Inguinal candidiasis is more often diagnosed in men than in women. The pathology belongs to the category of candidiasis of large folds and is characterized by severe symptoms, causing the patient discomfort and many unpleasant symptoms. The main cause of fungal disease is a decrease in the body’s protective functions under the influence of negative internal and external factors. Treatment of inguinal candidiasis should be carried out under the strict supervision of a physician. An important point is to identify the root cause that provoked the spread of fungal infection. Without its elimination, the risk of the disease progressing to the chronic stage, which is manifested by periodic relapses, increases. Medical specialists quickly diagnose the pathology and prescribe the most effective treatment, taking into account the individual characteristics of the patient’s body. Our doctors pay enough attention to each client to achieve the most positive therapeutic results and prevent complications.
Symptomatic picture of mycosis
Candidiasis of the inguinal folds is caused by specific fungi, which are opportunistic microorganisms that live on the skin and mucous membranes of any healthy person. The immune system, functioning without failures, suppresses the active activity of pathogenic microflora, so they remain in a latent state in the human body. However, under the influence of pathological exogenous and endogenous factors, the immune system is weakened and ceases to fully perform its functions. This contributes to the activation of the infection and its unhindered reproduction.
The active activity of a fungal pathogen on the skin in the groin area is manifested by the following pathological symptoms:
- Formation of spots in the groin. The lesions have clear boundaries and differ in color from healthy areas. The shade of the spots ranges from light pink to deep red.
- Peeling of the skin. In places where a fungal infection is localized, the skin becomes covered with a white coating and peels off. Peeling may spread to the perianal and pubic areas, as well as to the folds of skin between the groin and thigh.
- Uncomfortable sensations. In the groin area, the patient is bothered by severe, sometimes unbearable itching, which can cover the femoral part of the lower limb.
- Irritation. Swelling, redness, and irritation form at the site of active fungal activity.
On the skin of the groin area affected by the fungus, round, deformed areas are visualized, which differ from healthy skin in shade and the presence of peeling on the surface. Thanks to such visual signs, the doctor can make a preliminary diagnosis, which will be confirmed by the results of a comprehensive diagnostic examination.
List of sources
- Sergeev A. Yu., Sergeev Yu. V. Fungal infections (a guide for doctors). M., 2003. 185–193.
- Leshchenko V. M. Fungal skin diseases. In the book: Skin and venereal diseases (a guide for doctors). Ed. Yu. K. Skripkina, V. N. Mordovtseva. M., 1999. T. 1. P. 257–311.
- Sergeev V.Yu., Sergeev A.Yu. Dermatophytes: new in the diagnosis, therapy and prevention of the most common human mycoses. Consilium medicum. – Dermatology. – 2008. – No. 1. – P. 30–35.
- Haldin A.A., Sergeev V.Yu., Izyumova I.M. Modern ideas about inguinal dermatophytosis: etiology, epidemiology, clinical picture and effective therapy. Ross.zhur. leather and veins Bol. – 2005. – No. 5. – S. 43–48.
Athlete's inguinal
The disease is caused by fungi of the genus Epidermophyton floccosum. The infection is transmitted through household contact and most often affects men. Factors that provoke the development of the disease include:
- wearing tight, constricting clothing that disrupts natural air exchange in the groin area;
- profuse sweating;
- increased environmental humidity;
- frequent injury to the skin in the groin;
- inactive lifestyle;
- excess weight.
In the initial stages of development, the infection is localized in the skin folds of the genital area, but as it progresses it spreads to the upper part of the inner thigh, affecting both limbs. Usually the fungus does not affect the skin of the scrotum.
The rash has a scaly, pinkish border. Inguinal athlete's foot is often accompanied by itching and pain symptoms. Lack of timely treatment leads to an increase in lesions and the spread of infection to healthy tissue.
To prevent the development of inguinal athlete's foot, it is advisable to follow simple rules of prevention:
- wear comfortable underwear made from natural fabric;
- observe the rules of personal hygiene, especially in saunas and swimming pools;
- use personal hygiene items and do not give them to any strangers;
- normalize body weight;
- add moderate physical activity;
- If you have characteristic symptoms of a fungal infection, do not self-medicate, but make an appointment with a dermatologist as soon as possible.
Consequences and complications
When athlete's foot complications are considered:
- Transition from one form to another.
- Onychomycosis.
- The addition of a bacterial infection is secondary pyoderma , lymphangitis , lymphadenitis and recurrent erysipelas, resistant to antibiotic treatment. Against the background of such lesions, thrombophlebitis , lymphostasis and elephantiasis occur .
- Allergization of the body: urticaria , bronchial asthma , allergic rhinitis , the occurrence of mycids . These are secondary allergic rashes due to mycoses.
For inguinal athlete's foot:
- Mycotic eczema . It occurs in a chronic form, manifested by lichenification of the skin (thickening), which occurs from scratching. The process resembles neurodermatitis.
- Allergic dermatitis.
- Impetiginization is the development of impetigo as a complication of mycosis. Impetigo is a strepto-staphylococcal skin lesion.
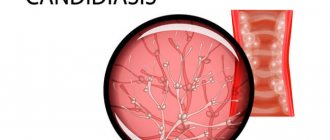
Candidiasis in the groin area
The causative agent of candidiasis in the groin area is a yeast-like fungus of the genus Candida, which belongs to the opportunistic microflora and lives on the skin and mucous membranes of every healthy person. With natural balance and proper functioning of the immune system, the infection is in a latent state and does not provoke the development of pathological processes. But as soon as the immune defense fails, the fungi are activated and begin to multiply unhindered, causing the formation of deformable surface changes, accompanied by pathological symptoms.
Common causes of candidiasis in the groin area are:
- obesity, accompanied by the appearance of large folds on the skin;
- endocrine, hormonal disorders;
- failure to comply with personal hygiene rules;
- uncontrolled use of certain groups of medications;
- unbalanced diet, predominance in the diet of foods containing large amounts of carbohydrates and sugar;
- infection through close contact with a carrier.
At the initial stage of development of inguinal candidiasis, the affected skin changes color to a darker one. Then the skin becomes covered with a small blistering rash. The spots have a clear outline. The areas where the blistering rash has formed begin to crack over time, forming erosions and ulcers. Injury is accompanied by unbearable itching and pain.
Fungi of the genus Candida produce a specific enzyme that accumulates in places of infection in the form of a thick, curdled mass. A whitish coating is a characteristic symptom of candidiasis and allows the dermatologist to differentiate the pathology. Treatment of candidiasis of the groin area must be carried out immediately, otherwise the disease will become chronic, accompanied by periodic exacerbations.
Diagnostic measures
With such problems, the patient should seek professional medical help from a mycologist. During the appointment, the doctor will conduct tests such as:
- Dermoscopic examination
- Scanning a surface using a special type of luminescent equipment.
- Skin pH assessment.
- Scraping test.
- Sowing to check the nutrient medium.
In addition, the expert can refer the patient for a consultation with colleagues in the orthopedic, phlebological, endocrinological and other departments.
Inguinal rubrophytosis
The infectious disease is caused by fungi of the genus Trichophyton rubrum. This is a fairly common type of mycosis, which is diagnosed in a third of the population. You can become infected with inguinal rubrophytosis from a carrier through bodily contact, clothing, and household items.
Common reasons for increased growth of fungal colonies are:
- excessive sweating;
- failure to comply with personal hygiene rules;
- regularly wearing tight, tight clothing, including underwear;
- hormonal and endocrine disorders;
- increased environmental humidity;
- uncontrolled use of certain groups of medications;
- obesity.
Inguinal rubrophytosis manifests itself in 2 forms:
- Erythematosquamous. It manifests itself in the formation of red spots on the skin that have an irregular shape with an intermittent border. On the surface of the affected skin, compactions and a blistering rash with liquid inside are noticeable.
- Follicular nodular. It develops when treatment of the erythematosquamous form is untimely. The follicular nodular form is characterized by the spread of infection to healthy areas of the body: buttocks, feet, forearm, hands, legs.
Inguinal rubrophytosis brings unbearable discomfort to the patient, causing severe itching, pain while walking and when in contact with clothing. If there is no therapy, the spots rapidly increase in size, spreading to healthy areas.
In terms of external signs, inguinal rubromycosis is similar to such common dermatological diseases as:
- eczema;
- psoriasis;
- candidiasis;
- erythrasmus.
To differentiate rubrotrophy, the doctor gives a referral for a comprehensive diagnosis, the results of which will help prescribe the correct and most effective treatment.
Tests and diagnostics
- Microscopy of pathological material is used as a method of preliminary diagnosis.
- Isolation of a pathogen culture (growth of the pathogen in a culture) takes time.
- Polymerase chain reaction (PCR). It makes it possible to obtain results within 24 hours that are highly specific (90-98%). It is especially important for onychomycosis and atypical forms of dermatomycosis, since in the earliest stages it allows to prescribe rational therapy, reduce complications and the severity of lesions.
What treatment therapy should I use?
Before prescribing treatment for inguinal candidiasis, it is necessary to establish an accurate diagnosis and identify the pathogen. Therefore, after an initial examination and history taking, the doctor gives a referral for a comprehensive diagnostic examination, including the following procedures:
- microscopy;
- bacterial sowing;
- molecular biological analysis.
Treatment of candidiasis in the groin should be comprehensive and carried out under the strict supervision of a doctor. Self-medicating with such a disease is dangerous and fraught with serious complications.
The treatment plan includes the following activities:
- Identification and elimination of factors that provoke immunodeficiency.
- Prescription of antifungal and symptomatic therapy.
- General strengthening therapy.
To combat a fungal infection localized in the groin, local antifungal drugs are prescribed in the form of creams and ointments, which contain an antimycotic component. In the fight against fungi, drugs such as:
- "Nystatin";
- "Natamycin";
- "Clotrimazole".
If the disease is advanced and accompanied by serious complications, in addition to topical medications, antifungal medications are prescribed for oral administration in the form of capsules and tablets:
"Fluconazole";
"Itraconazole"
In the most advanced cases, the doctor will recommend intravenous or intramuscular administration of antimycotics. As soon as the condition improves, you can switch to tablets.
In case of correct treatment, the disease completely disappears within 7–10 days. To confirm complete recovery, repeat tests must be taken after completing the main course. If the fungal infection is completely eradicated, the laboratory test results will be negative.
In addition to drug treatment, it is important to follow preventive measures that enhance the therapeutic effect and reduce the risk of relapse to zero. Therefore, together with drug therapy, it is advisable to follow the following rules of prevention:
- strengthen immunity;
- lead a healthy, active lifestyle;
- get rid of bad habits;
- maintain personal hygiene;
- normalize weight;
- use products that control sweat in large folds.
If there is no treatment for inguinal candidiasis, the fungal infection will gradually spread throughout the body, causing health and life-threatening complications. Therefore, if you have suspicious symptoms, you must make an appointment with a dermatovenerologist, take all tests and be treated under the supervision of a specialist.
Procedures and operations
In advanced forms of onychomycosis and irreversible changes in the nail plate, the patient may be offered surgical removal of the nail plate, which is performed under local anesthesia. After surgery, an antibiotic and antifungal ointment is applied to the wound. The dressing is changed twice a day. The course of treatment with local antifungal agents continues until a healthy nail grows - this may take 6-9 months.
Laser removal of the nail plate is also used. The procedure is less painful and bloodless than conventional surgical nail removal, is characterized by rapid tissue restoration, and there is no deformation of the growing nail. If the nail plate is slightly affected, it is not completely removed using a laser. It is enough to destroy the mycelium and spores of the pathogen with laser exposure. With the help of a laser, this is possible because it penetrates 7-8 mm through the nail into the soft tissue. The course of treatment is 4-5 procedures, and after a month it is recommended to repeat the course of treatment.