DIC syndrome is one of the most common and most severe, life-threatening disorders of the hemostatic system (hemostasis is a complex of body reactions aimed at preventing and stopping bleeding).
Synonyms for DIC syndrome are thrombohemorrhagic syndrome, consumption coagulopathy, hypercoagulability syndrome, defibration syndrome.
DIC syndrome (disseminated intravascular coagulation syndrome) is:
- a secondary pathological process that occurs with constant and prolonged stimulation of the hemostatic system;
- a pathological process that has a phase course, with initial activation and subsequent deep, increasing depletion of all parts of the hemostatic system up to the complete loss of the ability of blood to clot with the development of catastrophic uncontrolled bleeding and severe generalized hemorrhagic syndrome;
- a pathological process in which progressive diffuse intravascular coagulation is noted with multiple and widespread formation of blood microclots and aggregates of its formed elements, which worsens its rheological characteristics, blocks microcirculation in tissues and organs, causes ischemic damage in them and leads to multiple organ lesions.
Causes
The triggering factors for DIC syndrome can be a wide variety of intense or prolonged stimuli, one way or another fitting into Virchow's triad - disturbances in blood circulation, its properties or the vascular wall.
DIC syndrome occurs:
1. In case of violation of the rheological characteristics of blood and hemodynamics
- any kind of shock
- blood loss,
- intoxication,
- sepsis,
- Rhesus conflict pregnancy,
- circulatory arrest and subsequent resuscitation,
- gestosis,
- uterine atony,
- placenta previa,
- uterine massage
2. When blood comes into contact with damaged cells and tissues
- atherosclerosis,
- antenatal fetal death,
- oncological diseases
3. When the properties of the blood change and when thromboplastic substances enter the blood massively
- leukemia,
- amniotic fluid embolism,
- transfusion of incompatible blood,
- septic abortion,
- abruption of a normally located placenta with hemorrhage into the uterus,
- placenta accreta,
- uterine rupture,
- operations on parenchymal organs: uterus, liver, lungs, prostate, kidneys;
- acute radiation sickness,
- long-term compartment syndrome,
- gangrene,
- organ transplantation, chemotherapy, pancreatic necrosis, myocardial infarction, etc.).
Symptoms of DIC syndrome
During DIC syndrome there are 4 stages:
Stage 1 – phase of hypercoagulation and platelet hyperaggregation;
Stage 2 – transitional phase (multidirectional shifts in blood clotting both towards hyper- and hypocoagulation);
Stage 3 – deep hypocoagulation phase (blood does not clot at all);
Stage 4 – resolving phase (either hemostasis parameters are normalized, or complications develop that lead to death).
The symptoms of disseminated intravascular coagulation depend on many factors (the cause that caused it, the clinical picture of shock, disorders of all parts of hemostasis, thrombosis, reduced volume of the vascular bed, bleeding, anemia, dysfunction and dystrophy of target organs, metabolic disorders).
In the first phase, there is increased blood clotting, immediate formation of clots in large vessels and blood clots in small ones (during surgery). It is impossible to take blood from a patient for analysis, as it immediately clots. As a rule, the first phase proceeds very quickly and goes unnoticed by doctors. There is a sharp decrease in blood pressure, the skin is pale, covered with cold sticky sweat, the pulse is weak (thready). Then respiratory failure develops due to lung damage, a wet cough and crepitus in the lungs, cyanosis of the skin, cold feet and hands.
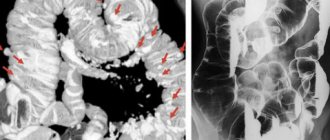
In the second phase, the same symptoms persist as in the first stage of DIC, plus the kidneys (renal failure), adrenal glands, and digestive tract are involved in the process (nausea, vomiting, abdominal pain, diarrhea). Microthrombi form in the brain (headache, dizziness, convulsions, loss of consciousness up to coma, paresis and paralysis, strokes).
The third phase (hypocoagulation stage) is characterized by massive bleeding, both from the original focus and from other organs (intestinal and gastric bleeding due to ulceration of the mucous membrane, blood in the urine - kidney damage, sputum mixed with blood when coughing).
The development of hemorrhagic syndrome is also characteristic (the appearance of massive hemorrhages, hematomas, petechiae, unstoppable bleeding at injection sites and during surgery, bleeding gums, nosebleeds, etc.).
The fourth phase, with timely and adequate treatment, leads to the restoration of hemostasis and stopping bleeding, but often ends in death with massive damage to internal organs and bleeding.
Thrombosis: normal or pathological?
In order to understand what the cause is and what are the mechanisms of occurrence of such a severe disorder as DIC syndrome, you need to know the main stages of blood coagulation.
A person is constantly faced with the risk of possible injuries, from minor scratches or cuts to serious wounds, so nature provides a special protective mechanism - thrombosis, that is, the formation of a blood clot at the site of vessel damage.
There are two oppositely directed systems in the body - coagulation
and
anticoagulant , the correct interaction of which promotes thrombus formation if necessary, as well as the liquid state of blood in the vessels in the absence of any damage.
These hemostatic systems play a very important protective role. Blood clot formation
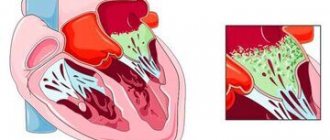
When the integrity of the vascular wall is violated, the coagulation system is activated, a whole cascade of reactions of which leads to the formation of a thrombus (a clot in the lumen of a vessel or chamber of the heart). Plasma proteins, in particular fibrinogen, as well as platelets, coagulation factors produced in the liver, and various enzymes are directly involved in this. The result is the formation of a blood clot that closes the defect in the vascular wall and prevents further bleeding.
To maintain the fluid state of the blood and prevent the uncontrolled formation of blood clots, there are specific antithrombotic mechanisms
, realized by the action of so-called
anticoagulants
- substances that prevent the occurrence of massive thrombosis (plasma proteins, proteolytic enzymes, endogenous heparin). In addition, an obstacle to thrombosis is rapid blood flow and so-called fibrinolysis, that is, the dissolution of the fibrin protein and its removal from the vascular bed with the help of enzymes circulating in the blood plasma and secreted by leukocytes, platelets and other cells. The remains of fibrin after its destruction are absorbed by leukocytes and macrophages.
When the interaction of the components of the hemostatic system changes in various diseases and injuries, discoordination occurs in the work of the coagulation and anticoagulation systems , which contributes to massive uncontrolled thrombus formation along with bleeding. These mechanisms form the basis of the pathogenesis of DIC syndrome, which is a life-threatening complication.
Diagnostics
Basic laboratory tests:
- determination of platelets (with DIC syndrome there is a decrease in platelets in phases 2, 3 and 4);
- blood clotting time (the norm is 5 – 9 minutes, in the 1st stage the indicator is shortened, in subsequent stages the time is lengthened);
- bleeding time (normal 1 – 3 minutes);
- APTT (activated partial thromboplastic time - increase in phases 2 and 3 of DIC syndrome);
- prothrombin time, thrombin time, determination of activated plasma recalcification time - AVR (increase in the second and third stages of DIC syndrome);
- clot lysis (normally not, in phase 3 lysis is rapid, and in phase 4 a clot does not form);
- fibrinogen (normal 2 – 4 g/l, decreases in stages 2, 3 and 4);
- study of the phenomenon of fragmentation of erythrocytes due to damage to them by fibrin threads (normally the test is negative, a positive test indicates disseminated intravascular coagulation syndrome);
- decreased red blood cells (anemia, decreased blood volume);
- decreased hematocrit (hypovolemia);
- determination of acid-base and electrolyte balance.
How is disseminated intravascular coagulation treated?
If you are suffering from disseminated intravascular coagulation, your doctor's first step, if possible, is to treat the underlying cause of your condition. For example, if infection is the underlying cause, you may be prescribed appropriate antibiotics.
You may also be given supportive care (fluid intake) and urine monitoring with a urinary catheter.
The next step is to replace the missing blood components. If your platelet count is low, platelet transfusions . If plasma clotting factors are reduced, they can be replaced with fresh frozen plasma. If fibrinogen levels are low, the doctor may consider a transfusion of cryoprecipitate , which is a fibrinogen-rich substance.
Doctors may consider heparin therapy , which is controversial. Heparin helps stop blood clotting by stopping enzymes that increase blood clotting. However, bleeding may increase in some patients.
Thus, heparin therapy is probably best suited for patients with signs of ischemia (insufficient blood supply) and cyanosis.
Surgery is limited to treating certain underlying causes of DIC, e.g. removal of cancer (malignant formation).
Treatment of DIC syndrome
Therapy for DIC syndrome is carried out by a doctor who has encountered this pathology (that is, the attending physician) together with a resuscitator. In the chronic course of DIC syndrome, its treatment is carried out by a therapist and a hematologist.
First of all, it is necessary to eliminate the cause of DIC syndrome. For example, for sepsis, antibacterial and transufusion (intravenous infusion of blood products) therapy is prescribed, for traumatic shock - adequate pain relief, immobilization, oxygenation and early surgical intervention. Or for tumor diseases - chemotherapy and radiotherapy, for myocardial infarction - relief of pain, restoration of heart rhythm and hemodynamics, for obstetric and gynecological pathologies, radical measures (hysterectomy, cesarean section).
Restoration of hemodynamics and rheological properties of blood is carried out through infusion-transfusion infusions.
An infusion of fresh frozen plasma is indicated, which not only restores the volume of circulating blood, but also contains all coagulation factors.
Crystalloid (saline, glucose) and colloid solutions (polyglucin, rheopolyglucin) in a 4/1 ratio and protein blood products (albumin, protein) are also administered.
A direct anticoagulant is prescribed - heparin. The dose of heparin depends on the stage of DIC syndrome (in phases 1–2 it is significant). In case of significant anemia, fresh (no more than 3 days) red blood cells are transfused.
In the treatment of severe generalized DIC, fibrinogen and blood clotting factor concentrates (cryoprecipetate) are used. Proteolysis inhibitors - antiproteases - are used to suppress tissue proteases that are released when cells are damaged (contrical, trasylol, gordox). Corticosteroids (hydrocortisone, dexamethasone) are also prescribed, as they increase blood clotting.
In parallel, the fight against multiple organ failure is being carried out (supporting the functions of the lungs, kidneys, gastrointestinal tract, adrenal glands). In phases 2–4 of DIC, a mixture of aminocaproic acid, dry thrombin, sodium ethamsylate and adroxon is used to restore local hemostasis. This mixture is introduced into the abdominal cavity through drainages, orally, in the form of tampons into the uterine and vaginal cavity, and wipes moistened with the solution are applied to the wound.
The entire process of intensive therapy takes 1–5 days (depending on the severity of DIC), and subsequent treatment continues until complete or almost complete recovery of all multiple organ disorders.
Appendix A1. Methodology for developing clinical guidelines
Target audience of these clinical recommendations:
— Doctors, anesthesiologists and resuscitators.
— Obstetrician-gynecologists.
— Transfusiologists.