in Table. 1, which is determined by the formula: CLcr (ml/min) = ([140 - age (years)] × body weight (kg)/72 × serum creatinine level (mg/dl)) × (0.85 - for women). In patients undergoing hemodialysis, the daily dose of pregabalin should be adjusted based on renal function. In addition to the daily dose, a dose of the drug should be taken immediately after a 4-hour hemodialysis procedure (Table 1). Table 1. Dose adjustment of pregabalin taking into account the state of renal function Creatinine clearance, ml/min Total daily dose of pregabalin* Dosage regimen Initial dose, mg/day Maximum dose, mg/day ≥60 150 600 2 or 3 times a day ≥30–< 60 75 300 2 or 3 times a day ≥15–<30 25–50 150 1 or 2 times a day <15 25 75 1 time a day Additional daily dose after hemodialysis, mg 25 100 Single dose+ *Total daily dose (mg /day) must be divided by the number of doses to obtain the number of milligrams per dose. +Additional dose - a single additional dose. Patients with impaired liver function. In patients with impaired liver function, no dose adjustment is required. Use in elderly patients (over 65 years of age). In elderly patients, a dose reduction of pregabalin may be necessary due to decreased renal function.
CONTRAINDICATIONS Hypersensitivity to the active substance or any of the auxiliary components.
SIDE EFFECTS The most common adverse reactions were dizziness and drowsiness. Adverse reactions reported with the use of pregabalin are listed below according to the classification of organs and systems indicating their frequency: very often (≥1/10), often (≥1/100-<1/10), infrequently (≥1/1000 –<1/100), isolated (≥1/10,000–<1/1000), very rare (<1/10,000), frequency unknown (cannot be estimated from the available data). The listed adverse reactions may also be associated with the underlying disease and/or concomitant medications. Infections and infestations: uncommon - nasopharyngitis. From the blood and lymphatic system: isolated - neutropenia. From the immune system: frequency unknown - hypersensitivity, angioedema, allergic reaction. Metabolic and metabolic disorders: often - increased appetite; infrequently - anorexia, hypoglycemia. From the mental side: often - confusion, disorientation, irritability, euphoria, decreased libido, insomnia; uncommon - depersonalization, anorgasmia, anxiety, depression, agitation, mood changes, depressed mood, difficulty finding words, hallucinations, pathological dreams, increased libido, panic attacks, apathy; single - disinhibition, high spirits, mania, delirium, manic reactions, paranoid reactions; frequency unknown - aggression, mental disorders. From the nervous system: very often - dizziness, drowsiness; often - ataxia, impaired coordination, impaired balance, attention disorders, memory impairment, tremor, dysarthria, paresthesia, sedation, lethargy, headache, lethargy; uncommon - impaired cognitive function, hypoesthesia, nystagmus, speech impairment, myoclonus, hyporeflexia, dyskinesia, psychomotor hyperactivity, postural dizziness, hyperesthesia, amnesia, ageusia, heartburn, intention tremor, stupor, fainting, perioral paresthesia, hypalgesia; single - hypokinesia, parosmia, dysgraphia, dependence, cerebellar syndrome, cogwheel syndrome, coma, encephalopathy, extrapyramidal symptoms, Guillain-Barre syndrome, intracranial hypertension, sleep disorders; frequency unknown - convulsions, poor health. From the organ of vision: often - blurred vision, diplopia, conjunctivitis; uncommon - visual impairment, visual field defect, dry eyes, eye swelling, decreased visual acuity, eye pain, asthenopia, increased lacrimation, impaired accommodation, blepharitis, hemorrhage in the eyeball, photosensitivity, retinal edema; isolated - photopsia, eye irritation, mydriasis, oscillopsia, changes in visual depth perception, loss of peripheral vision, strabismus, visual brightness, anisocoria, corneal ulcers, exophthalmos, ocular muscle paralysis, iritis, keratoconjunctivitis, miosis, night blindness, ophthalmoplegia, optic atrophy , papilledema, ptosis, uveitis; frequency unknown - loss of vision, keratitis. From the organ of hearing and vestibular apparatus: often - vertigo; infrequently - hyperacusis. From the heart: infrequently - first degree blockade, tachycardia; single - sinus tachycardia, sinus arrhythmia, sinus bradycardia; frequency unknown - congestive heart failure, prolongation of the QT interval. From the vascular system: infrequently - arterial hypotension/hypertension, flushes of blood, hot flashes; isolated - a feeling of coldness in the extremities. From the respiratory system, chest and mediastinal organs: infrequently - shortness of breath, dry nasal mucosa; single - nasal congestion, nosebleeds, rhinitis, snoring, tightness in the throat, cough, laryngospasm, pharyngolaryngeal pain, apnea, atelectasis, bronchiolitis, hiccups, pulmonary fibrosis, yawning; frequency unknown - pulmonary edema. From the digestive system: often - vomiting, constipation, dry mouth, flatulence, gastroenteritis; uncommon - abdominal bloating, excessive salivation, gastroesophageal reflux disease, oral hypoesthesia, cholecystitis, cholelithiasis, colitis, gastrointestinal bleeding, melena, swelling of the tongue, rectal bleeding; single - ascites, dysphagia, pancreatitis, stomatitis, esophageal ulcer, periodontal abscesses; frequency unknown - diarrhea, nausea. From the skin and subcutaneous tissue: uncommon - increased sweating, rash, bedsores, alopecia, dry skin, eczema, hirsutism, skin ulcers, vesiculobullous rash; single - cold sweat, urticaria, exfoliative dermatitis, lichenoid dermatitis, melanosis, nail lesions, petechial rash, purpura, pustular rash, skin atrophy, skin necrosis, skin and subcutaneous nodules; frequency unknown - Stevens-Johnson syndrome, itching. From the musculoskeletal system and connective tissue: infrequently - muscle twitching, joint swelling, muscle spasms, myalgia, arthralgia, back pain, pain in the limbs, muscle stiffness; isolated - spasms in the neck, neck pain, rhabdomyolysis. From the urinary system: infrequently - dysuria, urinary incontinence, albuminuria, hematuria, formation of kidney stones, nephritis; single - oliguria, renal failure, acute renal failure, glomerulonephritis, pyelonephritis; frequency unknown - urinary retention. From the reproductive system and mammary glands: often - erectile dysfunction, impotence; uncommon - delayed ejaculation, sexual dysfunction, leukorrhea, menorrhagia, metrorrhagia; single - amenorrhea, pain in the mammary glands, discharge from the mammary glands, dysmenorrhea, hypertrophy of the mammary glands, cervicitis, balanitis, epididymitis; frequency unknown - gynecomastia. General disorders: often - peripheral edema, edema, gait disturbances, feeling of intoxication, fatigue; uncommon - falling, feeling of constriction in the chest, pain, chills, malaise, asthenia, thirst, abscess, phlegmon, photosensitivity; single - generalized edema, pyrexia, anaphylactoid reactions, granuloma, intentional harm, retroperitoneal fibrosis, shock; frequency unknown - facial swelling. Laboratory indicators: often - increase in body weight; infrequently - increased ALT levels, increased CPK levels in the blood, increased AST levels, decreased platelet counts; single - increased glucose levels, increased creatinine levels in the blood, decreased potassium levels in the blood, decreased body weight, decreased leukocyte levels. After stopping short- and long-term treatment with pregabalin, some patients experienced withdrawal symptoms. The following reactions have been reported: insomnia, headache, nausea, anxiety, diarrhea, flu-like syndrome, convulsions, nervousness, depression, pain, increased sweating and dizziness. The patient must be informed about this at the beginning of therapy. Regarding the withdrawal of pregabalin after long-term treatment, there is no data on the frequency and severity of withdrawal symptoms depending on the duration of use and dose of the drug.
SPECIAL INSTRUCTIONS Patients with diabetes mellitus. According to current clinical practice, some patients with diabetes mellitus whose body weight has increased while using pregabalin may require dosage adjustment of hypoglycemic drugs. Hypersensitivity reactions. Hypersensitivity reactions, including cases of angioedema, have been reported. Pregabalin should be discontinued immediately if symptoms of angioedema such as swelling of the face, perioral area or upper respiratory tract occur. Dizziness, drowsiness, loss of consciousness, confusion and mental disorders. Pregabalin use has been associated with cases of dizziness and drowsiness, which may increase the incidence of accidental injuries (falls) in older adults. Loss of consciousness, confusion, and mental disturbances have also been reported. Therefore, patients should be advised to use caution until they are aware of the possible effects of the drug. Visual impairment. Temporary blurred vision and other vision changes have been reported in patients receiving pregabalin. In most cases, this phenomenon disappeared with continuous use of pregabalin. In clinical studies in which ophthalmologic examination was performed, the incidence of decreased visual acuity and visual field changes was higher in patients receiving pregabalin than in patients receiving placebo; the incidence of changes in the fundus was higher in the placebo group. Eye side effects have also been reported, including loss of vision, blurred vision, or other changes in visual acuity, most of which were temporary. Discontinuation of pregabalin may help resolve or reduce these symptoms. Discontinuation of concomitant antiepileptic drugs. There is insufficient data regarding discontinuation of concomitant antiepileptic drugs after seizure control is achieved when pregabalin is added to existing treatment to allow conversion to pregabalin monotherapy. Withdrawal symptoms. After stopping short- and long-term use of pregabalin, some patients experience withdrawal symptoms (see ADVERSE EFFECTS). Seizures, particularly status epilepticus and grand mal seizures, may occur during treatment with pregabalin or shortly after discontinuation of pregabalin use. Kidney failure. Cases of renal failure have been reported. Although the effect of drug discontinuation on the recurrence of symptoms of renal failure has not been systematically studied, improvements in renal function have been reported following drug discontinuation or pregabalin dose reduction. Congestive heart failure. Cases of congestive heart failure have been reported in patients using pregabalin. This reaction has frequently occurred when pregabalin was used to treat neuropathic pain in elderly patients with cardiovascular disease. Pregabalin should be used with caution in such patients. This phenomenon may disappear when you stop taking pregabalin. Treatment of neuropathic pain of central origin due to spinal cord lesions. During treatment of central neuropathic pain due to spinal cord injury, the incidence of overall adverse reactions, CNS adverse reactions, and especially somnolence was increased. This may be explained by the additive effect of other drugs (eg antispastic drugs) needed to treat this condition. This circumstance must be taken into account when pregabalin is prescribed to such patients. Suicidal thoughts and behavior. Suicidal ideation and behavior were recorded in patients receiving antiepileptic drugs for specific indications. A meta-analysis of randomized placebo-controlled trials of antiepileptic drugs also showed a slightly increased risk of suicidal ideation and behavior. The mechanism by which this risk occurs is unknown, and available data do not exclude its existence with pregabalin use. Therefore, it is necessary to closely monitor the patient for suicidal ideation and behavior and institute appropriate treatment if it occurs. Patients (and their caregivers) should be aware of the need to seek medical help if suicidal ideation or behavior occurs. Deterioration of the function of the lower digestive tract. Lower gastrointestinal tract dysfunction (eg, ileus, paralytic ileus, constipation) has been reported as a result of taking pregabalin with drugs that may cause constipation, such as opioid analgesics. When using pregabalin and opioids in combination, measures should be taken to prevent constipation (especially in women and elderly patients). Addictive potential. Cases of abuse have been reported. The drug should be prescribed with caution to patients with a history of drug addiction. Patients should be monitored for symptoms of pregabalin dependence. Encephalopathy. Cases of encephalopathy have occurred predominantly in patients with concomitant diseases that can cause encephalopathy. Elderly patients (over 65 years old). Pregabalin clearance tends to decrease with age. This decrease in pregabalin clearance after oral administration is consistent with the age-related decrease in creatinine clearance. Patients with age-related renal impairment may require a reduced dose of pregabalin (see USAGE). In elderly patients, adverse reactions such as dizziness, confusion, tremor, loss of coordination, and lethargy may occur more frequently.
Use during pregnancy and lactation Pregnancy. There are no data regarding the use of pregabalin during pregnancy. Animal studies indicate reproductive toxicity. The potential risk to humans is unknown. Therefore, pregabalin should not be used during pregnancy, except in certain cases when the benefit to the mother clearly outweighs the possible risk to the fetus. Women of childbearing age need to use effective contraception. Lactation. It is unknown whether pregabalin is excreted into human breast milk, but it is detected in rat milk. Therefore, breastfeeding during treatment with pregabalin is not recommended. Reproductive function. There is no clinical data on the effect of pregabalin on the reproductive function of women.
Male Fertility The effect of pregabalin on sperm motility was studied in healthy male volunteers receiving a dose of 600 mg/day of pregabalin. After 3 months of treatment, no effect on sperm motility was detected.
Children The safety and effectiveness of pregabalin in children under 18 years of age have not been established.
Effect on reaction speed when driving vehicles or operating machinery The drug may cause dizziness and drowsiness, and may also affect the ability to drive vehicles or operate machinery. Therefore, patients should refrain from driving or operating complex machinery until it is known exactly how the drug affects the ability to do such activities.
INTERACTIONS Since the drug is predominantly excreted unchanged in the urine and is only slightly metabolized in humans (<2% of the dose is excreted in the urine as metabolites), does not inhibit the in vitro metabolism of other drugs and does not bind to blood proteins, it is unlikely that pregabalin may enter into pharmacokinetic interactions with other drugs or be subject to such interactions. In vivo studies and population pharmacokinetic analysis. In in vivo studies, no significant clinical pharmacokinetic interactions were observed between pregabalin and phenytoin, carbamazepine, valproic acid, lamotrigine, gabapentin, lorazepam, oxycodone, or ethanol. A population pharmacokinetic analysis showed that oral antidiabetic drugs, diuretics, insulin, phenobarbital, tiagabine and topiramate did not have a clinically significant effect on the clearance of pregabalin. Oral contraceptives, norethisterone and/or ethinyl estradiol. The simultaneous use of pregabalin and oral contraceptives - norethisterone and/or ethinyl estradiol - does not affect the steady-state pharmacokinetics of either drug. Medicines that affect the central nervous system. Pregabalin may potentiate the effect of ethanol and lorazepam. In controlled clinical studies, multiple oral doses of pregabalin and oxycodone, lorazepam, or ethanol did not have a clinically significant effect on respiratory function. In clinical practice, respiratory failure and coma have been reported in patients taking pregabalin and other CNS depressants concomitantly. Pregabalin increased the cognitive and gross motor impairment caused by oxycodone. Interactions in elderly patients. No specific studies of pharmacodynamic interactions have been conducted in elderly patients.
OVERDOSE The most common adverse reactions reported in cases of pregabalin overdose were drowsiness, confusion, agitation and restlessness. Cases of coma have been reported occasionally. Treatment of pregabalin overdose should include general supportive measures and, if necessary, hemodialysis.
STORAGE CONDITIONS In original packaging at a temperature not exceeding 25 °C.
Dosage
the drug is prescribed at a dose of 150–600 mg/day, divided into 2 or 3 doses. The medicine can be used regardless of food intake.
Neuropathic pain. The initial dose of pregabalin is 150 mg/day. Depending on the patient’s individual response and tolerability of the drug, the dose can be increased after 3–7 days to 300 mg/day and, if necessary, to the maximum (600 mg/day) after another 7 days.
Fibromyalgia. Typically, the dose of the drug for most patients is 300–450 mg/day, divided into 2 doses. For some patients, a dose of 600 mg/day may be necessary. The drug should be started with a dose of 75 mg 2 times a day (150 mg/day) and increased, depending on effectiveness and tolerability, to 150 mg 2 times a day (300 mg/day) for 1 week. For patients in whom dosing of 300 mg/day is not effective enough, the dose can be increased to 225 mg 2 times a day (450 mg/day). If necessary, you can increase it after another week to a maximum of 600 mg/day.
Epilepsy. The initial dose of pregabalin is 150 mg/day. Depending on the patient's individual response and tolerability of the drug, the dose can be increased to 300 mg/day after 1 week. After another 1 week - up to a maximum of 600 mg / day.
Generalized anxiety disorders. The daily dose varies between 150–600 mg, divided into 2 or 3 doses. The need for pregabalin treatment should be reviewed regularly.
Pregabalin therapy can be started at a dose of 150 mg/day. Depending on the individual response and tolerability of the drug, the dose can be increased to 300 mg/day after the 1st week of treatment. Over the next week, the dose can be increased to 450 mg/day. After another 1 week, up to a maximum of 600 mg/day.
Discontinuation of the drug. If pregabalin must be discontinued, it is recommended to gradually discontinue the drug over at least 1 week.
Patients with impaired renal function. Reducing the dose of the drug in patients with impaired renal function should be carried out individually, taking into account CLcr, as indicated in Table 1, which is determined by the formula:
CLcr (ml/min) = ([140 - age (years)] × body weight (kg)/72 × serum creatinine level (mg/dl)) × (0.85 - for women).
In patients undergoing hemodialysis, the daily dose of pregabalin should be increased taking into account renal function. In addition to the daily dose, a dose of the drug should be taken immediately after a 4-hour hemodialysis procedure (Table 1).
Table 1 Pregabalin dose adjustment based on renal function
| Creatinine clearance, ml/min | Total daily dose of pregabalin* | Dosage regimen | |
| Initial dose, mg/day | Maximum dose, mg/day | ||
| ≥60 | 150 | 600 | 2 or 3 times a day |
| ≥30–<60 | 75 | 300 | 2 or 3 times a day |
| ≥15–<30 | 25–50 | 150 | 1 or 2 times a day |
| <15 | 25 | 75 | 1 time per day |
| Additional daily dose after hemodialysis, mg | |||
| 25 | 100 | Single dose+ | |
*The total daily dose (mg/day) must be divided by the number of doses to obtain the number of milligrams per dose.
+Additional dose - a single additional dose.
Patients with impaired liver function. In patients with impaired liver function, no dose adjustment is required.
Use in elderly patients (over 65 years old). In elderly patients, a dose reduction of pregabalin may be necessary due to decreased renal function.
Side effects
The most frequently reported side effects were dizziness and drowsiness. Side effects when using the drug were most often mild or moderate. In all controlled studies, the rate of drug discontinuation due to adverse reactions was 14% among patients who received pregabalin and 7% among patients who received placebo. The most common adverse reactions that led to exclusion from the pregabalin group were dizziness and drowsiness.
Selected adverse reactions associated with the use of pregabalin, according to an analysis of cumulative clinical trial data, are listed by organ system class and frequency: very common (>1/100), common (>1/100, <1/10), uncommon (>1 /1000, <1/100) and rarely (<1/1000).
The occurrence of these side effects could be associated with the course of the underlying disease or the concomitant use of other drugs.
Table 2 Adverse reactions observed in clinical studies
| Body systems | Adverse reaction to the drug |
| Infections and infestations | |
| Infrequently | Nasopharyngitis |
| From the blood and lymphatic system | |
| Rarely | Neutropenia |
| Metabolism and nutrition | |
| Often | Increased appetite |
| Infrequently | Anorexia |
| Rarely | Hypoglycemia |
| From the mental side | |
| Often | Confusion, disorientation, irritability, euphoria, decreased libido, insomnia |
| Infrequently | Depersonalization, anorgasmia, anxiety, depression, agitation, mood changes, difficulty finding words, hallucinations, unusual dreams, increased libido, panic attacks, apathy |
| Rarely | Looseness, high spirits |
| From the nervous system | |
| Often | Dizziness, drowsiness |
| Often | Ataxia, incoordination, imbalance, amnesia, attention disorders, memory impairment, tremor, dysarthria, paresthesia, sedation, lethargy |
| Infrequently | Impaired cognitive function, hypoesthesia, nystagmus, speech impairment, myoclonus, hyporeflexia, dyskinesia, psychomotor hyperactivity, postural vertigo, hyperesthesia, ageusia, burning sensation, intention tremor, stupor, syncope |
| Rarely | Hypokinesia, parosmia, dysgraphia |
| From the side of the organ of vision | |
| Often | Blurred vision, diplopia |
| Infrequently | Visual impairment, visual field defect, dry eyes, eye swelling, decreased visual acuity, eye pain, asthenopia, increased lacrimation |
| Rarely | Photopsia, eye irritation, mydriasis, oscillopsia, changes in visual depth perception, loss of peripheral vision, strabismus |
| From the organ of hearing and balance | |
| Often | Vertigo |
| Infrequently | Hyperacusis |
| From the side of the heart | |
| Infrequently | 1st degree AV block |
| Rarely | Sinus tachycardia, sinus arrhythmia, sinus bradycardia |
| From the vascular system | |
| Infrequently | Arterial hypotension/hypertension, flushing, hyperemia, feeling of coldness in the extremities |
| From the respiratory system, chest and mediastinum | |
| Infrequently | Shortness of breath, cough, dry nose |
| Rarely | Nasal congestion, nosebleeds, rhinitis, snoring, tightness in the throat |
| From the gastrointestinal tract | |
| Often | Vomiting, bloating, constipation, dry mouth, flatulence |
| Infrequently | Hypersalivation, gastroesophageal reflux, oral hypoesthesia |
| Rarely | Ascites, dysphagia, pancreatitis |
| From the skin and subcutaneous tissue | |
| Infrequently | Increased sweating, rash |
| Rarely | Cold sweat, hives |
| From the musculoskeletal system and connective tissue | |
| Infrequently | Muscle fasciculation, joint swelling, muscle spasms, myalgia, arthralgia, back pain, limb pain, muscle stiffness |
| Rarely | Neck spasms, neck pain, rhabdomyolysis |
| From the kidneys and urinary system | |
| Infrequently | Dysuria, urinary incontinence |
| Rarely | Oliguria, renal failure |
| From the reproductive system and mammary glands | |
| Often | erectile disfunction |
| Infrequently | Delayed ejaculation, sexual dysfunction |
| Rarely | Amenorrhea, breast pain, breast discharge, dysmenorrhea, breast hypertrophy |
| General state | |
| Often | Peripheral edema, falls, swelling, gait disturbance, feeling drunk, unusual sensations, fatigue |
| Infrequently | Sensation of chest compression, generalized edema, pain, chills, asthenia, thirst |
| Rarely | Pyrexia |
| Laboratory indicators | |
| Often | Weight gain |
| Infrequently | Increased levels of ALT, CPK in the blood, AST, decreased platelet count |
| Rarely | Increased levels of glucose, creatinine in the blood, decreased levels of potassium in the blood, decreased body weight, decreased levels of leukocytes |
The following adverse reactions have been reported during post-marketing surveillance:
from the immune system: angioedema, allergic reactions, hypersensitivity;
from the nervous system: headache, loss of consciousness, deterioration of mental activity;
from the psyche: aggression;
from the heart: congestive heart failure, prolongation of the QT interval;
from the organ of vision: keratitis, loss of vision;
from the gastrointestinal tract: swelling of the tongue, diarrhea, nausea;
general condition and changes at the injection site: malaise;
from the skin and subcutaneous tissue: facial swelling, itching, Stevens-Johnson syndrome;
from the kidneys and urinary system: urinary retention;
from the respiratory system and chest: pulmonary edema.
After stopping short-term and long-term treatment with pregabalin, some patients experienced withdrawal symptoms. The following reactions were reported: insomnia, headache, nausea, diarrhea, flu-like syndrome, nervousness, depression, pain, sweating and dizziness. The patient must be informed about this at the beginning of therapy.
With regard to discontinuation of pregabalin after long-term treatment, there are no data regarding the frequency and severity of withdrawal symptoms depending on the duration of use and dose of the drug.
Neogabin
About the drug
Neogabine is an antiepileptic drug.
Indications and dosage
Indications for the drug Neogabine:
- Neuropathic pain.
The drug is prescribed for the treatment of neuropathic pain in adults with damage to the peripheral and central nervous system.
- Epilepsy.
The drug is prescribed as adjunctive therapy for partial seizures with or without secondary generalization in adults.
- Generalized anxiety disorder.
The drug is prescribed for the treatment of generalized anxiety disorder in adults.
- Fibromyalgia.
Neogabine is prescribed in a dose of 150 to 600 mg per day, divided into 2 or 3 doses. The drug can be used regardless of meals.
Neuropathic pain. The starting dose of pregabalin is 150 mg per day. Depending on the individual patient response and tolerability of the drug, the dose can be increased after 3-7 days to 300 mg per day and, if necessary, increased to a maximum of 600 mg per day after
7 days.
Fibromyalgia.
Of course, the dose for most patients is 300-450 mg per day, divided into 2 doses. For some patients, a dose of 600 mg per day may be required. The drug should be started at a dose of 75 mg 2 times a day (150 mg/day) and can be increased depending on effectiveness and tolerability, up to 150 mg 2 times a day (300 mg/day) for one week. For patients for whom doses of 300 mg/day are not sufficiently effective, the dose can be increased to
225 mg 2 times a day (450 mg/day). If necessary, the dose can be increased after a week to a maximum of 600 mg/day.
Epilepsy. The starting dose of pregabalin is 150 mg per day. Depending on the patient’s individual response and tolerability of the drug, the dose can be increased to 300 mg per day after
1 week. After a week, the dose can be increased to a maximum of 600 mg per day.
Generalized anxiety disorders.
The daily dose varies from 150 to 600 mg in two or three doses. The need for pregabalin treatment should be reviewed regularly.
Treatment with pregabalin can be started at a dose of 150 mg per day. Depending on the individual response and tolerability of the drug, the dose can be increased to 300 mg per day after the first week of treatment. Over the next week of treatment, the dose can be increased to 450 mg per day. After a week, the dose can be increased to a maximum of 600 mg per day.
Oh, Neogabin 150. If pregabalin must be discontinued, it is recommended that the drug be tapered over a period of at least 1 week.
Patients with impaired renal function.
Dose reduction in patients with impaired renal function should be carried out individually, in accordance with the creatinine clearance (CLcr), as indicated in Table 1. CC is determined by the formula:
For patients undergoing hemodialysis, the daily dose of pregabalin should be adjusted according to renal function. In addition to the daily dose, immediately after each 4-hour dialysis procedure, an additional dose of the drug should be used.
Adjust the dose of pregabalin depending on the status of renal function.
Table 1
| CC (CL cr) (ml/min) | Total daily dose of pregabalin * | dosage regimen | |
| Initial dose (Mg/day) | Maximum dose (mg/day) | ||
| ³60 | 150 | 600 | 2 or 3 times a day |
| ³30 — <60 | 75 | 300 | 2 or 3 times a day |
| ³15 — <30 | 25-50 | 150 | 1 or 2 times a day |
| <15 | 25 | 75 | 1 time per day |
| Additional dose after hemodialysis (mg) | |||
| 25 | 100 | Single dose + | |
The total daily dose (mg/day) should be divided by the number of doses to obtain the number of mg per dose.
+ A refill is a one-time additional dose.
Patients with impaired liver function.
There is no need for dose adjustment for patients with impaired liver function.
Use in elderly patients (over 65 years of age).
For elderly patients, it may be necessary to reduce the dose of pregabalin due to decreased renal function.
Overdose
The most commonly reported adverse reactions of Neogabine in cases of pregabalin overdose were drowsiness, confusion, agitation, and restlessness.
Cases of coma have been reported occasionally.
Treatment of pregabalin overdose should include general supportive measures and, if necessary, hemodialysis.
Side effects
Frequent manifestations of adverse reactions of the drug Neogabine were dizziness and drowsiness.
Adverse reactions reported with the use of pregabalin are listed below in the classification of organs and systems indicating their frequency: very often (≥ 1/10), often (≥ 1/100
<1/10), uncommon (≥1/1000 <1/100), rare (≥1/10000 <1/1000), rare (<1/10000), frequency unknown (cannot be estimated from available data).
The listed adverse reactions may also be associated with the underlying disease and/or concomitant medications.
Infections and infestations:
infrequently - nasopharyngitis.
From the blood and lymphatic system:
single cases - neutropenia.
From the immune system:
frequency unknown - hypersensitivity, angioedema, allergic reaction.
Metabolic and metabolic disorders:
often - increased appetite; infrequently - anorexia, hypoglycemia.
From the mental side:
often - confusion, disorientation, irritability, euphoria, decreased libido, insomnia infrequently - depersonalization, anorgasmia, anxiety, depression, agitation, mood changes, depressed mood, difficulty finding words, hallucinations, pathological dreams, increased libido, panic attacks, apathy; single - disinhibition, high spirits, mania, delirium, manic reactions, paranoid reactions, frequency unknown - aggression, mental disorder.
From the nervous system:
very often - dizziness, drowsiness; often - ataxia, impaired coordination, impaired balance, attention disorders, memory impairment, tremor, dysarthria, paresthesia, sedation, lethargy, headache, lethargy; uncommon - impaired cognitive function, hypoesthesia, nystagmus, speech impairment, myoclonus, hyporeflexia, dyskinesia, psychomotor hyperactivity, postural dizziness, hyperesthesia, amnesia, ageusia, burning sensation, intention tremor, stupor, fainting, perioral paresthesia, hypalgesia; isolated - hypokinesia, parosmia, dysgraphia, dependence, cerebellar syndrome, cogwheel syndrome, coma, encephalopathy, extrapyramidal symptoms, Guillain-Barré syndrome, intracranial hypertension, sleep disorders; frequency unknown - convulsions, poor health.
From the side of the organ of vision:
often - blurred vision, diplopia, conjunctivitis uncommon - visual impairment, visual field defect, dry eyes, eye swelling, decreased visual acuity, eye pain, asthenopia, increased lacrimation, accommodation disturbance, blepharitis, hemorrhage in the eyeball, photosensitivity, retinal edema ; isolated - photopsia, eye irritation, mydriasis, oscillopsia, changes in visual depth perception, loss of peripheral vision, strabismus, visual brightness, anisocoria, corneal ulcers, exophthalmos, ocular muscle paralysis, iritis, keratoconjunctivitis, miosis, night blindness, ophthalmoplegia, optic atrophy , papilledema, ptosis, uveitis; frequency unknown - loss of vision, keratitis.
From the hearing and vestibular apparatus:
often - vertigo; infrequently - hyperacusis.
From the heart:
uncommon - first degree block, tachycardia isolated - sinus tachycardia, sinus arrhythmia, sinus bradycardia frequency unknown - congestive heart failure, prolongation of the QT interval.
From the vascular system:
uncommon - arterial hypotension/hypertension, flushes, hot flashes; isolated - a feeling of coldness in the extremities.
From the respiratory system, chest and mediastinal organs:
infrequently - shortness of breath, dry nasal mucosa; single - nasal congestion, nosebleeds, rhinitis, snoring, tightness in the throat, cough, laryngospasm, pharyngolaryngeal pain, apnea, atelectasis, bronchiolitis, hiccups, pulmonary fibrosis, yawning; frequency unknown - pulmonary edema.
From the digestive tract:
often - vomiting, constipation, dry mouth, flatulence, gastroenteritis infrequently - bloating, excess salivation, gastroesophageal reflux disease, oral hypoesthesia, cholecystitis, cholelithiasis, colitis, gastrointestinal bleeding, ground, swelling of the tongue, rectal bleeding single - ascites, dysphagia , pancreatitis, stomatitis, esophageal ulcer, periodontal abscesses; frequency unknown - diarrhea, nausea.
From the skin and subcutaneous tissue:
uncommon - sweating, rash, bedsores, alopecia, dry skin, eczema, hirsutism, skin ulcers, vesicular rash; single - cold sweat, urticaria, exfoliative dermatitis, lichenoid dermatitis, melanosis, nail lesions, petechial rash, purpura, pustular rash, skin atrophy, skin necrosis, skin and subcutaneous nodules; frequency unknown - Stevens-Johnson syndrome, itching.
From the musculoskeletal system and connective tissue:
uncommon - muscle twitching, joint swelling, muscle spasms, myalgia, arthralgia, back pain, pain in the limbs, muscle stiffness; isolated - spasms in the neck, neck pain, rhabdomyolysis.
From the urinary system:
uncommon - dysuria, urinary incontinence, albuminuria, hematuria, kidney stones, nephritis
isolated - oliguria, renal failure, acute renal failure, glomerulonephritis, pyelonephritis; frequency unknown - urinary retention.
From the reproductive system and mammary glands:
often - erectile dysfunction, impotence; infrequently - delayed ejaculation, sexual dysfunction, leukorrhea, menorrhagia, metrorrhagia; isolated - amenorrhea, pain in the mammary glands, discharge from the mammary glands, dysmenorrhea, mammary hypertrophy, cervicitis, balanitis, epididymitis; frequency unknown - gynecomastia.
General violations:
often - peripheral edema, edema, gait disturbances, feeling of intoxication, fatigue; infrequently - falling, feeling of constriction in the chest, pain, chills, malaise, asthenia, thirst, abscess, phlegmon, photosensitivity; isolated - generalized edema, pyrexia, anaphylactoid reactions, granuloma, intentional harm, retroperitoneal fibrosis, shock frequency unknown - facial edema.
Laboratory indicators:
often - weight gain; uncommon - increased alanine aminotransferase levels, increased CPK levels in the blood, increased AST levels, decreased platelet counts; single - increased glucose levels, increased blood creatinine levels, decreased blood potassium levels, decreased body weight, decreased leukocyte levels.
After stopping short-term and long-term treatment with pregabalin, some patients experienced withdrawal symptoms. The following reactions have been reported: insomnia, headache, nausea, anxiety, diarrhea, flu-like syndrome, convulsions, nervousness, depression, pain, sweating and dizziness. The patient must be informed about this at the beginning of therapy.
Regarding the withdrawal of pregabalin after long-term treatment, there are no data on the frequency and severity of withdrawal symptoms depending on the duration of use and dose of the drug.
Contraindications
Contraindications for Neogabine:
Hypersensitivity to the active substance or any of the excipients.
Interaction with other drugs and alcohol
Interaction of the drug Neogabine with other drugs:
Since pregabalin is predominantly excreted unchanged in the urine, undergoes little metabolism in humans (less than 2% of the dose is excreted in the urine as metabolites), does not inhibit in vitro
metabolism of other drugs and does not bind to blood proteins, it is unlikely that pregabalin could lead to or be subject to a pharmacokinetic drug interaction.
In vivo studies and population pharmacokinetic analysis.
In in vivo
no significant clinical pharmacokinetic interactions were observed between pregabalin and phenytoin, carbamazepine, valproic acid, lamotrigine, gabapentin, lorazepam, oxycodone, or ethanol. A population pharmacokinetic analysis showed that oral antidiabetic drugs, diuretics, insulin, phenobarbital, tiagabine, and topiramate do not have a clinically significant effect on the clearance of pregabalin.
Oral contraceptives, norethisterone and/or ethinyl estradiol.
Concomitant use of pregabalin and oral contraceptives norethisterone and/or ethinyl estradiol does not affect the steady-state pharmacokinetics of either drug.
Medicines that affect the central nervous system.
Pregabalin may enhance the effect of ethanol and lorazepam. In controlled clinical studies, concomitant administration of multiple oral doses of pregabalin and oxycodone, lorazepam, or ethanol did not have a clinically significant effect on respiratory function.
In clinical practice, respiratory failure and coma have been reported in patients taking pregabalin and other central nervous system depressants concomitantly. Pregabalin appears to potentiate oxycodone-induced cognitive and gross motor impairment.
Interaction in elderly patients.
Specific pharmacodynamic interaction studies have not been conducted in elderly patients.
Composition and properties
active substance:
pregabalin;
1 capsule contains 75 mg or 150 mg of pregabalin;
Excipients:
microcrystalline cellulose, croscarmellose sodium, magnesium stearate, talc
hard gelatin capsule:
gelatin, titanium dioxide (E 171).
Release form:
Capsules.
Pharmachologic effect:
Pharmacodynamics.
The active ingredient is pregabalin, which is an analogue of gamma-aminobutyric acid
((S)-3-(aminomethyl)-5-methylhexanoic acid).
Mechanism of action.
Pregabalin binds to the auxiliary subunit (a 2 -d-protein) of voltage-gated calcium channels in the central nervous system.
Clinical studies have demonstrated the effectiveness of pregabalin in neuropathic pain, fibromyalgia, epilepsy and generalized anxiety disorders.
Pharmacokinetics.
Steady-state pharmacokinetics of pregabalin were similar in healthy volunteers, patients with epilepsy using antiepileptic drugs, and patients with chronic pain.
Absorption. Pregabalin is rapidly absorbed when taken orally on an empty stomach and reaches maximum plasma concentrations within 1:00 after single and repeated use. The bioavailability of pregabalin when administered orally is calculated to be 90% or more and is independent of dose. After repeated use, an equilibrium state is achieved within 24-48 hours. The rate of absorption of pregabalin is reduced when taken concomitantly with food, resulting in a decrease in maximum concentration (Cmax) by approximately 25-30%, and the time to reach maximum concentration (tmax) slows down by approximately 2.5 hours. However, administration of pregabalin with food did not have a clinically significant effect on the extent of absorption.
Distribution. In preclinical studies, pregabalin has been shown to readily cross the blood-brain barrier in animals, as well as the placenta in rats and is excreted into milk during lactation. In humans, the conventional volume of distribution of pregabalin after oral administration is approximately 0.56 L/kg. Pregabalin does not bind to plasma proteins.
Metabolism. Pregabalin undergoes little metabolism in humans. After administration of a dose of radiolabeled pregabalin, approximately 98% of the radioactive substances are excreted in the urine as unchanged pregabalin. N-methylated pregabalin derivative (the main metabolite of pregabalin, which is determined in urine) amounted to 0.9% of the administered dose. Preclinical studies have shown that there is no racemization of the S-enantiomer into the R-enantiomer.
Conclusion. Pregabalin is excreted from the systemic circulation mainly by the kidneys in unchanged form. The half-life of pregabalin is 6.3 hours. Plasma and renal clearance of pregabalin are directly proportional to creatinine clearance. Patients with impaired renal function or patients undergoing hemodialysis need to adjust the dose of the drug (see Section "Dosage and Administration").
Linearity/nonlinearity. The pharmacokinetics of pregabalin is linear across all recommended doses. Intersubject pharmacokinetic variability for pregabalin is low (less than 20%). The pharmacokinetics of multiple doses are predictable based on single dosing data. Therefore, there is no need to monitor pregabalin plasma concentrations.
Pharmacokinetics in certain groups of patients.
Floor. The results of clinical studies indicate that there is no clinically significant effect of gender on pregabalin plasma concentrations.
Renal dysfunction. Pregabalin clearance is directly proportional to creatinine clearance. In addition, pregabalin is effectively removed from plasma during hemodialysis (after 4 hours of hemodialysis, pregabalin plasma concentrations are reduced by approximately 50%). Since renal excretion is the main route of elimination of pregabalin, patients with impaired renal function should reduce the dose of the drug, and after hemodialysis, take an additional dose.
Liver dysfunction. Specific pharmacokinetic studies have not been conducted in patients with impaired liver function. Since pregabalin does not undergo significant metabolism and is excreted primarily unchanged in the urine, it is unlikely that hepatic impairment would significantly affect pregabalin plasma concentrations.
Storage conditions:
Neogabine should be stored out of the reach of children, in its original packaging at a temperature not exceeding 25 ° C.
general information
- Sales form:
on prescription
- Current issue:
Pregabalin
- Manufacturer:
Pharma Start, LLC, Kiev, Ukraine
special instructions
During post-marketing observations, there have been reports of hypersensitivity reactions, including cases of angioedema. Pregabalin should be discontinued immediately if symptoms of angioedema such as swelling of the face, perioral area or upper respiratory tract occur.
Pregabalin use has been associated with cases of dizziness and drowsiness, which may increase the incidence of accidental injuries (falls) in older adults. Post-marketing reports of loss of consciousness, confusion, and deterioration of mental performance have been received. Therefore, patients should be advised to use caution until they are aware of the possible effects of the drug.
In post-marketing surveillance, temporary blurred vision and other visual changes have been reported in patients receiving pregabalin. After discontinuation of the drug, such symptoms may disappear or weaken. In clinical studies in which ophthalmologic examination was performed, the incidence of decreased visual acuity and visual field changes was higher in patients receiving pregabalin than in patients receiving placebo; the incidence of changes in the fundus was higher in the placebo group. Ocular side effects, including loss of vision, blurred vision, or other changes in visual acuity, most of which were temporary, were also reported during post-marketing surveillance. Discontinuation of pregabalin may help resolve or reduce these symptoms.
There is insufficient data regarding discontinuation of concomitant antiepileptic drugs once seizure control is achieved when pregabalin is added to existing treatment to allow transition to pregabalin monotherapy.
After discontinuation of short- and long-term use of pregabalin, some patients experienced withdrawal symptoms. The following effects have been reported: insomnia, headache, nausea, anxiety and diarrhea.
Although the effect of drug discontinuation on return of symptoms of renal failure has not been systematically studied, improvements in renal function have been reported following drug discontinuation or pregabalin dose reduction.
Although no causal relationship has been established between the use of pregabalin and congestive heart failure, cases of congestive heart failure have been reported in post-marketing experience in patients using pregabalin. In short-term studies in patients without clinically significant cardiac or peripheral vascular disease, there was no significant association between peripheral edema and cardiovascular complications such as hypertension or congestive heart failure. Since there is insufficient data on the use of the drug in patients with severe congestive heart failure, pregabalin should be used with caution in them.
During treatment of central neuropathic pain due to spinal cord injury, the incidence of overall adverse reactions, CNS adverse reactions, and especially somnolence was increased. This may be explained by the additive effect of other drugs (eg antispastic drugs) needed to treat this condition. This circumstance must be taken into account when pregabalin is prescribed to such patients.
Suicidal ideation and behavior have been observed in patients receiving antiepileptic drugs for certain indications. A meta-analysis of randomized placebo-controlled trials of antiepileptic drugs also showed a slightly increased risk of suicidal ideation and behavior. The mechanism by which this risk occurs is unknown, and available data do not exclude its existence with pregabalin use.
Therefore, it is necessary to closely monitor the patient for suicidal ideation and behavior and institute appropriate treatment if it occurs. Patients (and their caregivers) should be aware of the need to seek medical help if suicidal ideation or behavior occurs.
Use during pregnancy and lactation
Pregnancy. There are no data regarding the use of pregabalin during pregnancy. Animal studies indicate reproductive toxicity. The potential risk to humans is unknown. Therefore, pregabalin should not be used during pregnancy, except in certain cases when the benefit to the mother clearly outweighs the possible risk to the fetus. Women of childbearing age need to use effective contraception.
Lactation. It is unknown whether pregabalin is excreted into breast milk, but it is detected in the milk of rats. Therefore, breastfeeding during treatment with pregabalin is not recommended.
Children. The safety and effectiveness of pregabalin in children under 12 years of age and adolescents have not been studied. It is not recommended to use the drug in children.
Influence on reaction speed when driving vehicles or working with other mechanisms. The drug may cause dizziness and drowsiness and may affect your ability to drive or operate machinery. Therefore, patients should refrain from driving or operating complex machinery until it is known exactly how the drug affects the ability to do such activities.
Neogabine capsules 75 mg No. 10x3
Name
Neogabin
Description
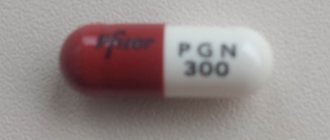
Hard gelatin capsules, white; the contents of the capsules are white or almost white powder; The presence of compressed columns or lumps is allowed, which disintegrate when pressed.
Main active ingredient
Pregabalin
Release form
capsules
Dosage
75 mg
Indications for use
treatment of neuropathic pain in adults with damage to the peripheral and central nervous system; as adjunctive therapy for partial seizures with or without secondary generalization in adults; Treatment of generalized anxiety disorder in adults.
Directions for use and doses
The drug is prescribed in a dose of 150 to 600 mg/day, divided into 2 or 3 doses. The drug can be used regardless of meals. Neogabine is intended for oral use only. Neuropathic pain The initial dose of pregabalin is 150 mg/day, divided into 2 or 3 doses. Depending on the patient's individual response and tolerability of the drug, the dose can be increased after 3-7 days to 300 mg/day and, if necessary, increased to a maximum dose of 600 mg/day after another 7 days. Epilepsy The initial dose of pregabalin is 150 mg/day, divided into 2 or 3 doses. Depending on the patient's individual response and tolerability of the drug, the dose can be increased to 300 mg/day after 1 week. After another week, the dose can be increased to a maximum of 600 mg/day. Generalized anxiety disorder The daily dose varies from 150 to 600 mg, divided into 2 or 3 doses. The need for pregabalin treatment should be reviewed regularly. Treatment with pregabalin can be started at a dose of 150 mg/day. Depending on the individual response and tolerability of the drug, the dose can be increased to 300 mg/day after the first week of treatment. Over the next week of treatment, the dose can be increased to 450 mg/day. After another week, the dose can be increased to a maximum of 600 mg/day. Discontinuation of the drug If pregabalin is to be discontinued, it is recommended to gradually discontinue the drug over at least 1 week. Patients with impaired renal function Dose reduction in patients with impaired renal function must be carried out individually, in accordance with the creatinine clearance (CLcr), as indicated in table 1. Creatinine clearance is determined by the formula: CLcr (ml/min) = 1.23×
140-age (years)
×weight (kg)/creatinine level in blood plasma (μmol/l) For women, multiply the resulting figure by 0.85. Pregabalin is effectively eliminated from blood plasma by dialysis (50% within 4 hours). For patients undergoing hemodialysis, the daily dose of pregabalin should be adjusted depending on renal function. In addition to the daily dose, immediately after each 4-hour dialysis procedure, it is necessary to apply an additional dose of the drug. Table 1. Pregabalin dose adjustment based on renal function Creatinine clearance (CLcr) (ml/min) Total daily dose of pregabalin* Dosage regimen Initial dose (mg/day) Maximum dose (mg/day) ≥60 150 600 2 or 3 times/day ≥30–
Use during pregnancy and lactation
Pregnancy There are no data regarding the use of pregabalin in pregnant women. There is evidence from animal studies that suggests reproductive toxicity. The potential risk to humans is unknown. Therefore, pregabalin should not be used during pregnancy, except in certain cases when the benefit to the mother clearly outweighs the possible risk to the fetus. Women of reproductive age need to use effective contraception. Breastfeeding Period It is known that small amounts of pregabalin have been detected in the milk of women who are breastfeeding. Therefore, breastfeeding is not recommended during treatment with pregabalin. Fertility There is no clinical information regarding the effect of pregabalin on the reproductive function of women. There is evidence of the effect of pregabalin on sperm motility, which was studied in healthy male volunteers who received a dose of pregabalin 600 mg/day: after 3 months of treatment, no effect on sperm motility was detected.
Precautionary measures
Use for impaired liver function There is no need for dose adjustment for patients with impaired liver function. Use for impaired renal function In patients with impaired renal function, a dose reduction is recommended in accordance with the QC. Use in Elderly Patients Elderly patients (over 65 years of age) may require a reduction in the dose of pregabalin due to deterioration of renal function. Use in children The safety and effectiveness of pregabalin in children and adolescents under 18 years of age have not been established. Patients with Diabetes Mellitus According to current clinical practice, some patients with diabetes mellitus whose body weight increases while using pregabalin may require dosage adjustment of hypoglycemic drugs. Hypersensitivity reactions Hypersensitivity reactions, including cases of angioedema, have been reported. Pregabalin should be discontinued immediately if symptoms of angioedema such as swelling of the face, perioral area, or upper respiratory tract occur. Dizziness, drowsiness, loss of consciousness, confusion and mental disturbances Pregabalin use has been associated with cases of dizziness and drowsiness, which may increase the risk of accidental injury (falls) in elderly patients. The development of such adverse reactions as loss of consciousness, confusion, and mental disturbances has also been reported. Therefore, patients should be advised to exercise caution until they are aware of the possible effects of the drug. Visual disturbances: Temporary blurred vision and other vision changes have been reported in patients treated with pregabalin. In most cases, this phenomenon disappeared with continuous use of pregabalin. It is known that in studies in which ophthalmological examination was performed, the incidence of deterioration in visual acuity and changes in visual fields was higher in patients treated with pregabalin than in patients in the placebo group. Eye side effects have also been reported, including loss of vision, blurred vision, or other changes in visual acuity, most of which were temporary. Discontinuation of pregabalin may result in resolution or improvement of these visual symptoms. Discontinuation of concomitant antiepileptic drugs There is insufficient data regarding the discontinuation of concomitant antiepileptic drugs after seizure control is achieved when pregabalin is added to existing treatment in order to switch to pregabalin monotherapy. Withdrawal symptoms After stopping short- and long-term use of pregabalin, some patients experienced withdrawal symptoms (see section "Side effects"). Seizures, particularly status epilepticus and grand mal seizures, may occur during treatment with pregabalin or shortly after discontinuation of pregabalin use. Renal failure Cases of renal failure have been reported. Although the effect of drug discontinuation on the reversibility of renal failure has not been studied systemically, improvements in renal function have been reported following drug discontinuation or pregabalin dose reduction. Congestive Heart Failure Cases of congestive heart failure have been reported in patients using pregabalin. This reaction has mostly been observed during pregabalin treatment of neuropathic pain in elderly patients with cardiovascular disorders. Pregabalin should be used with caution in such patients. This phenomenon may disappear when pregabalin is discontinued. Treatment of central neuropathic pain due to spinal cord injury It is known that during the treatment of central neuropathic pain due to spinal cord injury, the incidence of adverse reactions in general, adverse reactions from the central nervous system, especially drowsiness, was increased. This may be explained by the additive effect of concomitant medications (eg, antispastic agents) that are necessary to treat this condition. This circumstance must be taken into account when pregabalin is prescribed to such patients. Suicidal ideation and behavior Cases of suicidal ideation and behavior have been observed in patients treated with antiepileptic drugs for certain indications. Existing data from a meta-analysis of randomized placebo-controlled trials of antiepileptic drugs also showed a nonsignificant increase in the risk of suicidal ideation and behavior. The mechanism by which this risk occurs is unknown, and available data do not exclude the possibility of its existence for pregabalin. Therefore, it is necessary to closely monitor the patient for signs of suicidal ideation and behavior and prescribe appropriate treatment if it occurs. Patients (and their caregivers) should be aware of the need to seek medical attention if signs of suicidal ideation or behavior occur. Lower gastrointestinal deterioration: Lower gastrointestinal deterioration (eg, ileus, paralytic ileus, constipation) has been reported due to the use of pregabalin with drugs that may cause constipation, such as opioid analgesics. When using pregabalin and opioids in combination, measures should be taken to prevent constipation (especially in women and elderly patients). Additive Potential Cases of drug misuse, abuse, and dependence have been reported. The drug should be prescribed with caution to patients with a history of substance abuse; It is necessary to monitor the patient for symptoms of misuse, abuse or dependence on pregabalin (cases of addiction, exceeding the prescribed dose, drug-seeking behavior have been reported). Encephalopathy Cases of encephalopathy have occurred predominantly in patients with concomitant diseases that can cause encephalopathy. Use in Pediatrics The safety and effectiveness of pregabalin in children under 18 years of age have not been established. Based on existing data (see section “Pharmacological action”) it is impossible to provide any recommendations regarding the use of the drug in this category of patients. Effects on the ability to drive vehicles and use machines Pregabalin may cause dizziness and drowsiness and may affect the ability to drive a vehicle or use machines. Therefore, patients should be advised to refrain from driving or operating complex machinery until it is known exactly how Neogabine affects the ability to perform such activities.
Interaction with other drugs
Because pregabalin is primarily excreted unchanged in the urine, undergoes little metabolism in humans (less than 2% of the dose is excreted in the urine as metabolites), does not inhibit the in vitro metabolism of other drugs, and is not bound to plasma proteins, it is unlikely that pregabalin would in pharmacokinetic drug interactions. In vivo study and population pharmacokinetic analysis In in vivo studies, no clinically significant pharmacokinetic interactions were observed between pregabalin and phenytoin, carbamazepine, valproic acid, lamotrigine, gabapentin, lorazepam, oxycodone, or ethanol. A population pharmacokinetic analysis showed that oral antidiabetic drugs, diuretics, insulin, phenobarbital, tiagabine and topiramate do not have a clinically significant effect on the clearance of pregabalin. Oral contraceptives, norethisterone and/or ethinyl estradiol Concomitant use of pregabalin and oral contraceptives (norethisterone and/or ethinyl estradiol) does not affect the steady-state pharmacokinetics of either drug. Medicines affecting the central nervous system Pregabalin may potentiate the effect of ethanol and lorazepam. In controlled clinical studies, coadministration of multiple oral doses of pregabalin and oxycodone, lorazepam, or ethanol did not have a clinically significant effect on respiratory function. In clinical practice, respiratory failure and coma have been reported in patients taking pregabalin and CNS depressants concomitantly. Pregabalin appears to potentiate oxycodone-induced cognitive and gross motor impairment. Interaction in Elderly Patients Specific pharmacodynamic interaction studies have not been conducted in elderly patients.
Contraindications
hypersensitivity to the active substance or any of the excipients.
Compound
1 caps. pregabalin 75 mg Excipients: microcrystalline cellulose, croscarmellose sodium, magnesium stearate, talc. Composition of hard gelatin capsule: gelatin, titanium dioxide (E171).
Overdose
Symptoms: The most common adverse reactions reported in cases of pregabalin overdose were drowsiness, confusion, agitation and restlessness. Cases of coma have been reported occasionally. Treatment: should include general supportive measures and, if necessary, hemodialysis.
Side effect
The most common manifestations of adverse reactions were dizziness and drowsiness. It is known that adverse reactions were usually mild or moderate. Adverse reactions reported with the use of pregabalin are listed below according to the classification of organs and systems indicating their frequency: very often (≥1/10), often (≥1/100,
Storage conditions
The drug should be stored in its original packaging to protect it from light and moisture, out of the reach of children at a temperature not exceeding 25°C. Shelf life of the drug Shelf life – 2 years. Do not use after the expiration date stated on the package.
Buy Neogabine caps. 75 mg per bl. in pack No. 10x3 in the pharmacy
Price for Neogabine caps. 75 mg per bl. in pack №10x3
Instructions for use for Neogabin caps. 75 mg per bl. in pack №10x3
Interaction
Since the drug is predominantly excreted unchanged in the urine and is only slightly metabolized in humans (<2% of the administered dose is excreted in the urine as metabolites), does not inhibit the in vitro metabolism of other drugs and does not bind to blood proteins, it is unlikely that pregabalin may enter into pharmacokinetic interactions with other drugs or be subject to such interactions.
Accordingly, no significant clinical pharmacokinetic interactions were observed between pregabalin and phenytoin, carbamazepine, valproic acid, lamotrigine, gabapentin, lorazepam, oxycodone, or ethanol in in vivo studies. In addition, a population pharmacokinetic analysis showed that oral antidiabetic drugs, diuretics, insulin, phenobarbital, tiagabine and topiramate did not have a clinically significant effect on the clearance of pregabalin.
The simultaneous use of pregabalin and oral contraceptives - norethisterone and/or ethinyl estradiol - does not affect the steady-state pharmacokinetics of either drug.
Pregabalin may potentiate the effect of ethanol and lorazepam. In controlled clinical studies, multiple oral doses of pregabalin and oxycodone, lorazepam, or ethanol did not have a clinically significant effect on respiratory function. During post-marketing surveillance, respiratory failure and coma have been reported in patients taking pregabalin and other CNS depressants concomitantly. Pregabalin increased the impairment of mnestic and basic motor functions caused by oxycodone. There have been post-marketing reports of events associated with decreased lower gastrointestinal function (eg, ileus, paralytic ileus, constipation) when pregabalin is coadministered with drugs that may cause constipation, such as opioid pain medications.
No specific studies of pharmacodynamic interactions have been conducted in elderly volunteers.
Note!
The description of the drug Neogabine on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use. Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug).
Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.