Hyperemia is
The definition of Hyperemia comes from the merger of two Greek words, where “hyper” means too much, and “haima” means blood. When blood accumulates in some part of the body or near some organ, we speak of hyperemia. Externally, it manifests itself as redness of the problem area, and sometimes the body temperature may rise locally. Sometimes a rush of blood causes tissue swelling.
There are several reasons that cause hyperemia. First of all, possible pathologies of the blood supply are identified: the inflow and outflow of blood in a specific area. If there are no problems in the circulatory system, then other possible causes are determined, including:
- temperature changes;
- stress;
- hormonal disorders;
- allergic reactions;
- infectious lesion;
- burn.
It is necessary to eliminate hyperemia from the diagnosis, since it is not a disease in itself, but is considered by medicine exclusively as a symptom.
Types of hyperemia
Hyperemia is primarily considered as a pathology of the circulatory system. There are two types of pathological hyperemia:
- arterial;
- venous.
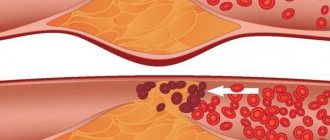
Arterial is called excessive blood supply to an organ when the arteries supply large volumes of blood that the venous system does not have time to remove. Arterial hyperemia can be physiological when more blood begins to flow to the organ during increased load. And venous is called hyperemia, which occurs during normal blood supply, which the venous system cannot drain due to the resulting pathology. For example, with blockage, thrombosis, or atherosclerosis, the lumen of the vascular bed is significantly reduced, and the passage of blood flow is significantly hampered.
The cause of venous hyperemia may be low blood rheology. When it is thick, it is difficult for the heart to pump it throughout the body system. In such a situation, you need to undergo an examination to confirm the problem, and in case of really thick blood, the doctor will prescribe treatment. Most often, it is enough to buy a drug that thins the blood and reduces the risk of blood clots.
The neurotonic type of hyperemia is said to occur when the tone of the nerve conductors increases under the influence of certain factors. First of all, this is facilitated by emotional activity. The second factor that increases the tone of nerve fibers is infectious diseases affecting the nervous system.
Along with an increase in the conductivity of nerve fibers, there is also a reverse reaction - a decrease in tone. As a rule, this is a temporary phenomenon caused by many reasons, such as tissue compression, swelling, hypothermia. As soon as the obstacle to the passage of arterial blood is removed, the tissues are filled with biological fluid with increased intensity, which causes the effect of hyperemia.
Circulatory disorders
General information
The health of the body depends on the condition of the circulatory system. Violation of the blood supply to an organ of the body leads to the fact that the tissues cannot receive the required amount of nutrients and oxygen. As a result, a person’s metabolism slows down and hypoxia develops. In addition, metabolism slows down. Hypoxia develops - low oxygen content in the body or individual organs and tissues. This can lead to the development of serious diseases. As a result, the health of the body as a whole depends on the state of the circulatory system.
Circulatory disorders
Ensuring blood flow is a complex process that depends on the functioning of the heart and the integrity of blood vessels. Depending on the location, blood circulation can be:
- general;
- local.
General disorders can occur in the body as a result of disruption of the heart, changes in the physicochemical properties of the blood. Disorders of blood and lymph circulation are caused by structural and functional damage to the vascular bed in any of its sections - in one organ, part of an organ or part of the body.
What diseases cause circulatory disorders
It is necessary to understand that the division of circulatory disorders into general and local is quite arbitrary, since in terms of reducing blood pressure in the aorta it leads to a decrease in blood supply to the renal cortex. Which, in turn, activates the renin-angiotensin system and causes an increase in blood pressure.
Local circulatory disorders are a consequence of general disorders. With general venous congestion, thrombosis of the veins of the lower extremities often develops.
Myocardial infarction is the first cause of heart failure, and bleeding as a local process can be the cause of general acute anemia.
General circulatory disorders:
- general arterial plethora;
- venous congestion;
- anemia (acute or chronic);
- blood thickening;
- blood thinning;
- shock;
- DIC syndrome.
Arterial hyperemia is an increase in the number of blood cells (erythrocytes), sometimes combined with an increase in the volume of circulating blood. The process is relatively rare: when climbing to a height, in residents of mountainous areas, in people with lung pathologies, as well as in newborns. Symptoms may be as follows:
- redness of the skin;
- increased blood pressure.
Arterial congestion is of greatest importance in Vaquez disease (polycythemia vera), a disease in which there is a true overproduction of red blood cells.
General venous congestion
One of the most common types of general circulatory disorders is general venous congestion. It is a clinical and morphological manifestation of pulmonary heart failure.
Three main factors play a role in the pathogenesis of general venous congestion
- disturbance of heart activity;
- pulmonary diseases;
- chest injuries.
Cardiac dysfunction or heart failure may be associated with acquired and congenital heart defects. Other reasons could be:
- inflammatory heart diseases (myocarditis, endocarditis);
- cardiosclerosis of various etiologies (atherosclerotic, post-infarction);
- myocardial infarction.
Pulmonary diseases are accompanied by a decrease in the volume of vessels in the pulmonary circulation:
- pneumosclerosis of various etiologies;
- emphysema;
- chronic nonspecific pneumonia;
- pneumoconiosis.
In case of damage to the chest , as well as the pleura and diaphragm, the suction function of the chest is impaired:
- pleurisy;
- pneumothorax;
- chest deformities.
Acute venous congestion is a manifestation of the syndrome of acute heart failure and hypoxia . There may be several reasons, namely:
- myocardial infarction;
- acute myocarditis;
- pulmonary embolism;
- pneumothorax;
- all types of asphyxia.
As a result of hypoxia , the histohematic barrier can be damaged and capillary permeability increases. In addition, the following is observed in the tissues:
- venous stagnation;
- plasmorrhagia;
- edema;
- stasis in capillaries.
Dystrophic and necrotic changes appear in parenchymal organs. The cause of venous congestion of the lungs is left ventricular heart failure. Acute venous congestion causes dilation of the alveolar capillaries, which is accompanied by pulmonary edema. may also occur .
General anemia
Depending on the etiology and pathogenesis there are:
- acute anemia;
- chronic anemia.
General acute anemia develops with large blood loss, due to a decrease in circulating blood volume (CBV) in the general circulation in a short period of time.
Causes of acute anemia:
- injuries with damage to organs, tissues, blood vessels;
- spontaneous rupture of a large, pathologically altered vessel or heart;
- rupture of a pathologically altered organ (ectopic pregnancy, pulmonary tuberculosis, gastric ulcer).
Symptoms of the disease are expressed:
- pale skin;
- dizziness;
- frequent weak pulse;
- low blood pressure.
Patients die as a result of hypovolemic shock.
Chronic anemia (anemia) is a decrease in the number of red blood cells and/or hemoglobin content in a volumetric unit of blood. The total volume of circulating blood in the body does not change. Causes of general chronic anemia:
- diseases of the hematopoietic organs (anemia);
- infections (tuberculosis, syphilis);
- parasites (helminthic infestations);
- exogenous intoxication (poisoning with lead, benzene, carbon monoxide);
- endogenous intoxication (poisoning with nitrogen metabolism products).
- starvation;
- avitaminosis.
Clinical manifestations of the disease:
- pallor,
- weakness;
- decreased performance,
- dizziness,
- fainting states.
A blood test for anemia shows a decrease in the number of red blood cells and a decrease in hemoglobin content.
Thickening and thinning of blood
Blood thickening is characterized by a decrease in the content of water and some electrolytes in the peripheral blood. As a result, blood viscosity increases, rheological properties change, and the number of cells per unit volume increases relatively. Blood thickening develops when a large amount of fluid is lost. The reasons can be completely different:
- severe forms of dysentery;
- salmonellosis;
- poisoning with toxic substances;
- iatrogenic pathology.
Blood thinning (hydremia) is an increase in the amount of water in a person’s peripheral blood. It is observed quite rarely in patients with:
- kidney diseases;
- hypervolemia;
- when replacing BCC with plasma and blood substitutes after blood loss;
- in some cases of resuscitation and intensive care, if doctors administer large amounts of fluid intravenously for the purpose of detoxification.
Disseminated intravascular coagulation syndrome
DIC syndrome is characterized by widespread formation of small blood clots in the microvasculature of the entire body. Together with blood incoagulability, it leads to multiple massive hemorrhages. The disease requires early diagnosis and urgent treatment. It is based on discoordination of the functions of the coagulation and anticoagulation systems of the blood responsible for hemostasis.
Possible causes of DIC syndrome :
- infections (fungal infection; meningococcal sepsis, rickettsiosis);
- severe viremia (hemorrhagic fever);
- neonatal or intrauterine infections;
- gynecological diseases (placental abruption, amniotic fluid embolism);
- liver disease (cirrhosis);
- malignant tumors;
- injuries;
- fever;
- surgical interventions with artificial circulation;
- intravascular hemolysis;
- severe shock;
- snake bites.
Numerous blood clots in the microvasculature in disseminated intravascular coagulation syndrome lead to impaired tissue perfusion with the accumulation of lactic acid in them and the development of ischemia, as well as the formation of microinfarctions in the body organs.
Shock is a clinical condition that is associated with a decrease in effective cardiac output and impaired autoregulation of the microcirculatory system. Characterized by a decrease in blood supply to tissues, which leads to destructive changes in internal organs. The following types of shock are distinguished:
- hypovolemic;
- neurogenic;
- septic;
- cardiogenic;
- anaphylactic.
Local circulatory disorders
Local circulatory disorders may be as follows:
- arterial plethora;
- venous congestion;
- thrombosis;
- embolism;
- ischemia;
- heart attack;
- bleeding;
- blood stasis.
Local arterial plethora (arterial hyperemia) is an increase in the flow of arterial blood to an organ or tissue. Experts distinguish hypermia:
- physiological;
- pathological.
A striking example of physiological arterial hyperemia can be a blush of shame on the face, pink-red areas of the skin at the site of its thermal or mechanical irritation.
Angioneurotic hyperemia is observed in vasomotor disorders and is characterized by an acceleration of blood flow not only in normally functioning, but also in opening reserve capillaries. The skin and mucous membranes become red, slightly swollen, and feel warm or hot to the touch. Usually this hyperemia passes quickly, leaving no marks on the body. Collateral hyperemia occurs when the main artery is closed by an atherosclerotic plaque. The inflowing blood rushes through the collaterals, which expand. The rate of closure of the great vessel and the level of blood pressure are of great importance in the development of collateral arterial hyperemia.
Postanemic hyperemia develops in cases of fluid accumulation in the cavities, causing ischemia. The vessels of previously bloodless tissue expand sharply and fill with blood. The danger of arterial hyperemia is that overcrowded vessels can rupture and lead to bleeding and hemorrhage. Brain anemia may occur.
Vacate hyperemia develops due to a decrease in barometric pressure. An example of such plethora is skin hyperemia under the influence of medical cups. Inflammatory hyperemia is one of the important clinical signs of any inflammation.
Local venous congestion
Venous hyperemia develops when the outflow of venous blood from an organ or part of the body is disrupted. Experts distinguish between hypermia:
- obstructive venous;
- compression venous hyperemia;
- collateral venous hyperemia.
Blood stasis is a slowdown, up to a complete stop, of blood flow in the vessels of the microvasculature in the capillaries. Blood stasis may be preceded by:
- venous congestion (stasis);
- ischemia.
Blood stasis is characterized by stopping blood in capillaries and venules with expansion of the lumen and gluing of red blood cells into homogeneous columns (this distinguishes stasis from venous hyperemia). Hemolysis and blood clotting do not occur.
Stasis is observed in the following diseases:
- angioedema crises (hypertension, atherosclerosis);
- acute forms of inflammation;
- viral diseases (flu, measles).
The cerebral cortex is sensitive to circulatory disorders and hypoxia Stasis can lead to microinfarction . Extensive stasis in areas of inflammation carry with them the danger of tissue necrosis, which can radically change the course of the inflammatory process.
Bleeding
Bleeding is the release of blood from the lumen of a vessel or the cavity of the heart. If blood is shed into the environment, then we talk about external bleeding, if in the cavity of the body - about internal bleeding. Examples of external bleeding may include:
- hemoptysis;
- nosebleeds;
- vomiting blood;
- discharge of blood in feces.
With internal bleeding, blood can accumulate in the pericardial cavity, pleura, and abdominal cavity. Hemorrhage is a special type of bleeding. The causes of bleeding (hemorrhage) can be rupture, corrosion and increased permeability of the vessel wall. Hemorrhages are distinguished:
- point;
- bruise;
- hematoma;
- hemorrhagic infiltration.
Thrombosis is intravital blood clotting in the lumen of a vessel, in the cavities of the heart, or loss of dense masses from the blood. The resulting blood clot is called a thrombus. In addition to the coagulation system, there is a system that ensures the regulation of hemostasis: the liquid state of blood in the vascular bed under normal conditions. Based on this, thrombosis is a manifestation of dysregulation of the hemostatic system.
Factors influencing thrombus formation :
- damage to the vascular endothelium;
- changes in blood flow;
- changes in the physical and chemical properties of blood.
The causes of thrombosis can be:
- infections;
- malignant tumors;
- postoperative period;
- diseases of the cardiovascular system.
The location of the thrombosis determines subsequent treatment; thrombosis exists:
- arterial;
- cordial;
- venous (thrombophlebitis, phlebothrombosis).
Thrombosis does not always have certain manifestations. Symptoms occur if the clot grows in size and rises above the calf (this can cause swelling and pain in the leg).
Facial hyperemia
Facial hyperemia can occur as a result of a complex of vascular problems. A similar situation occurs with high blood flow speed and increased pressure. In addition, a small difference in the oxygen content between arterial and venous blood forces the heart and lungs to work harder, which provokes redness.
After a walk in the frosty air, hyperemia also occurs. It is caused by a sharp narrowing of the thin capillaries of the facial skin in response to low temperatures, which is replaced by a sharp increase in blood flow. This is how the body understands that there are areas of the body that are not protected by clothing, which need to be ensured vitality by being warmed by the bloodstream.
But there is also other redness caused by an allergic reaction to frost. This is the body's pathological response to cold. Such redness does not go away for a long time, even after returning to a warm room. This reaction indicates a decrease in immunity and the body’s inability to protect itself from adverse external factors.
Allergic facial hyperemia can be distinguished from physiological hyperemia by several signs. For allergies:
- redness occurs on all open areas of the body;
- hyperemia may take the form of urticaria;
- skin itching appears;
- the mucous membrane swells;
- there is a flow from the nose or tear duct;
- headache appears.
The temperature rarely rises during an allergic reaction.
Causes of hyperemia of the conjunctiva of the eye
Often redness of the eye
- This is a sign of conjunctivitis (inflammation of the conjunctiva). But it is important to remember that hyperemia can be caused by other reasons, and can also be a symptom of complex pathologies that lead to complete or partial blindness. Therefore, it is worth entrusting the diagnosis to experienced ophthalmologists.
The main causes of conjunctival hyperemia:
- All kinds of diseases of the organs of vision - barley, blepharitis, iritis, chalazion of the eyelid and others
- Allergy
- Mechanical damage and injury
- Diseases of the heart and vascular system
- Diabetes mellitus and other endocrine diseases
- Pathologies of cerebral vessels
- External factors - chronic fatigue, stress, increased visual stress, lack of sleep, radioactive radiation, etc.