Ehlers-Danlos syndrome (according to some sources, Ehlers-Danlos syndrome, EDS) is a rare hereditary collagen pathology that affects the skin, musculoskeletal system and other organs. Other names for the syndrome are “skin hyperelasticity”, cutis hyperelastica, Rusakov desmogenesis imperfecta and Chernogubov-Ehlers-Danlos syndrome. People with this syndrome could be seen in the circus in the past because of their ability to surprise ordinary people with their appearance and movements. Some famous people also suffered from this disease - for example, virtuoso violinist Niccolo Paganini.
History of the discovery of the syndrome
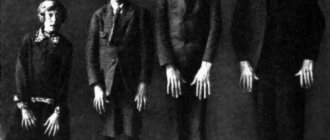
People with this disease were described by Hippocrates in 400 BC. e. in the essay “Airs, Waters and Places” (De aere, aquis, locis). He observed nomads and Scythians with weak joints and multiple scars around them. Hippocrates believed that the scars were traces of cauterization, with the help of which they tried to reduce joint hypermobility. Much later, in 1657, the Dutch surgeon J. Van Meekeren (1611–1666) described a small Spaniard with very elastic skin. A boy named George Albs could stretch the skin of his chin to his chest, and the skin of his knees to the middle of his shins, but this only affected the right half of his body. World-famous violinist and composer Niccolo Paganini (1782–1840) had hypermobile joints, a thin physique, and a deformed chest—all symptoms characteristic of a carrier of Ehlers-Danlos syndrome. At the end of the 19th century, some patients with EDS performed as people with unusual abilities in traveling shows, such as the “elastic lady” described by American doctors George M. Gould and Walter L. Pyle. For a long time, the diversity of clinical manifestations of the syndrome did not allow a detailed description of all forms of the disease.
Diagnostics
Diagnosing this disease is a very difficult matter and requires knowledge and skills in the field of genetics and more. The main sign indicating the presence of the disease is stretching of the skin 2 cm from the body. In a healthy person, such a tension is simply impossible to perform. A number of special methods are used to help determine whether the disease belongs to a certain type. After they are completed, a special course of therapy will be prescribed, aimed at improving health and avoiding progression of the disease and death. The main attention is paid to the following indicators:
- hyperelasticity of the skin, in a tense and normal state;
- joint hypermobility is assessed using a special Brighton scale;
- condition of blood vessels, presence of bruises and cyanosis;
- fragility of the skin and the presence of wounds;
- painful sensations.
The main diagnosis is made based on the following measures:
- collecting information about the patient;
- examination of the musculoskeletal system, joints and skin, measurement of folds on it;
- a biopsy is performed to analyze a piece of skin to establish an accurate diagnosis and exclude dermatosparaxis and arthrochalasia;
- molecular genetic examinations are carried out.
In addition to the main methods, the following are also used:
- ultrasound examination of internal organs to identify possible pathological changes caused by Ehlers syndrome;
- examination by an ophthalmologist using biomicroscopy and computed tomography;
- electrocardiogram;
- Tilt test.
After all the studies have been carried out and their results have been fully collected, a diagnosis is made and a course of treatment begins.
Classification and name
The first detailed description of EDS was presented by the Russian doctor at the Myasnitskaya Hospital in Moscow, Andrei Chernogubov, at the Moscow Venereological and Dermatological Society in 1892. He described two patients with increased mobility of large joints. One of them was a 17-year-old boy with epilepsy who had fragile and hyperelastic skin that was unable to hold sutures.
Later, in 1901, Danish dermatologist Edvard Lauritz Ehlers published a description of a patient with weak joints and hyperelastic skin, with a predisposition to bruising. He demonstrated it at the Danish Dermatological Society in 1899. Seven years later, French physician Henri-Alexandre Danlos examined a patient with vascular skin lesions on the elbows and knees. Afterwards, separate descriptions of this syndrome appeared in both the USA and England, and by 1966 the total number of reports had increased to 300. In 1936, the English dermatologist Frederick Parkes Weber combined all cases with hyperelasticity and fragility of the skin, as well as hypermobility joints. He called the new disease “Ehlers-Danlos syndrome.”
In 1972, the first molecular defect in collagen was discovered in EDS. In 1986, at the International Congress on Hereditary Connective Tissue Diseases in Berlin, 9 types of Ehlers-Danlos syndrome were identified, but in 1997, in Villefranche-sur-Mer (France), experts developed and adopted a more precise classification. It already had 6 types of EDMS:
- classical;
- hypermobile;
- vascular;
- kyphoscoliotic;
- achondroplasyplastic;
- dermatosparaxis.
Causes
This pathology is considered a genetic disease. From medical research it is known that not only the skin consists of connective tissue, but all organs are surrounded by it. Therefore, this disease very often has a systemic nature and affects:
- skin covering;
- joints and ligaments;
- internal organs;
- various systems.
For this reason, in addition to geneticists, the disease is of great interest to people from other scientific fields, such as:
- traumatology;
- orthopedics;
- ophthalmology;
- cardiology;
- dentistry and others.
The disease occurs due to mutations of certain genes. Gene mutations lead to a deficiency of hydroxylysine, which is an important and very necessary component of collagen. As a result of this phenomenon, the biosynthesis of collagen fibers is disrupted and collagen instability begins to occur. Consequently, various kinds of changes begin in the connective tissue. The most basic and pronounced is hyperelasticity. This disease in severe form is extremely rare, often it is a moderate form of the severity of the disease.
Diagnosis criteria
This classification not only systematizes the forms of the syndrome, but also identifies major and minor criteria for diagnosing Ehlers-Danlos syndrome, which is why it is often called the Villefranche diagnostic criteria.
Major diagnostic criteria:
- Thin translucent skin with a visible venous pattern.
- Predisposition to vascular, intestinal and uterine ruptures or weakness of these structures.
- Easy bruising and bleeding.
- Characteristic facial features: wide-set eyes, depressed middle part and epicanthus fold at the inner corner of the eye, covering the lacrimal tubercle
Some minor diagnostic criteria:
- Premature aging of the limbs (acrogeria - atrophy of the skin of the hands and feet).
- Hypermobility of small joints (interphalangeal and metacarpophalangeal joints of the hand).
- Rupture of tendons and muscles.
- Clubfoot.
- Pneumothorax/pneumothorax.
- Retraction (sagging) of the gums, their underdevelopment.
- Complicated family history, sudden death of close relatives.
Two or more major criteria allow one to suspect EDS; laboratory confirmation is required for clarification. If only small criteria exist, then this is not an EDS - there must be at least one large criterion.
Hypermobile EDMS
It is inherited in an autosomal dominant manner and is associated with the type 3 collagen gene COL3A1. Occurs in one person per 10,000–15,000 population. The dominant symptom is increased mobility of large and small joints, accompanied by pain. Dislocations and subluxations can occur spontaneously or due to minor injuries. Symptoms occur regardless of age, but in children with Ehlers-Danlos syndrome it is more difficult to diagnose due to the physiological weakness of the ligamentous apparatus of the joints. Patients with this type of EDS are also characterized by early development of osteoporosis (almost immediately after 30 years). This type of EDS is also characterized by functional disorders of the large intestine, hypermobility of the esophagus, gastroesophageal reflux and gastritis.
Vascular EDS
Develops with an autosomal dominant defect in the COL3A1 gene, which is involved in the synthesis of type III collagen. It is less common than the previous two types - one in 250,000 people. This type is characterized by a high risk of profuse bleeding from internal organs and ruptures of blood vessels. A patient with the vascular type of EDS has thin skin with vessels visible through it. It is precisely because of problems with blood vessels that such patients rarely live past 50 years. The appearance of a patient with the vascular type of EDS can be very characteristic - the face looks emaciated with prominent cheekbones and sunken cheeks, the nose and lips are thin. At the same time, there is no pronounced hyperelasticity of the skin.
The remaining types are much less common than the previous three - there are about 100 cases worldwide. The achondroplasisplastic type of EDS develops due to a defect in type 1 collagen. About 30 cases have been reported. Already at birth, children with Ehlers-Danlos syndrome are diagnosed with hip dislocation; patients suffer from early arthritis, frequent bruising of the skin and its increased elasticity, as well as atrophic scars. Dermatosparaxis - only 10 cases of EDS of this type have been registered in the world. Patients have extremely fragile skin with a soft, loose texture that is prone to bruising easily. Very early on, patients begin to experience chronic debilitating pain in the joints and muscles. Hyperelasticity of the skin manifests itself to varying degrees, but there is no atrophy of scars.
Prognosis for patients
There is no increased risk of early mortality, however, due to joint instability, chronic and acute pain, and symptoms outside the musculoskeletal system, the patient's quality of life is seriously impaired.
As mentioned above, there is no special treatment. It is necessary to undergo individualized auxiliary and symptomatic treatment methods, including physical therapy, rehabilitation, analgesics and appropriate therapy for extra-articular symptoms. Surgical measures should be considered judiciously.
Treatment and prognosis
Patients with EDS are observed throughout their lives by various specialists - therapists, geneticists, orthopedists, physiotherapists, exercise therapy specialists, neurologists, cardiologists, etc., depending on the clinical symptoms. There is no specific treatment. Early diagnosis of Ehlers-Danlos syndrome in children allows one to make a prognosis, select the necessary lifestyle for the patient and reduce the number of complications associated with the underlying disease. Most people with this diagnosis can live relatively normal and long lives. The main condition is to reduce injuries while maintaining sufficient physical activity for the development of the muscular frame. In addition, regular preventive examinations and treatment by a dentist and ophthalmologist are necessary.
Sources
- Federal clinical guidelines for the diagnosis and treatment of Ehlers-Danlos syndrome. Rumyantsev A. G., Maschan A. A., Zhukovskaya E. V. - 2021
- Ehlers-Danlos syndrome—a historical review Liakat A. Parapia and Carolyn Jackson Department of Haematology, Bradford Teaching Hospitals NHS Foundation Trust, and University of Bradford, Bradford, UK.
- Vascular type of Ehlers-Danlos syndrome. M. V. Gubanova, L. A. Dobrynina, L. A. Kalashnikov. — Volume 10. — No. 4–2016. Annals of Neurology.
- Ehlers-Danlos syndrome in a 6-year-old child. E. F. Argunova, O. N. Ivanova, E. E. Gurinova, S. N. Alekseeva. Pacific Medical Journal. - 2014. - No. 2.
Prevention
In order to prevent complications and due to the increased risk of injury, patients should avoid contact sports, as well as those that involve a high load on the joints (running, football, etc.), exercises with weights and stretching. In addition, they should be guided by the choice of a profession that does not involve constant stress on the spine and legs, as well as physical activity.
To protect and stabilize joints, do not forget to use bandages, orthoses, special finger rings, and use elbow pads, knee pads and a helmet when playing sports.
In order to reduce the risk of vascular rupture, blood pressure levels should be regularly monitored. It is also necessary to visit an ophthalmologist annually to assess the degree of myopia and be able to promptly identify glaucoma or retinal detachment. When planning a pregnancy, a mandatory consultation with a geneticist is indicated.
Severe pain and instability in the leg joints is a direct indication for using a wheelchair.