In this article we will tell you:
- Causes of strabismus
- Symptoms of strabismus
- Types of strabismus
- Criteria for strabismus
- Diagnosis of strabismus
- Treatment of strabismus
- Conclusion
Strabismus is a disease, the characteristic feature of which is periodic or constant deviation of the visual axis of the eye in relation to the point of fixation and disorder of binocular vision (the ability to see well with both eyes at the same time). The defect has external manifestations, which consist in a violation of the position of the eyeballs. Violation often leads to headaches, dizziness, and general weakness. Depending on the nature of the course and severity, treatment of strabismus is based on the use of conservative correction options, including exercises and wearing glasses, as well as invasive methods - surgery, hardware techniques.
What causes squint?
Depending on the etiology of development, experts distinguish strabismus, which was present at birth and developed during life (for example, due to injury). In the first case, the defect is present at birth or develops during the first six months of the child’s life. It is difficult to establish the exact reason why a deviation appears during the period of intrauterine formation or the early stage of development of a child.
Pathology of the visual organs that arose later is called acquired strabismus. The reasons may be as follows:
- Diseases characterized by damage to the nervous system.
- Stress, nervous shock.
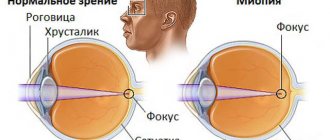
- Ophthalmological diseases of various etiologies and degrees of severity: optic nerve atrophy, eyesore, myopia, astigmatism.
- Pathology of development, injury and damage to the eye muscles.
- Paresis, as well as paralysis.
- Diseases of infectious etiology. Loss of vision, which can be either gradual or rapid.
- Somatic diseases (diseases of the body and internal organs).
- Benign and malignant tumors.
- Frequent and prolonged visual stress on the eyes, as a result of which vision is noticeably reduced.
Strabismus can be fickle and acquired, but you should know that in adulthood, a defect in the organ of vision “pops up” solely against the background of provoking factors. It is important to make a diagnosis and determine the causes of strabismus; this approach allows us to eliminate the primary factors and simplify the treatment process.
What complications should you expect after surgery?
The most common complication that occurs in medical practice after surgery to eliminate strabismus is overcorrection. It is formed when the muscles of the eye organ are excessively lengthened or sewn in. The main reasons for this undesirable effect:
- surgeon error;
- incorrect preliminary calculations;
- the patient’s natural growth, which affects the increase in size of the eye organ.
Recently, experts have found the best way to minimize the risk of such a complication. Increasingly, operations are being carried out not by cutting, but by sewing in muscle folds. In this case, the applied suture is adjustable and the undesirable effect can be corrected in a minimally invasive way.
Formation of a rough scar at the site of muscle cutting and subsequent reattachment. This method of surgical intervention deprives the muscle tissue of mobility and elasticity, which is partially replaced by fibrous tissue. The only alternative at this time is to reduce the size of the excised area.
Strabismus returns (relapses) over time. This complication most often occurs due to the fault of the patient himself, who neglects to comply with all the rules in the postoperative period. In children, relapse can occur due to sudden increases in load on the eye organ. For example, an operation to correct strabismus was performed at the age of five or six years, and after a couple of months the child began to attend school.
The most serious, but very rare complication is damage during the operation to the vagus nerve, which is responsible for the functioning of the lungs, gastrointestinal tract and heart muscles.
Symptoms of strabismus
The symptoms accompanying strabismus vary significantly depending on the course, type and severity of the disease, as well as the age and general health of the person. A common clinical sign indicating the development of strabismus is decreased visual acuity.
The appearance of strabismus before the age of seven is accompanied by a number of the following symptoms:
- A characteristic turn of the head directed towards the squinting eye. The appearance of this sign is possible even against the background of the absence of externally expressed symptoms of eye disease.
- The appearance of problems with focusing the eyes, otherwise - strabismus. The occurrence of this sign (strabismus) is typical for all types of strabismus. Regardless of the reasons why strabismus occurs in children of a younger age category, the following variable symptom typically appears - when moving, the child may bump into various objects, which is due to impaired visual function of the eyes.
- Discrepancy in the synchrony of eye movements.
- Eye discrepancy, which can be determined by exposure to a direct light source.
Regardless of the causes of strabismus, the clinical picture in these cases includes the following signs in adolescents and adults:
- One of the main manifestations is a decrease in visual acuity during strabismus, which is expressed in the blurred perception of visual images by the eyes.
- Increased level of photosensitivity, with prolonged exposure to the sun or in a brightly lit room, vision decreases.
- General symptoms include headaches and systematic dizziness.
- Increased fatigue and blurred vision after short reading.
Parents often wonder whether strabismus can occur in young children and what to do in such cases. In babies less than four months old, eye movements are not synchronous. After reaching the specified age, the eyes take an anatomically correct position. If this does not happen, there is a possibility of developing eye disease.
Recommendations for parents
In order to prevent strabismus and visual impairment in children, it is necessary to control the time they watch TV shows and spend time at the computer. The child should have a properly equipped and well-lit place where he could draw, look at pictures and books.
You should not read while lying down, placing the book too close to your eyes or to the side. You should not buy glasses using the “selection” method without having your vision checked by a specialist. If you have any visual impairment, you should immediately consult a doctor.
Types of strabismus
Depending on how this ophthalmological pathology makes itself felt and what factors provoked the development of the eye disease, experts distinguish two main types of pathology: friendly and paralytic.
- Friendly. This type of disease is divided into 2 subtypes: accommodative (impaired visual perception of the affected eye, can be easily corrected with glasses), partially accommodative, non-accommodative (pathology that cannot be treated conservatively, is formed against the background of congenital anomalies). Typical manifestations of these forms of the disease are the following: absence of double vision in the perception of visual images, preservation of full mobility, identical strabismus angle of the affected eye to the healthy one.
- Paralytic. Caused by damage to certain parts of the brain and nervous system, this type of strabismus is characterized by disturbances of the vertical as well as torsion type (the direction of the affected eye upward or towards the temple), which is taken into account when choosing treatment tactics.
Depending on the characteristics of the involvement of the eyes in the pathological process, a monolateral or alternating type of the disease develops. In the first case, the position of one eye is disturbed. In the second case, there is a violation of the position of both one and the second eye.
Experts also identify the following forms of strabismus:
- Latent and compensated. Treatment with exercises in these cases is not mandatory; only measures that will help prevent complications are permissible. More often, these types of diseases of the visual organs are detected exclusively as part of preventive examinations and do not have external manifestations.
- Subcompensated. Against the background of this form of the disease, a person can control the movements of the eyeballs. External signs indicating that the patient is developing strabismus are barely noticeable. But over time, they become more pronounced; accordingly, it is necessary to correct vision and remove provoking factors as soon as possible, this is also done with the help of exercises.
- Decompensated. It is characterized by pronounced external manifestations and a lack of control regarding the movements of the eyeballs, which means a weakening of muscle tissue.
Treatment methods
Diagnosing pathology is possible only during a comprehensive ophthalmological examination. Specific tests allow you to evaluate the angle of deviation of the eye and impairment of binocular vision.
There are several basic methods for correcting the defect:
- spectacle correction
– prescription of special lenses; - hardware treatment
– a set of orthoptic exercises to develop the muscular structures of the organ of vision; - prismatic compensators
– special lenses for creating individual correction of the optical system for strabismus; - surgical treatment of divergent strabismus
- special operations that can normalize muscle function.
Often patients prefer to start with non-surgical therapy - the risks of surgery become discouraging factors when choosing a treatment method.
Orthoptic treatment of divergent strabismus shows good results. Special sets of exercises have been developed on hardware programs, on a synoptophore, with various lenses and prisms. Prismatic compensators can also be prescribed in the form of glasses - some companies and research institutes are creating glasses for permanent wear with prisms that form binocular vision in patients with strabismus. Courses of treatment are also recommended before surgery - only the readiness of the brain to perceive images from both eyes can reduce the risks of relapse of strabismus and repeated surgical interventions.
Criteria for strabismus
When treating strabismus, the criteria for the development of the disease are taken into account:
- In accordance with the characteristics and time of development of the disease, congenital and acquired forms are distinguished. Experts note that the most common is the first option.
- According to the stability of the deviation of the eyeball from the visual axis, unstable and constant forms are distinguished.
- Depending on how exactly the defect occurs, what manifestations it is accompanied by, for example, rapidly decreasing vision, friendly and paralytic forms are distinguished.
- Depending on how the pathology develops, why this happens, and in which direction the affected eye is deviated, forms of the disease are distinguished: mixed, vertical and horizontal.
Determining the type of disease should be considered as an important aspect, since the features of treatment of strabismus and the choice of medical tactics depend on the form of the pathology.
Diagnosis of strabismus includes:
Diagnosis of pathology includes a wide range of techniques, the most common of which are the following:
- Initial examination. In the later stages of development, external signs of pathology are clearly expressed; in the primary stages, when negative consequences can be avoided, only a specialist can see them. When the initial examination is carried out, the doctor notes the position of the head, as well as the location of the eyeballs.
- Checking visual acuity using special corrective lenses. This method allows you to determine whether the patient’s vision is deteriorating or whether these signs are absent; testing must be done over a period of time.
- Computer refractometry. This research method is necessary to determine the nature and characteristics of refraction - the process of refraction of light waves within the optical system of the eyeball; it should be done when identifying primary signs of the disease.
Additional examination of the patient is required if a paralytic form of the disease is detected.
How is strabismus treated?
Before starting treatment and getting rid of the defect, the patient will need to undergo a series of diagnostic procedures. Depending on why the pathology develops and the degree of its severity, the following treatment options can be chosen:
- Optical correction. To get rid of pathology in the early stages of formation, the patient is required to wear corrective lenses or glasses. Using this treatment method, almost any stage and type of strabismus is completely corrected. To correct the position of the eyeballs, children need to wear glasses on a regular basis.
- Pleoptic therapy (exercises). Using this method, pathology affecting only one eye is treated. The essence of the technique is to turn off the healthy eyeball from the visual process in order to train and correct the position of the affected one. Surgical intervention. Surgery is often used to treat patients under five years of age who do not respond to conservative treatment methods.
To improve results, vision correction during treatment with surgical intervention is carried out in combination with conservative methods of therapy. Doctors warn: in the case of strabismus, consistency in exercises is extremely important. Teach your children to do them regularly along with brushing their teeth.
Rehabilitation period
Although the operation to correct strabismus is performed in one day and the patient is immediately sent home, this does not mean that there is no rehabilitation period. To quickly restore binocular vision, you will need to adhere to certain doctor’s recommendations for some time and perform special eye exercises.
The first day after surgery, the eye organ will be sore, slightly red and inflamed. This is a natural state. There may also be a short-term deterioration in vision. During this period, every movement must be controlled, since any attempts to touch the eye can only result in increasing pain.
Important: Restoration of the tissues of the eye organ and binocular vision occurs after a month. Most patients see a double picture all this time. If after this period vision is not restored, you should consult an ophthalmologist.
In children, adaptation time is significantly reduced. The main thing is to perform the exercises prescribed by a specialist and visit an ophthalmologist.
For active recovery, a specialist may recommend using special corrective glasses, as well as covering the healthy eye from time to time. This will help create stress on the operated organ. The muscles will develop faster and reach the desired level.