1.General information
The term “acute abdomen” appeared in Russian medicine and became commonly used by the mid-twentieth century, after the publication in 1940 of a translation of a monograph by French surgeon Henri Mondor on emergency gastroenterological diagnostics.
Below we use another figurative expression from A. Mondor’s book: “abdominal catastrophe.”
We are talking about a life-threatening condition in which the prognosis is directly dependent on how quickly emergency medical care is called and provided. Statistical and analytical studies have repeatedly confirmed that the mortality associated with the condition of an acute abdomen increases several times, even if the delay for one reason or another is about a day.
It must be recognized that in big cities the situation in this regard is still much better than in the periphery.
A must read! Help with treatment and hospitalization!
Prevention of acute abdomen
There is no specific prevention of acute abdomen!
- Dynamic observation by a family doctor and treatment of chronic diseases of the gastrointestinal tract, cardiovascular system, lungs, liver, kidneys, and genitourinary system.
- Timely referral of the patient to a surgeon if symptoms of an acute abdomen occur.
- Qualified differential diagnosis in the surgical department.
- Adequate choice of treatment tactics (operative or conservative management of the patient).
- The use of antibacterial drugs and other medications to prevent postoperative complications.
2. Reasons
Acute abdomen as a special pathological status can develop as a result of gastroenterological diseases, their progression and exacerbation, or for reasons not directly related to gastrointestinal diseases.
Thus, the gastroenterological diseases that most often cause the development of acute abdomen include:
- perforated ulcer of the stomach and duodenum;
- purulent acute appendicitis;
- phlegmonous cholecystitis with perforation of the walls of the gallbladder;
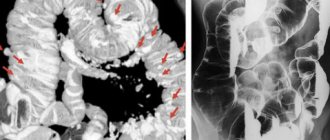
- intestinal obstruction;
- acute pancreatitis;
- strangulated hernia,
as well as acute diffuse peritonitis that developed as a result of the listed or other factors.
Quite often, the cause of an abdominal catastrophe is severe gynecological diseases and complications, primarily ectopic pregnancy and polycystic ovary syndrome with ruptured cysts or torsion of their legs, as well as mechanical ruptures of the spleen, intestines, and bladder due to blunt or penetrating abdominal trauma.
In some cases, the condition of an acute abdomen develops following thrombosis or rupture of an aneurysm (with massive internal bleeding in the abdominal cavity) in the mesenteric blood vessels or the abdominal aorta.
Visit our Gastroenterology page
Emergency conditions in gynecology
“Acute abdomen” in gynecology is a syndrome that develops as a result of acute pathology in the abdominal cavity and is manifested by sudden pain in any part of the abdomen, peritoneal symptoms and pronounced changes in the patient’s condition.
Acute pain in the lower abdomen in women with severe peritoneal symptoms is possible:
- with intra-abdominal bleeding (ectopic pregnancy, ovarian apoplexy);
- torsion of the legs of an ovarian cyst (cystoma);
- perforation of purulent formations of the appendages;
- pelvioperitonitis.
Risk factors for developing ectopic pregnancy:
- previous history of salpingoophoritis, endomyometritis, abortion;
- violation of hormonal function of the ovaries;
- genital infantilism;
- endometriosis;
- previous operations on the internal genital organs;
- increased trophoblast activity.
In an ectopic pregnancy, the fertilized egg implants and develops outside the uterine cavity. Pregnancy can develop or be disrupted (by the type of tubal abortion or by the type of fallopian tube rupture).
During a tubal abortion, the fertilized egg, not having the appropriate conditions for development, peels off from the walls of the fallopian tube and is expelled into the abdominal cavity. Due to the rhythmic contraction of the fallopian tube, blood enters the abdominal cavity periodically.
When the fallopian tube ruptures (with a delay of menstruation by an average of 3–4 weeks) as a result of a violation of an ectopic pregnancy, the villi of the fertilized egg completely destroy the thin wall of the fallopian tube and blood from the damaged vessels pours into the abdominal cavity.
Ovarian apoplexy (ovarian rupture, ovarian infarction, ovarian hematoma) is an acute violation of the integrity of the ovary with hemorrhage into its stroma and subsequent bleeding into the abdominal cavity. Ovarian apoplexy occurs more often in women of reproductive age, but also occurs in adolescents, more often occurring during the period of ovulation and in the stage of vascularization and flowering of the corpus luteum.
Ovarian rupture occurs due to:
- congestive hyperemia;
- varicose or sclerotic vessels;
- sclerotic changes in the stroma;
- dysfunctions of the autonomic and endocrine systems.
A hematoma forms, which causes sharp pain due to an increase in intraovarian pressure, followed by rupture of the ovarian tissue.
Torsion of the pedicle of an ovarian cyst (cystoma) is a complication of an ovarian cyst or cystoma. The onset of the disease is often associated with the following factors:
- sudden change in body position;
- increased intra-abdominal pressure as a result of strong straining, prolonged coughing, heavy physical work;
- impaired blood supply to the cyst.
When the cyst pedicle is torsed, the following is observed:
- disturbance of blood supply;
- swelling of the cyst;
- hemorrhage and necrosis of the parenchyma.
With partial (gradual) torsion:
- the leg changes its position by 90–180°;
- arterial blood flow is maintained;
- venous outflow is difficult due to vascular compression;
- Venous congestion and swelling of the cyst wall occur.
In case of complete (sudden) torsion:
- the leg changes its position by 360°;
- arterial blood flow stops;
- necrobiotic processes occur in the ovarian cyst;
- peritoneal symptoms appear;
- When the cyst becomes infected, peritonitis begins.
Provoking factors for the development of purulent formations of the appendages are:
- microbial invasion;
- weakening or changing the barrier properties of the uterus and genital tract:
– physiological (menstruation, childbirth);– iatrogenic (abortion, intrauterine contraceptives, operations, hysteroscopy, in vitro fertilization).
The routes of infection of the appendages can be intracanalicular, ascending, hematogenous, lymphogenous.
The following ectopic pregnancies are distinguished: tubal, ovarian, cervical, in the rudimentary horn, abdominal.
Fallopian tube rupture occurs suddenly and causes:
- bleeding, usually massive (intra-abdominal);
- pain in the lower abdomen, radiating to the rectum;
- dizziness;
- weakness;
- pale skin;
- fainting state.
With continued bleeding, hemorrhagic shock and posthemorrhagic anemia begin. The severity of hemodynamic disorders is directly dependent on the deficit in circulating blood volume.
Ovarian apoplexy is accompanied by: intra-abdominal bleeding (anemic form of apoplexy); pain syndrome (pain form).
The disease begins acutely, with sudden pain in the lower abdomen, mainly on the affected side.
Torsion of the pedicle of an ovarian cyst (cystoma) causes:
- pain in the lower abdomen from the side of the mass - gradually increasing or acute;
- nausea, vomiting, flatulence;
- intestinal paresis;
- tension of the anterior abdominal wall;
- symptoms of peritoneal irritation.
The clinical picture of inflammatory diseases of the female genital organs, in particular the uterine appendages, is often blurred and asymptomatic. Pyosalpinx, piovar, tubo-ovarian abscess cause:
- constant pain in the lower abdomen, mainly due to inflammation;
- chills, high fever;
- weakness;
- tachycardia;
- nausea, stool retention, gas;
- purulent discharge from the genital tract.
The pain radiates to the lower extremities and lumbar region. The abdomen is soft and may be moderately swollen.
With perforation of purulent formations, mild symptoms of peritonitis appear already in the first hours, which overlap with the clinical picture of a severe inflammatory process and include:
- pain is intense, sometimes aching, of unclear localization;
- chills, fever, tachycardia;
- painful urination;
- loose stools;
- bloating;
- local symptoms of peritoneal irritation.
Possible complications include intra-abdominal bleeding and pelvioperitonitis or peritonitis.
Diagnostics
Symptoms of ectopic pregnancy:
- amenorrhea 4–8 weeks, probable signs of pregnancy;
- positive immunological reactions to pregnancy;
- the size of the uterus is less than the expected pregnancy;
- spotting bloody discharge from the genital tract;
- unilateral cramping or constant pain;
- pain when the cervix is displaced;
- unilateral adnextumor;
- general disorders (deterioration of general condition, nausea, diarrhea, flatulence).
When the fallopian tube ruptures, the abdomen participates in the act of breathing to a limited extent, is painful on palpation and percussion, symptoms of peritoneal irritation are positive, and upon percussion there is dullness in the sloping areas of the abdomen.
In case of ovarian apoplexy, during examination the following is determined:
- in the painful form - pain in the lower abdomen, symptoms of peritoneal irritation are mild;
- in the anemic form - signs of intra-abdominal bleeding.
During an objective examination, general signs include behavior, gait, position in the gynecological chair and reaction to pain with facial expressions; color of skin and mucous membranes.
The respiratory rate can be more than 20 beats/min - with peritonitis, acute blood loss.
Tachycardia is always present in “acute abdomen” of any origin, as it is characteristic of fever, hypovolemia, and acute blood loss.
“Acute abdomen” is not accompanied by hypertension. Hypotension is caused either by a septic condition or by hypovolemia due to acute blood loss (tubal rupture, cyst rupture, ovarian apoplexy).
A general objective examination reveals signs of pregnancy: enlargement (engorgement) of the mammary glands, pigmentation of the nipples, and the release of colostrum.
A coated, dry tongue indicates inflammatory processes in the genitals, appendicitis, intestinal obstruction, and peritonitis.
An increase in abdominal volume is observed with large tumors, ascites, intestinal obstruction, peritonitis, intra-abdominal bleeding; lag of the abdominal wall from respiratory excursions - for all causes of “acute abdomen”.
Palpation of the abdomen during peritonitis reveals tension and pain in the abdominal wall, Shchetkin-Blumberg symptom; with bleeding into the abdominal cavity (ovarian apoplexy, rupture of the fallopian tube, rupture of the spleen) - Kulenkampff's symptom, pain and symptoms of irritation of the peritoneum without tension in the abdominal wall.
With intra-abdominal bleeding, inflammatory effusion, ascites, percussion of the abdomen shows dullness in sloping areas (iliac regions), which moves when the body changes to one side.
In a general blood test, leukocytosis, a shift in the leukocyte formula to the left, and an accelerated ESR indicate inflammatory diseases of the genitals; a decrease in hemoglobin level indicates intra-abdominal bleeding.
Puncture of the abdominal cavity through the posterior vaginal fornix reveals the nature of the liquid contents in the abdominal cavity (pus, serous effusion, blood).
An ultrasound is performed to clarify the size of the uterus, identify pathological formations in the uterus and appendages, and the presence of effusion.
Differential diagnosis of fallopian tube rupture is carried out with the following conditions:
- ectopic pregnancy (delayed menstruation, subjective signs of pregnancy, bleeding from the genital tract);
- acute pancreatitis (girdle pain, intense, poor diet, chronic diseases of the digestive system);
- perforated ulcer of the stomach and duodenum;
- acute appendicitis;
- torsion of the pedicle of an ovarian cyst, etc.
Torsion of the pedicle of the cyst (cystoma) and ovarian apoplexy are differentiated from acute appendicitis and impaired ectopic pregnancy.
Main directions of therapy
- In case of intra-abdominal bleeding - administration of blood-substituting solutions (dextrans, starch preparations) until hospitalization.
- Broad-spectrum and long-acting antibiotics (ceftriaxone 1–2 g intravenously or intramuscularly in combination with metronidazole 100 ml intravenously and amoxicillin 2–4 g intravenously in combination with metronidazole 100 ml intravenously).
In case of torsion of the pedicle of the cyst (cystoma) of the ovary, treatment is not carried out at the prehospital stage.
The algorithm for dealing with bleeding in the event of an ectopic pregnancy is presented in the figure.
Clinical pharmacology of individual drugs
Reopolyglucin is a 10% solution of low molecular weight dextran dissolved in an isotonic sodium chloride solution. It has a detoxifying effect, prevents and eliminates the aggregation of blood cells and reduces its viscosity, helps restore blood flow in small vessels. Available in bottles of 200 and 400 ml. Administer intravenously in streams and drips of 400–1000 ml (up to 1500 ml).
Polyglucin (dextran) is a synthetic colloidal plasma substitute that has a colloid-osmotic and hemodynamic effect. Produced in bottles of 200 and 400 ml of 6% solution. Administer intravenously in streams and drips of 400–1200 ml (up to 2000 ml).
Common errors in therapy are: administration of analgesics and delay in hospitalization.
Analysis of clinical cases. The ambulance team was called to the home of a 24-year-old patient who complained of weakness, dizziness, dry mouth, and pain in the lower abdomen radiating to the rectum. The patient became acutely ill 2 hours ago, when the above complaints suddenly arose after coitus.
From the anamnesis, it was possible to find out that the patient’s menstruation began at the age of 12, 6–7 days after 30 days, moderate, painless. The last menstruation began 14 days ago, came on time, and went as usual. Contraception was carried out with the combined oral contraceptive Logest for 4 months.
On examination: the patient's condition is moderate. The skin is pale. The tongue is dry, covered with a white coating. Blood pressure - 90/60 mm Hg. Art., pulse - 92 beats/min, rhythmic. Heart sounds are clear and rhythmic. The abdomen evenly participates in the act of breathing, is somewhat swollen, sharply painful on palpation in the lower parts. The Shchetkin–Blumberg sign is positive in the lower sections.
Probable diagnosis: ovarian apoplexy, intra-abdominal bleeding.
Emergency hospitalization to a gynecological hospital is indicated and, taking into account the presence of intra-abdominal bleeding, the administration of blood replacement solutions (dextrans, starch preparations) is indicated at the pre-hospital stage.
The ambulance team was called to the home of a 20-year-old patient who complained of pain in the left lower abdomen, nausea, vomiting, flatulence, gradually increasing or acute; I fell ill 3 days ago, when, after physical activity, pain first appeared in the lower abdomen, more on the left, which gradually intensified.
From the anamnesis: the patient’s menstruation from 15 years of age was 4–5 days every 30 days, moderate, painless. The last menstruation began 10 days ago, came on time, and went as usual. Sexual life from the age of 17, without contraception. The only pregnancy ended in an induced abortion at 5 weeks, without complications. 2 months ago, during a routine examination, a gynecologist discovered a cyst on the right ovary. No treatment was given.
Objectively: the patient’s condition is of moderate severity. The skin is pale. The tongue is clean and moist. Blood pressure - 110/75 mm Hg. Art., pulse - 78 beats/min, rhythmic. Heart sounds are clear and rhythmic.
The abdomen evenly participates in the act of breathing, is not distended, there is pronounced tension in the muscles of the anterior abdominal wall, the symptoms of peritoneal irritation are positive.
Presumable diagnosis: torsion of the pedicle of the right ovarian cyst. The patient is indicated for urgent hospitalization in a hospital. If the pedicle of an ovarian cyst is torsed, no treatment is carried out at the prehospital stage.
Let's give other examples.
The ambulance station received a call from patient E., 34 years old, who 5 hours ago developed intense aching pain of unclear localization, chills, fever, painful urination, loose stools, and bloating. 10 days ago, the patient underwent an ultrasound-guided medical abortion at 8 weeks of pregnancy and removal of an intrauterine contraceptive inserted 7 years ago. After 7 days, cloudy, purulent discharge from the genital tract with an unpleasant odor appeared.
Probable diagnosis: acute bilateral salpingoophoritis, endomyometritis; pelvioperitonitis.
The patient requires emergency hospitalization in a gynecological hospital. At the prehospital stage, infusion, antibacterial, and anti-inflammatory therapy is indicated.
The ambulance station received a call from patient D., 28 years old, who, 3 hours ago after lifting weights, developed pain in the lower abdomen, which gradually intensified, as well as nausea, vomiting, and dry mouth. From the medical history, it was possible to find out that the patient’s last normal menstruation was 3 weeks ago, came on time, and was more scanty. It is necessary to make a differential diagnosis between acute appendicitis, torsion of the pedicle of an ovarian cyst, and impaired tubal pregnancy.
The patient is indicated for urgent hospitalization in a gynecological hospital.
Taking into account the possibility that the patient had a torsion of the pedicle of the ovarian cyst, no treatment was carried out at the prehospital stage.
A. Z. Khashukoeva , Doctor of Medical Sciences, Professor Z. Z. Khashukoeva Russian State Medical University, Moscow
3. Symptoms and diagnosis
There are clear criteria and diagnostically significant signs of acute abdomen. In particular, obligate symptoms include uncontrollable spastic muscle tension of the anterior abdominal wall, especially pronounced in the “catastrophe” area, and hypersensitivity of the abdominal skin.
Another mandatory sign is intense pain, which, however, does not always reach extreme severity. Depending on the etiology, the pain may not be dagger-like, but quite tolerable, dull, wave-like - which in such cases often leads to fatal waiting instead of immediately seeking help.
The patient himself, as well as those providing first aid, should interpret bloating, lack of peristalsis and the urge to release gases from the intestines as a very alarming sign.
It is also necessary to pay attention to the general condition of the patient (usually it progressively worsens), dry mouth, accelerated pulse, painful inhalation and exhalation, which forces the patient to breathe frequently and shallowly. The so-called acute abdomen is very characteristic. the mask of Hippocrates - a sallow, pale, haggard face with sharpened features and a frozen expression of suffering.
Arriving health workers apply standard diagnostic protocols and criteria for differential diagnosis: the suspected acute abdomen may not be confirmed, since many diseases and conditions imitate typical symptoms to one degree or another. In particular, it is necessary to exclude lower lobe pleurisy or pneumonia, myocardial infarction and other factors of acute heart failure, renal colic, etc. A prompt and, if possible, detailed history taking should also exclude fractures of the pelvis, ribs, and spine. An external examination, palpation and auscultation are performed, and it is very important to first reassure the patient and, among other things, warm your hands before palpation (if assistance is provided in the cold season) in order to maximally objectify the clinical picture and prevent involuntary aggravation (exaggeration of symptoms). In general, a lot depends on the qualifications, experience, tactile sensitivity and skills of the doctor. When diagnosing a suspected acute abdomen in young children or people with abnormal body weight, a digital examination through the vagina or anus (if the patient is male) is indicated - careful palpation with this access is often the most informative diagnostic technique and brings decisive arguments.
It should be noted that the widespread opinion about the inadmissibility of pre-medical use of analgesics in such a situation (so as not to “blur” the symptoms) is exaggerated and unsubstantiated: the analysis of the clinical picture is always complex, including not only subjective pain sensations.
All necessary, in this particular case, additional diagnostic methods, laboratory and instrumental, are carried out urgently immediately after hospitalization - if there is time for this, taking into account the patient’s condition.
About our clinic Chistye Prudy metro station Medintercom page!
Epidemiology of acute abdomen
Without a doubt, acute abdomen is one of the top five among all diseases in terms of incidence, along with acute coronary syndrome (myocardial infarction, unstable angina), acute cerebrovascular accident (ischemic and hemorrhagic strokes), acute trauma (road accidents, domestic trauma, burns and etc.), various infectious diseases.
In surgical practice, the acute abdomen comes first, as it includes a fairly large group of nosological units. Since statistics are kept for individual diseases, it is difficult to give an exact figure for the pathological incidence of the population with “acute abdomen”.
4.Treatment
Almost all cases of acute abdomen create absolute indications for emergency surgery. Currently, the standard of care, based on extensive statistical material, requires making and implementing a decision within a time period not exceeding six hours from the moment of the onset of diagnostically significant symptoms.
Therefore, it is worth recalling once again that in any situation and in any area, with any refusals and any dissimulation (deliberate concealment of sensations) on the part of the patient - who, before the onset of symptoms characteristic of an acute abdomen, could be as strong and healthy as he likes - as well as with any doubts among relatives, the time factor is critical, and the faster help is provided, the higher the chances of avoiding death. The question should be posed precisely in this formulation.
Forecast
The prognosis of acute abdomen syndrome is ambiguous. The outcome of the pathology is influenced by the following factors: the direct cause of the syndrome, the patient’s age, concomitant diseases, and the timeliness of the operation. Long-term purulent inflammation of the peritoneum, necrotic damage to the intestinal wall, and mesenteric thrombosis worsen the prognosis of the syndrome, especially in weakened individuals, the elderly and children. Early diagnosis and proper therapy reduce the mortality rate.