Zomig®
Zomig is not intended for the prevention of migraine attacks.
Zomig has a pronounced effect on migraine with and without aura and on migraine associated with menstruation. The effectiveness of the drug is not affected by the gender and age of the patient, the duration of the attack, the presence of nausea before taking the drug and the use of conventional drugs for the prevention of migraine attacks.
The drug should be used only when a diagnosis has been established. Other possible serious neurological conditions should be excluded before using the drug.
There are currently no data on the use of Zomig for hemiplegic or basilar migraine.
Patients with migraine may be at increased risk of developing cerebrovascular accidents. Hemorrhagic stroke, subarachnoid stroke, ischemic stroke and other cerebrovascular accidents have been reported in patients taking 5HT1B/1D serotonin receptor agonists.
Very rarely, when using this class of drugs (5HT1B/1D-serotonin receptor agonists), coronary artery spasms, angina pectoris, or the development of myocardial infarction were observed. Patients at high risk of developing coronary artery disease are recommended to undergo an examination of the state of the cardiovascular system before starting to use the drug. In very rare cases, serious cardiovascular complications can develop in patients who have no indication of a history of cardiovascular disease.
Atypical sensations in the cardiac region have been reported when using Zomig (as well as other serotonin 5HT1B/1D receptor agonists). If chest pain or symptoms of coronary artery disease occur, you should stop taking zolmitriptan until appropriate medical evaluation is performed.
Zomig can cause a slight transient increase in blood pressure (like other serotonin 5HT1B/1D receptor agonists) regardless of a history of arterial hypertension; very rarely such an increase in blood pressure was clinically significant.
When using Zomig (as well as other serotonin 5HT1B/1D receptor agonists), anaphylactic/anaphylactoid reactions were rarely observed.
Excessive use of antimigraine drugs may lead to an increase in the frequency of headaches, potentially requiring discontinuation of treatment.
Use in pediatrics
Safety and effectiveness of Zomig in children and adolescents under 18 years of age
not installed.
Impact on the ability to drive vehicles and operate machinery
There was no significant deterioration in psychomotor tests when taking Zomig at a dose of up to 20 mg. It is unlikely that the use of the drug will impair the patient's ability to engage in potentially hazardous activities, but the patient should be warned about the possibility of drowsiness.
Zomig in the treatment of migraine attacks
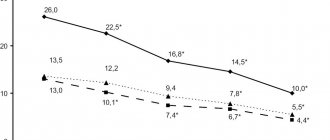
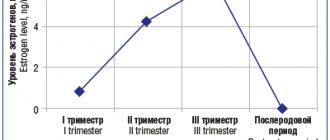
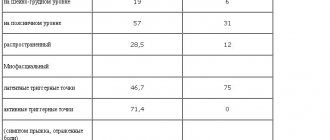
Among the various types of primary headaches, migraine is the most common, the frequency of which in the population is 13–20%. The disease is more common in women, and the “peak” of its prevalence occurs at the most working age – 35–45 years [20,28]. Due to its high prevalence, which impairs the ability of patients to work and leads to significant economic losses, migraine, according to the decision of the World Health Organization, is included in the list of 19 diseases that most disrupt the social adaptation of patients. There are 2 main forms of migraine – migraine with aura and migraine without aura [1,18]. Migraine without aura (previously used terms - simple migraine, hemicrania) is characterized by repeated attacks of headache lasting from 4 hours to 3 days. Its typical manifestations are unilateral localization, pulsating nature, moderate or severe intensity, aggravation with movement and the presence of accompanying symptoms: nausea, vomiting and/or photophonophobia. A distinctive feature of migraine with aura (previously used terms - classical migraine, associated migraine) is the presence of reversible focal neurological symptoms, most often visual (aura), usually increasing within 5-20 minutes and lasting no more than an hour, followed by (less often - simultaneously with them) headache occurs, the characteristics of which are similar to those for migraine without aura [1,18]. Central and peripheral mechanisms are involved in the genesis of a migraine attack. The generator of a migraine attack is the serotonergic and adrenergic neurons of the upper parts of the brain stem (the locus coeruleus, raphe nuclei, gray matter around the aqueduct of Sylvius), which have increased excitability in patients with migraine. The result of their paroxysmal activity, transmitted along numerous perivascular nerve fibers, is the development of neurogenic inflammation in the meningeal and cranial arteries. It is caused by the release of vasoactive peptides (substance P and neurokinin A) into their wall, leading to extravasation of plasma proteins, degranulation of mast cells, adhesion and aggregation of platelets, and activation of the endothelium. Irritation of the afferent sensory fibers of the trigeminal nerve, caused by neurogenic inflammation, is transmitted to its sensory nucleus, and then to the optic thalamus and cortical sections of the sensory analyzer, which leads to the formation of pain [23,30]. Unraveling the pathophysiological mechanisms of migraine attacks is important for the development of their pathogenetic treatment. Treatment of migraine attacks presents considerable difficulties, which are associated with frequent, uncontrolled use of analgesics, leading to worsening of the pain syndrome with the development of abusive headaches. A revolutionary achievement in the treatment of these types of primary headaches was the discovery of triptans, selective agonists of 5HT1B/D receptors, which are involved in the modulation of the central and peripheral effects of the trigemenovascular system. The first in a series of these drugs was sumatriptan, which began to be used in the clinic in 1990 and which , as clinical trials have shown, is an effective remedy for relieving migraine attacks [31]. However, it soon became obvious that some of its characteristics need to be improved (rate of absorption after oral administration, bioavailability, duration of maintaining therapeutic concentration in the blood, effect on the coronary arteries, peripheral mechanism of action) [7]. This led to the creation of second-generation “triptans”, to which Zomig belongs. Zomig is a selective serotonin receptor agonist that penetrates the blood-brain barrier and therefore acts not only on the peripheral, but also on the central part of the trigemen-vascular system. The mechanisms of action of Zomig, pathogenetically significant for the relief of headache attacks, include: 1) reduction of neurogenic inflammation due to the binding of Zomig to presynaptic serotonergic autoreceptors of the efferent fibers of the trigemenal nerve, which inhibits the release of neuropeptides into the vascular wall; 2) vasoconstriction; 3) reduction of pain afferentation due to inhibition of depolarization of the trigeminal nerve terminals in the vascular wall; 4) inhibition of brain stem structures involved in the perception of pain [13–16]. Zomig is produced in the form of regular tablets, lingual lozenges and nasal spray [3,6,11,17,22,27]. A study of the pharmacokinetics and pharmacodynamics of Zomig showed that it is rapidly absorbed when administered orally, with greater bioavailability (40%) and a lower effective dose (2.5 mg) than sumatriptan (14%, 100 mg, respectively). The maximum concentration of the drug in the blood occurs between 2 and 4 hours after oral administration, with 75% of the maximum concentration achieved within the first hour [7,8,13]. About 1/3 of the drug is excreted by the kidneys, 2/3 is metabolized primarily in the liver. The effect of Zomig when administered intranasally begins earlier than when taken orally [4,33]. For migraine, Zomig is used to treat attacks without aura and with aura, menstrually-dependent attacks, attacks that develop upon awakening and are characterized by severity and resistance to traditional therapy [17,25,26,29]. The effectiveness of Zomig does not depend on the age, gender, weight of patients, or whether the patient is taking other drugs [32]. Zomig is usually taken at the very beginning of a migraine attack, but it is also effective when taken later, when the headache has already lasted for 4 hours or more. The latter circumstance is very significant from a practical point of view, since at the beginning of a migraine attack the medicine may not be “at hand” [25]. The optimal dose of Zomig, providing the most favorable ratio between the effectiveness and tolerability of the drug, is 2.5–5 mg [13]. Double-blind placebo-controlled studies, including almost 2.5 thousand patients, showed the high effectiveness of Zomig in the treatment of migraine attacks [13,25]. 1 hour after taking 2.5 mg of the drug, a significant improvement in condition was noted in 40% of patients, after 2 hours - in 64%, after 4 hours - in 73% of patients. Taking 5 mg of Zomiga reduced or eliminated headaches after an hour in 73% of patients, and after 2 hours – in 81% of patients [32]. Increasing the dose of the drug to 10–25 mg did not increase its effectiveness [13,25]. The effectiveness of the drug depended on the severity of the initial headache: after 2 hours it disappeared in 35% of patients with an initially severe migraine attack, in 57% of patients with a moderate attack, and in 80% of patients with a mild migraine attack [32]. In 19–24% of patients, 4 hours after taking 2.5–5 mg of Zomiga, moderate or severe headache remained, and in 15–30% of patients, after an initial improvement in condition, a recurrence of headache was observed during the first day. With repeated administration of 2.5–5 mg of Zomig, improvement occurred in 90–95% of patients [25,32]. Over time, the effectiveness of Zomig does not decrease [32]. Taking Zomig not only reduces headaches - the main manifestation of migraine, but also its accompanying symptoms - nausea, photo-, phonophobia. After 2 hours, their severity decreased by 20–39–40%, respectively [13,25]. In the treatment of acute migraine attacks, Zomiga 2.5 mg is similar in effectiveness to almotriptan 12.5 mg, eletriptan 40 mg, sumatriptan 50 mg and is more effective than naratriptan 2.5 mg in relieving pain 2 hours after taking the drug. Its effectiveness is comparable to 10 mg of rizatriptan in reducing or eliminating headaches, but is less effective in maintaining a lasting effect [5]. Side effects after a single dose of Zomig, according to placebo-controlled studies, were mild or moderate in intensity [12]. Among the side effects, the most frequently observed were general weakness, heaviness, dry mouth, dizziness, drowsiness, paresthesia, and a feeling of warmth. However, at least one of these side effects was observed in 46% of cases with a dose of Zomig 2.5 mg and in 58% with a dose of 5 mg (compared to 29% with placebo). Severe side effects were observed in less than 1% of patients, that is, with the same frequency as in the group receiving placebo. Side effects in the form of discomfort in the heart, sometimes occurring when taking selective serotonin receptor agonists, were rare (1-2%), were mild and disappeared quickly. The incidence of side effects did not increase when the dose of Zomig was increased from 2.5 to 20 mg. With repeated and sufficiently long-term use of the drug, the frequency of side effects did not increase [32]. Only two side effects among more than 2 thousand patients who took Zomig repeatedly during the year were considered serious. One of them was represented by a spasm of the pharyngeal muscles, which went away on its own after 2 hours, the other was an increase in migraine attacks. During long-term use of Zomig, only 8% of patients were forced to abandon it due to side effects [32]. Taking Zomig does not cause an increase in blood pressure, heart rhythm disturbances, or ischemic changes on the ECG, even in persons over 65 years of age and in persons suffering from mild/moderate controlled arterial hypertension [12,21]. Taking Zomig, either single-dose or long-term, is not accompanied by any significant changes in clinical and biochemical blood tests or urine tests. The drug does not affect blood circulation in the brain, since 5HT1B/1D receptors are predominantly located in the cranial vessels [12]. Apparently, due to the latter circumstance, taking the medicine is safe for migraine with aura, when there is a danger of developing a migraine infarction. The good tolerability and safety of Zomig is confirmed by clinical data that a 10-fold increase in its dose does not cause any serious consequences [13]. Along with the usual tablet form of Zomig, there are lingual lozenges (instantly dissolving and quickly entering the bloodstream), which are currently not yet registered in Russia. Their effectiveness, safety and low incidence of side effects have been shown in clinical trials [11,26,27]. An analysis of the attitudes of patients and emergency department physicians toward the use of 2.5 mg Zomiga lingual tablets for the treatment of migraine attacks during a 6-month international study showed the following. The vast majority of patients (85.7%) were satisfied with the results of treatment and wanted to continue taking this form of Zomig in the future, preferring it to other medications (including other triptans). Doctors continued to prescribe this drug to more than two-thirds of patients with migraine attacks. However, it is not known whether this preference is due to the drug itself or its specific form [26]. The form of Zomig in the form of a spray for intranasal use is also a new form of the drug, not yet registered in Russia. Zomig in the form of a spray is effectively used in the treatment of migraine attacks, especially in cases where oral administration of the drug is difficult due to severe nausea and vomiting. Compared to the tablet form, the drug is absorbed faster and has a faster therapeutic effect. In a randomized, double-blind, placebo-controlled study, the intranasal spray was shown to be rapid, effective and well tolerated. The effectiveness of the drug and its tolerability do not decrease with long-term use [4,10,17,24]. The nasal spray has been successfully used not only in adults, but also in children and adolescents, and its pharmacokinetic profile is comparable to that in adults [19]. A prospective study assessing patients' preference for using different dosage forms of Zomig in the treatment of a migraine attack showed the following. After 4 months of using different forms of the drug, 46.9% of patients preferred lingual lozenges, 43.8% - nasal spray and 6.3% of patients - the usual tablet form. The choice of lingual tablets was justified by convenience and, to a lesser extent, speed of action; the choice of spray was based on the speed of onset of action and overall effectiveness [9]. In conclusion, it should be noted once again that Zomig, a selective serotonin receptor agonist with peripheral and central action, is highly effective in the treatment of migraine attacks and cluster headaches, is well tolerated by patients and does not reduce its effectiveness over time. Literature 1. International classification of headaches. Full Russian version. 2nd edition. International Headache Society. 2003. 2. Bahra A, Gawel MJ, Hardebo J–E, Millson D, Brean SA, Goadsby PJ. Oral zolmitriptan is effective in the acute treatment of cluster headache. Neurology. 2000;54:1832–1839 3. Bahra A., May A., Goadsby PJ Cluster headache: a prospective clinical study in 230 patients with diagnostic implications. Neurology 2002;58:354–361. 4. Charlesworth BR, Dowson AJ, Purdy A, et al. Speed of onset and efficacy of zolmitriptan nasal spray in the acute treatment of migraine: a double–blind, placebo–controlled, dose–ranging study versus zolmitriptan tablet. CNS Drugs. 2003;17:653–667. 5. Chen LC, Ashcroft DM. Meta-analysis of the efficacy and safety of zolmitriptan in the acute treatment of migraine. Headache. 2008;48(2):236–47. 6. Cittadini E; May A, Straube A, Evers S. Effectiveness of intranasal Zolmitriptan in acute cluster headache. A randomized, placebo–controlled, double–blind crossover study. Arch Neurol. 2006; 63:1537–1542. 7. Dienner HC, Gendolla A, Juptner M., Kaube H., Limmorth V. Emerging treatment in headache. Eur. Neurol. 1997. – V.38. – P. 167–174. 8. Dixon R., Warrander A. The clinical pharmacokinetics of zolmitriptan. Cephalalgia 1997;17(suppl 18):15–20. 9. Dowson A, Bundy M, Salt R, Kilminster S. Patient preference for triptan formulations: a prospective study with zolmitriptan. Headache. 2007;47(8):1144–51. 10. Dowson A, Charlesworth B, Purdy A, Becker WJ, Boes–Hansen S, Farkkila M. Tolerability and consistency of effect of zolmitriptan nasal spray in a long–term migraine treatment trial. CNS Drugs. 2003;17: 839 –851 11. Dowson AJ, MacGregor EA, Purdy RA, et al. Zolmitriptan orally disintegrating tablet is effective in the acute treatment of migraine. Cephalalgia. 2002;22:101–6. 12. Edmeads JG, Millson DS Tolerability profile of Zolmitriptan (ZomigTM; 311C90) a novel dual central and peripherally acting 5HT1B/1D agonist. Cephalalgia 1997;17(suppl. 18):41–52. 13. Ferrari MD 311C90: Increasing the options for therapy with effective acute antimigraine 5HT1B/1D receptor agonist. Neurology 1997;48(suppl 3):21–24. 14. Ferrari MD, Saxena PR 5–HT1 receptors in migraine pathophysiology and treatment. Eur. Neurol 1995; 2:5–21. 15. Goadsby PJ, Hoskin KL Inhibition of trigeminal neurons by intravenous administration of the serotonin (5HT)1B/1D receptor agonist zolmitriptan (311C90): are brain stem sites therapeutic targets in migraine? Pain 1996; 67:. 355–359. 16. Goadsby PJ, Knight YE Direct evidence for central sites of action of zolmitriptan (311C90): an autoradiographic study in cat. Cephalalgia 1997;17:153–158. 17. Goadsby PJ, Yates R. Zolmitriptan intranasal: a review of the pharmacokinetics and clinical efficacy. Headache. 2006;46:138–149. 18. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders (second edition). Cephalalgia. 2004;24(suppl 1):1–160 19. Lewis DW, Winner P,. Hershey AD et al. Efficacy of zolmitriptan nasal spray in adolescent migraine. Pediatrics 2007; 120(2):390–396. 20. Lipton RB, Stewart WF, Diamond S. et al. Prevalence and burden of migraine in the United States: results from the American Migraine Study II. Headache 2001; 41: 646–657. 21. Martin GR Pre–clinical pharmacology of zolmitriptan (ZomigTM; formely 311C90), a centrally and peripherally acting 5HT 1B/1D agonist for migraine. Cephalalgia 1997;17(suppl. 18):4–14. 22. Mathew NT, Kailasam J, Seifer T, Bouton T. Zolmitriptan (Zomig) nasal spray in cluster headache attacks; a single–blind observation—a preliminary report [abstract]. Headache. 2004;44:483. 23. Moscowitz MA, Buzzi MG, Sakas DE, Linnik MD Pain mechanisms underlying vascular headache. Rev. Neurol. 1989;145:181–193. 24. Rapoport AM, Mathew NT, Silberstein SD, Dodick D, et al Zolmitriptan nasal spray in the acute treatment of cluster headache: a double–blind study. Neurology. 2007 28; 69(9): 821–826. 25. Schoenen J., Sawyer J. Zolmitriptan (Zomig TM 311C90), a novel dual central and peripheral 5HT 1B/1D agonist: an overview of efficacy. Cephalalgia 1997; 17 (suppl. 18): 28–40. 26. Shapero G, Dowson A, Lacoste J–P, Almqvist P. Improved migraine management in primary care: results of a patient treatment experience study using zolmitriptan orally disintegrating tablet. Int J Clin Pract. 2006; 60(12): 1530–1535. 27. Spierings ELH, Rapoport AM, Dodick DW, Charlesworth B. Acute treatment of migraine with zolmitriptan 5 mg orally disintegrating tablet. CNS Drugs. 2004;18:1133–41. 28. Stewart WF, Lipton RB, Celentano DD, Reed ML Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA 1992; 267:64–69. 29. Tuchman M, Hee A, Emeribe U, Silberstein S. Efficacy and tolerability of zolmitriptan oral tablet in the acute treatment of menstrual migraine. CNS Drugs. 2006;20(12):1019–1026. 30. Welch KM, Cutrer FM, Goadsby J. Migraine pathogenesis. Neural and vascular mechanisms. Neurology 2003; 60(Suppl 2):S9–S14. 31. Wilkinson M., Pfaffenrath V., Schoenen J. et.al. Migraine and cluster headache – their management with sumatriptan: a critical review of the current clinical experience. Cephalalgia 1995; 15: 337–357. 32. Zagami AS 311C90: long–term efficacy and tolerability profile for the acute treatment of migraine. Neurology 1997; 48(suppl. 3):S25–S28. 33. Zingmark P–H, Yates R, Hedlund C, Kagedal M. True nasopharyngeal absorption of zolmitriptan following administration of zolmitriptan nasal spray [abstract]. Eur J Neurol. 2003;10(suppl 1):76.