Stevens-Johnson syndrome
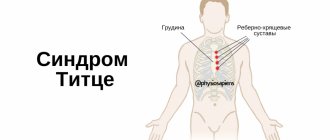
Stevens-Johnson syndrome refers to severe systemic delayed-type allergic reactions (immune complex) and is a severe variant of erythema multiforme (Fig. 1), in which, along with skin damage, there is damage to the mucous membranes of at least two organs [1].
The causes of Stevens-Johnson syndrome are divided into four categories [2].
- Medicines. An acute toxic-allergic reaction occurs in response to the administration of a therapeutic dose of a drug. The most common causally significant drugs: antibiotics (especially penicillin) - up to 55%, non-steroidal anti-inflammatory drugs - up to 25%, sulfonamides - up to 10%, vitamins and other drugs that affect metabolism - up to 8%, local anesthetics - up to 6 %, other groups of medications (anti-epileptic drugs (carbamazepine), barbiturates, vaccines, and heroin [3, 4]) - up to 18%.
- Infectious agents. An infectious-allergic form is distinguished in association with viruses (herpes, AIDS, influenza, hepatitis, etc.), mycoplasmas, rickettsia, various bacterial pathogens (group A b-hemolytic streptococcus, diphtheria, mycobacteria, etc.), fungal and protozoal infections.
- Oncological diseases.
- Idiopathic Stevens-Johnson syndrome is diagnosed in 25–50% of cases.
Clinical picture
Stevens-Johnson syndrome most often occurs between the ages of 20 and 40 years, but cases of its development have also been described in three-month-old children. Men get sick 2 times more often than women. As a rule (in 85% of cases), the disease begins with manifestations of an upper respiratory tract infection. The prodromal flu-like period lasts from 1 to 14 days and is characterized by fever, general weakness, cough, sore throat, headache, and arthralgia. Vomiting and diarrhea are sometimes observed. Damage to the skin and mucous membranes develops rapidly, usually after 4–6 days, and can be localized anywhere, but symmetrical rashes are more typical on the extensor surfaces of the forearms, legs, dorsum of the hands and feet, face, genitals, and mucous membranes. Edema, clearly demarcated, flattened papules of a pink-red color, round in shape, with a diameter of several millimeters to 2–5 cm, appear, having two zones: an internal (grayish-bluish color, sometimes with a bubble in the center filled with serous or hemorrhagic contents) and an external (Red). Diffuse erythema, blisters, and erosive areas covered with a yellowish-gray coating appear on the lips, cheeks, and palate. After opening large blisters, continuous bleeding painful lesions form on the skin and mucous membranes, while the lips and gums become swollen, painful, with hemorrhagic crusts (Fig. 2, 3). The rash is accompanied by burning and itching. Erosive damage to the mucous membranes of the genitourinary system can be complicated by urethral strictures in men, bleeding from the bladder and vulvovaginitis in women. When the eyes are affected, blepharoconjunctivitis and iridocyclitis are observed, which can lead to loss of vision. Bronchiolitis, colitis, and proctitis rarely develop. Common symptoms include fever, headache and joint pain [5].
| Figure 2. Damage to the lips and oral mucosa in Stevens-Johnson syndrome in a 42-year-old patient |
Prognostically unfavorable factors for Stevens-Johnson syndrome and Lyell's syndrome include: age over 40 years, rapidly progressive course, tachycardia with heart rate (HR) more than 120 beats/min, initial area of epidermal lesion more than 10%, hyperglycemia more than 14 mmol /l [6].
The mortality rate for Stevens-Johnson syndrome is 3–15%. When the mucous membranes of internal organs are damaged, stenosis of the esophagus and narrowing of the urinary tract can form. Blindness due to secondary severe keratitis is reported in 3–10% of patients.
Differential diagnosis should be made between erythema multiforme, Stevens-Johnson syndrome and Lyell's syndrome (Table 1). It should be remembered that similar skin lesions can occur with primary systemic vasculitis (hemorrhagic vasculitis, polyarteritis nodosa, microscopic polyarteritis, etc.).
Diagnostics
When collecting anamnesis, the patient should be asked the following questions:
- Has he had any allergic reactions before? What caused them? How did they manifest themselves?
- What preceded the development of an allergic reaction this time?
- What medications did the patient use the day before?
- Were the rashes preceded by symptoms of a respiratory infection (fever, general weakness, headache, sore throat, cough, arthralgia)?
- What measures did the patient take independently and how effective were they?
It is mandatory to record the presence of drug allergies in the medical documentation.
| Figure 3. Symmetrical lesions of the hands, lower extremities and genital mucosa in the same patient |
During the initial examination, pay attention to the presence of changes in the skin and visible mucous membranes, note the nature of the rash, localization, indicate the percentage of skin damage, the presence of blisters, epidermal necrosis; stridor, dyspnea, wheezing, dyspnea, or apnea; hypotension or a sharp decrease in normal blood pressure (BP); gastrointestinal symptoms (nausea, abdominal pain, diarrhea); pain when swallowing, urinating; change of consciousness.
An objective examination includes measurement of heart rate, blood pressure, body temperature, palpation examination of the lymph nodes and abdominal cavity.
Laboratory research:
- Detailed general blood test daily - until the condition stabilizes.
- Biochemical blood test: glucose, urea, creatinine, total protein, bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), C-reactive protein (CRP), fibrinogen, acid-base status (ALS).
- Coagulogram.
- General urine test daily until the condition stabilizes.
- Cultures from the skin and mucous membranes, bacteriological examination of sputum, feces - according to indications.
In order to verify skin rashes and damage to mucous membranes, a consultation with a dermatologist is indicated. If there are signs of damage to other organs and systems, it is advisable to consult other specialists (otolaryngologist, ophthalmologist, urologist, etc.).
Emergency care at the prehospital stage
With the development of Stevens-Johnson syndrome, the main direction of emergency treatment is to replace fluid loss, as in burn patients (even if the patient’s condition is stable at the time of examination). Catheterization of the peripheral vein is carried out and fluid transfusion begins (colloid and saline solutions 1-2 l), if possible, oral rehydration.
Intravenous jet administration of glucocorticosteroids is used (in terms of intravenous prednisolone 60–150 mg). However, the effectiveness of prescribing systemic hormones is questionable. It is considered advisable to use pulse therapy in high doses in the early stages from the onset of an acute toxic-allergic reaction, because their planned administration increases the risk of septic complications and can lead to an increase in the number of deaths [5].
There must be readiness for artificial pulmonary ventilation (ALV), tracheotomy if asphyxia develops, and immediate hospitalization in the intensive care unit [9].
Principles of inpatient therapy
The main measures are aimed at correcting hypovolemia, carrying out nonspecific detoxification, preventing the development of complications, primarily infections, as well as eliminating repeated exposure to the allergen.
It is necessary to discontinue all medications, except for those that are necessary for the patient for health reasons.
Appointed:
- hypoallergenic diet (liquid and pureed foods, drinking plenty of fluids; parenteral nutrition in severely ill patients;
- intensive infusion therapy (electrolyte solutions, saline solutions, plasma-substituting solutions), volume about 6000 ml/day;
- systemic glucocorticosteroids (daily dose in terms of intravenous prednisolone 60–240 mg/day), however, one should remember the likelihood of an increase in the number of complications and deaths;
- measures to prevent bacterial complications: specially created sterile conditions in an open manner (separate room, heated air);
- skin treatment, which is carried out as for burns; in the case of an exudative component, the skin must be dried and disinfected with solutions (saline solutions, 3% hydrogen peroxide solution, etc.); as epithelialization occurs, the solutions can gradually be replaced with creams and ointments (softening and nourishing, corticosteroid). The most commonly used topical corticosteroids: Elokom, Lokoid, Adventan, Celestoderm. For secondary infection, combined ointments are used (corticosteroid plus antibacterial and (or) antifungal): triderm, pimafucort, belogent, etc. The patient's clothing should be made of soft cotton fabrics, in addition, it should be loose;
- treatment of the mucous membranes of the eyes 6 times a day: eye gels (carbomer 974R (oftagel) 1 drop in the affected eye 1–4 times a day), eye drops (azelastine (allowed for children from 4 years old) 1 drop in each eye 2 times per day, etc.), for severe manifestations - corticosteroid eye drops and ointments (prednisolone 0.5%, 1-2 drops 3 times a day, etc.);
- treatment of the oral cavity after each meal (reopolyglucin, hydrogen peroxide, disinfectant solutions, etc.);
- treatment of the mucous membranes of the genitourinary system 3–4 times a day (with disinfectant solutions, solcoseryl ointment, glucocorticosteroid ointment, etc.);
- antibacterial drugs taking into account the results of bacteriological examination in the presence of infection of the skin and urinary tract to prevent the development of bacteremia. The use of penicillin antibiotics is strictly prohibited;
- for skin itching and to prevent repeated allergic manifestations associated with the release of new portions of histamine, antihistamines are used, preferably II and III generations (Table 2).
- symptomatic therapy, especially analgesic drugs, strictly according to indications [10].
A general nonspecific hypoallergenic diet according to A.D. Ado is prescribed as a hypoallergenic diet. It involves excluding the following foods from the diet: citrus fruits (oranges, tangerines, lemons, grapefruits, etc.); nuts (peanuts, hazelnuts, almonds, etc.); fish and fish products (fresh and salted fish, fish broths, canned fish, caviar, etc.); poultry meat (goose, duck, turkey, chicken, etc.) and products made from it; chocolate and chocolate products; coffee; smoked products; vinegar, mustard, mayonnaise and other spices; horseradish, radish, radish; tomatoes, eggplants; mushrooms; eggs; unleavened milk; strawberry, melon, pineapple; butter dough; honey; alcoholic drinks.
Can be used:
- lean beef meat, boiled;
- soups: cereal, vegetable:
– on secondary beef broth;– vegetarian with the addition of butter, olive, sunflower;
- Boiled potatoes;
- porridge: buckwheat, rolled oats, rice;
- one-day lactic acid products (cottage cheese, kefir, yogurt);
- fresh cucumbers, parsley, dill;
- baked apples, watermelon;
- tea;
- sugar;
- compotes from apples, plums, currants, cherries, dried fruits;
- white unsweetened bread.
The diet includes about 2800 kcal (15 g protein, 200 g carbohydrates, 150 g fat).
Possible complications:
- Ophthalmological - corneal erosions, anterior uveitis, severe keratitis, blindness.
- Gastroenterological - colitis, proctitis, esophageal stenosis.
- Urogenital - tubular necrosis, acute renal failure, bleeding from the bladder, urethral stricture in men, vulvovaginitis and vaginal stenosis in women.
- Pulmonological - bronchiolitis and respiratory failure.
- Skin - scars and cosmetic defects that arise during healing and the addition of a secondary infection.
Typical mistakes:
– use of low doses of glucocorticosteroids at the onset of the disease and long-term glucocorticosteroid therapy after stabilization of the patient’s condition;
– prophylactic administration of antibacterial drugs in the absence of infectious complications.
Let us emphasize once again that penicillin drugs are strictly contraindicated and the administration of vitamins (group B, ascorbic acid, etc.) is contraindicated, since they are strong allergens.
The use of calcium preparations (calcium gluconate, calcium chloride) is pathogenetically unjustified and can unpredictably affect the further course of the disease.
Further recommendations
The patient is constantly reminded that medications should be taken only as prescribed by the doctor. The patient is given a reminder about drug intolerance, referred for a consultation with an allergist or clinical immunologist, and is recommended to study at an allergy school. The patient is taught the correct use of emergency medications, injection techniques in case of repeated contact with the allergen and the occurrence of severe acute toxic-allergic reactions (anaphylactic shock). Your home medicine cabinet should include adrenaline, glucocorticosteroids (prednisolone) for parenteral administration, syringes, needles and antihistamines.
Prevention of the development of drug allergies includes compliance with the following rules.
- A thorough collection and analysis of pharmacological history should be carried out.
- The title page of the outpatient and/or inpatient chart should indicate the drug that caused the allergy, the reaction, its type and the date of the reaction.
- You cannot prescribe a drug (and combination drugs containing it) that previously caused an allergic reaction.
- You should not prescribe a drug that belongs to the same chemical group as an allergen drug, taking into account the possibility of developing cross-allergy.
- It is necessary to avoid prescribing multiple medications at the same time.
- The instructions for administering the drug should be strictly followed.
- Prescribe doses of medications in accordance with the age, body weight of the patient and taking into account concomitant pathology.
- It is not recommended to prescribe drugs with histaminoliberation properties (paracetamol, valpromide, valproic acid, phenothiazine neuroleptics, pyrazolone drugs, gold salts, etc.) to patients suffering from diseases of the gastrointestinal tract, hepatobiliary system and metabolism.
- If there is a need for emergency surgery, tooth extraction, or the introduction of radiopaque agents to persons with a history of drug allergies and if it is impossible to clarify the nature of the existing adverse reactions, premedication should be carried out: 1 hour before the intervention - intravenous drip of glucocorticosteroids (4-8 mg of dexamethasone or 30-60 mg prednisolone) in saline and antihistamines.
Thus, Stevens-Johnson syndrome is a serious disease that requires early diagnosis, hospitalization of the patient, careful care and observation, and rational drug therapy.
Literature
- Clinical recommendations. Patient management standards. M.: GEOTAR Medicine, 2005. 928 p.
- Hurwitz S. Erythema multiforme: a review of its characteristics, diagnostic criteria, and management//Pediatr. Rev. 1990; 11:7:217–222.
- Hallgren J., Tengvall-Linder M., Persson M. Stevens-Johnson syndrome associated with ciprofloxacin: A review of adverse cutaneous events reported in Sweden as associated with this drug//J. Amer. Acad. Derm. 2003; 49:5.
- Hofbauer GF, Burg G., Nestle FO Cocaine-related Stevens-Johnson syndrome//Dermatology. 2000; 201:3:258–260.
- Parrillo SJ Stevens-Johnson Syndrome//eMedicine, December 2004. - https://www.emedicine.com/
- Bastuji-Garin S., Fouchard N., Bertocchi M., Roujeau JC, Revuz J., Wolkenstein P. SCORTEN: a severity-of-illness score for toxic epidermal necrolysis // J. Invest Dermatol. 2000; 115(2): 149–153.
- Shear N., Esmail N., Ing S., Kerba M. Dermatology/Review Notes and Lecture Series//MCCQE, 2000; 21.
- Drannik G. N. Clinical immunology and allergology. M.: Medical Information Agency LLC, 2003. 604 p.
- Vertkin A. L. Emergency medical care. Guide for paramedics: textbook. allowance. M.: GEOTAR Medicine, 2005. 400 p.
- Immunopathology and allergology. Algorithms for diagnosis and treatment / ed. R. M. Khaitova. M.: GEOTAR Medicine, 2003. 112 p.
A. L. Vertkin, Doctor of Medical Sciences, Professor A. V. Dadykina , Candidate of Medical Sciences NNPOS MP, MGMSU, CPC and teaching staff of Nizhny Novgorod State Medical Academy, Moscow, Nizhny Novgorod
Epidemiology
Since the 70s, medicine has kept an annual record of the prevalence of Lyell's syndrome. According to various authors, rates range from 0.4–1.3 cases per 1 million population per year. Mortality rates range from 20–60% of the number of cases, depending on the state of the region's health care system. Thus, the number of deaths from this pathology throughout the world per year is in the thousands. Among immediate allergic reactions, Lyell's syndrome is second only to anaphylactic shock in terms of mortality. In the general structure of drug allergies, the share of Lyell's syndrome is 0.3%. Women are more often affected: the ratio to male patients is 1.5:1. There was no direct relationship between the risk of the disease and age. Patients who have previously had Lyell's syndrome, especially in childhood, are considered a risk group.
The most common form of the syndrome is medicinal, up to 80% of all cases. After medicinal, the second most common cause is malignant neoplasms (especially lymphomas). The frequency of idiopathic cases of the syndrome is 5–10%.
In children, Lyell's syndrome more often - up to 60% of cases - has an infectious etiology. A special risk group for the manifestation of the disease among children is those who suffered from acute respiratory viral infections at an early age and underwent a course of treatment with NSAIDs in connection with this.
Forecast
Since 2011, the SCORTEN scale for assessing the severity of Lyell's syndrome has been widely used in the West. It takes into account the following prognostic factors:
- patient age > 40 years;
- Heart rate > 120 beats. in min.;
- presence of concomitant malignant oncological disease;
- affected body surface area > 10%;
- blood urea level > 10 mmol/l;
- plasma bicarbonate level
- blood glucose > 14 mmol/l.
The presence of each factor increases the risk of death. Thus, the approximate risk of death is: in the presence of 1 factor - up to 3.2%; 2 factors - 12.1%; 3 factors - 35.3%; 4 factors - 58.3%; 5 or more factors – 90%.
Clinical case
In 2009, in Donetsk, I witnessed a rare case for Donbass (only 6 cases in the Donetsk region from 1991 to 2013!) case of Lyell's syndrome.
Patient: 37 years old. Allergic and infectious anamnesis are not burdened. Three days before admission, she fell ill with a cold. She was treated with “familiar” medications: cough tablets, eye drops, nasal drops, vitamins. From the evening of the second day, itching and rashes appeared. She took suprastin on her own. After short-term relief, the condition worsened. In the evening on the third day, after fainting, she was taken to the city hospital by emergency medical services, and within a few hours was transferred to a regional clinic. A woman was admitted with hyperemic skin on her chest, shoulders, and inner thighs. On the third day, bubbles filled with cloudy contents appeared. The volume of others reached 100 ml. Throughout the entire period, hyperemia of the eyelids, sclera, mucous membranes of the oral cavity, and perianal area persisted.
From the third day, the combustiologist made repeated attempts to close the wound surface of the xenoskin. However, short-term periods of calm were replaced by psychomotor agitation in the patient, which led to displacement of the bandages and xenoskin. Not a single flap took root. Over the course of two weeks in the intensive care unit, the patient spent more than half of the time in forced medicated sleep. And from the sixth day, when the patient’s condition became critical, she was transferred to permanent mechanical ventilation.
In this case, Lyell's syndrome was diagnosed within two days after the patient was admitted to the hospital; the course of the disease was not lightning fast, but rather acute; Asymptomatic therapy was carried out, but it was not possible to save the woman.
How to avoid mistakes during treatment?
- The treatment process should not be started with small dosages of corticosteroids, nor should they be used after the end of treatment;
- If the examination does not reveal infectious processes, then antibiotics should not be used. It should be noted that vitamin preparations and penicillin antibacterial agents are powerful allergens, and they should not be present during the treatment process;
- Treatment for Stevens-Johnson syndrome is similar to standard treatment for an allergy attack. But given the complexity of the disease, the patient urgently needs to be hospitalized and in each case an individual course of treatment should be prescribed based on the results of examinations and tests.
Possible complications
Each disease can cause certain complications . As for Stevens-Johnson syndrome, they manifest themselves in the following:
- blood infection. When bacteria enter the bloodstream, they spread throughout the body, causing sepsis. It progresses very quickly and in some cases causes organ failure and shock to the patient;
- secondary skin infection can provoke a variety of complications;
- with severe damage to the organs of vision, partial loss of vision and even complete blindness may occur;
- damage to internal organs causes their deformation. This applies to the genitourinary tract, heart, liver, kidneys, lungs.
According to statistics, approximately 10–15% of patients with Stevens-Johnson syndrome have a fatal outcome.
Etiology
Discussions about the etiology and pathogenesis of Lyell's syndrome continue. The most studied drug form of the disease, which develops due to a violation of the body’s ability to neutralize reactive intermediate drug metabolites. These metabolites interact with tissues, resulting in the formation of an antigenic complex, the immune response to which initiates the development of the disease.
In fact, a genetic predisposition to this pathology has also been proven, in particular in individuals with a number of HLA histological compatibility complex antigens: A2, A29, B12, B27, DR7. The presence of chronic foci of infection in the body (sinusitis, tonsillitis, cholecystitis, etc.), leading to decreased immunity, increases the risk of disease. HIV-infected patients are a special risk group: their risk of developing Lyell's syndrome is 1000 times higher than in the general population.
Diagnostics
For differential and laboratory diagnosis, provocative tests are not performed, since the risk of uncontrolled complications is high. The most common are extraorganismal diagnostic tests based on the reactions of the patient’s blood cells to a substance that has sensitized the body. These include: the Shelley basophil degranulation test, the Fleck leukocyte agglomeration test, the blast transformation reaction of lymphocytes, hemolytic tests.
HIV-infected patients are 1000 times more likely to develop Lyell's syndrome than the general population.
Apoptosis of keratinocytes is one of the first tissue morphological signs of Lyell's syndrome. Needle biopsy using frozen skin sections is becoming increasingly common. This reveals the absence of typical acantholytic cells, total epidermal necrolysis, sub- and intraepidermal blisters.
Material and methods
A retrospective analysis of the medical records of 147 patients with SSc and Lyell's syndrome who were hospitalized in the allergy department of the State Budgetary Healthcare Institution of the Republic of Belarus City Clinical Hospital No. 21 (Ufa) in 2008–2018 was carried out. All patients - 54 (37%) men and 93 (63%) women - were under our supervision. The average age of the patients was 46.65±1.4 years. The diagnosis of SSc was established on the basis of a complex of studies, which included anamnesis, objective examination, laboratory (general and biochemical blood tests, urinalysis) and instrumental (ECG, chest x-ray) studies. In patients with SSc of viral etiology, a serological enzyme immunoassay was performed to detect viral antibodies of the IgG and IgM classes in the blood serum to herpes simplex virus (HSV), cytomegalovirus (CMV), and Epstein-Barr virus (EBV). The study used an analytical method (analysis and substantiation of the results obtained based on data from specialized literature) and a statistical method - statistical data processing using the Microsoft Office Excel 2013 software package.