How dangerous is the flu?
There is probably no person who does not suffer from ARVI. According to WHO, every person gets a cold from 2 to 4 times a year, school-age children - 4-5 times, preschoolers - 6 times a year, and babies in their first year of life - from 2 to 12 times. Among ARVI, the influenza virus is truly dangerous, which is why its prevention and treatment is given such great importance. Flu can lead to viral pneumonia and severe intoxication. It also leads to decreased immunity and exacerbation of chronic bacterial infections, bronchial asthma, cardiovascular diseases, and kidney diseases. All this, in turn, can lead to death. Therefore, patients with symptoms of severe intoxication, meningitis, acute respiratory and heart failure, high fever for more than 5 days, and pregnant women must be hospitalized in the infectious diseases department.
The end of the 20th – the beginning of the 21st centuries: by surprise
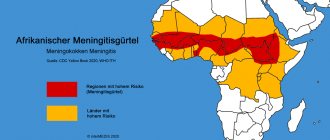
No matter how well GISRS works, unfortunately, sometimes the virus manages to break through contrary to scientists’ predictions. Humanity was taken by surprise by the outbreaks of the so-called “bird” and “swine” flu at the beginning of the 21st century. These strains, a recombination of human and animal viruses (birds and pigs), turned out to be completely new to human immunity and were not included in the WHO forecast.
In such rare cases, when unexpected mutations of influenza occur, vaccines are created on an emergency basis to prevent the infection from spreading widely, and are used separately, or the new strain is included in the seasonal vaccine.
In general, over the almost 70 years of existence of GISRS, the system has proven itself to be excellent and has shown the correctness of the adopted strategy for the prevention of influenza by adapting vaccine production to virus mutations.
To summarize the historical excursion, I would like to note the contribution of vaccination to protecting the population from influenza. According to the State report “On the state of sanitary and epidemiological well-being of the population in the Russian Federation in 2021”, the effectiveness of vaccination is clearly confirmed by the dynamics of influenza incidence, the level of which has decreased by almost 140 times since 1997 (from 5173.8 per 100 thousand population (with vaccination coverage of 4.9 million people in 1996) to 37.3 in 2021 (with vaccination coverage of 70.8 million people in 2021).
The graph clearly shows a decrease in incidence in direct proportion to the number of people vaccinated:
How does the flu vaccine work?
There are several types of vaccines:
- vaccines containing live attenuated strains of viruses;
- vaccines containing dead viruses or fragments of viruses and antibodies to them.
Modern vaccines are tri- and quadrivalent, i.e. containing three or four types of viruses predicted by the World Health Organization for this particular year for a particular region. After vaccination, the body’s immune system begins to react, producing special antibodies that recognize and kill the virus when it enters the body. This process usually takes about a month, so vaccination takes place 1 - 1.5 months before the expected epidemic.
Unusual solution
If, to protect against most vaccine-preventable infections (measles, diphtheria, polio, etc.), the same vaccine composition has been used for decades, and 1 course, and sometimes even one injection of the drug, is enough to develop full immunity in a person life, then in a situation with a constantly mutating flu, scientists had to look for a different way to make an effective vaccine.
The solution found is striking in its complexity and scale. Every year, for the flu season, we need to produce vaccines with a new composition! And to reduce the risk of errors, it is proposed to include in the vaccine not one strain, but a set (usually of three) of the most probable strains. A system was needed to monitor and forecast the circulation of the influenza virus in all countries on all continents.
In 1952, the WHO created the Global Influenza Surveillance and Response System (GISRS). Its work is to collect information about viruses from all over the world. The resulting data is entered into a single database and a special The commission makes a decision on the forecast of which influenza strains will actively circulate and can cause an epidemic in the coming season.A lot of factors are taken into account, including the aggressiveness of newly identified viruses, the similarity with previously circulating strains, and the presence of immunity in the population.
It was with the participation of this system that the possibility of effective influenza vaccine prevention became possible.
How does this happen
Every year in February, a WHO meeting takes place, at which, according to GISRS, recommendations are issued to manufacturers about the strains of influenza virus that should be included in the vaccine. At the end of February and beginning of March, the cultivation of strains begins. Almost all vaccine manufacturers use an old, proven technology for this: the influenza virus multiplies in chicken embryos. If the recommended strain is well cultivated, it is taken into production. Sometimes, due to poor growth of a particular type of virus, a well-growing analogue with a similar antigenic structure is urgently selected.
After this, the vaccine manufacturing process is activated at full capacity. Typically, it takes about 4 months to produce three (or four) strains, neutralize (in different ways for different types of vaccines), purification, quality control, mixing components and packaging. We recommend watching the vaccine production process in the video of our partners Sanofi Pasteur:
Next comes certification and logistics taking into account the “cold chain”. If everything goes smoothly, the first batches of the vaccine will arrive at medical organizations at the end of August. Typically, the main volumes become available in September-October, which makes it possible to vaccinate the population before the seasonal rise in incidence begins.
Who is recommended for the flu vaccine?
- children over 6 months old, especially those attending nurseries, kindergartens, schools;
- medical workers;
- employees of children's educational institutions (teachers, educators, heads of clubs, sections);
- elderly people over 60 years of age;
- chronic patients with diseases of the respiratory and cardiovascular systems;
- patients with reduced immunity.
Vaccination is mandatory for all these population groups. The vaccine will prevent you from getting sick or get through the disease more easily, and will prevent complications from developing.
Why doesn't the vaccine protect 100%?
Previously, we have already examined cases when vaccinated people can also get sick. Once again, we note that any vaccines do not provide a 100% guarantee. In the instructions for the drugs you will see efficiency indicators that are always above 80%, close to 95-99%.
Efficacy is influenced by the initial characteristics of the vaccine and the immune status of the individual. In the case of influenza, we described the additional risks and complexities associated with yearly forecasting and updating of strains.
Scientists have extensive experience in combating this elusive enemy; more than 2,000 serotypes of influenza viruses are known in the world. However, the risk of a completely new mutation always exists, and scientists cannot yet control this. Just like they cannot create a vaccine that would protect against influenza for life and 100%.
Whether you should get vaccinated when you are unsure of the Global Influenza Surveillance System forecasts is up to you. Perhaps the numbers will help you make a difficult choice: in Russia, among those sick with influenza A, 91.8% were unvaccinated, and among those who died, 100%.
What complications can occur after vaccinations?
- allergic reaction, if you are allergic to chicken protein, you should inform your doctor;
- the occurrence of a local reaction at the site of vaccine administration;
- after vaccination, symptoms of acute respiratory viral infection or flu may appear, but they are usually more easily tolerated than if an infection had occurred with an unattenuated virus.
From September to October 2021, you can get vaccinated under the compulsory medical insurance policy at your place of attachment or go to a private clinic. The average cost of vaccination is about 500 rubles.
There are contraindications. Specialist consultation is required.
Flu vaccines. Pros and cons, which vaccine to choose?
Vaccination in itself is a great benefit, as it has helped protect humanity from destruction or a significant reduction in the population of the Earth. Let opponents of universal vaccination sing their mantras about the dangers of vaccines, but this procedure very effectively helps to build immunity against bacterial or viral agents with a stable cell membrane structure, such as smallpox, measles, polio and many others.
Contraindications for vaccination.
Intolerance to chicken protein and/or preservatives used in vaccine production; children under 6 months of age; acute illnesses or exacerbations of chronic diseases until complete recovery, it is usually recommended to wait 3-4 weeks after the acute process has subsided and then allow flu vaccination; a history of other post-vaccination complications in response to previous vaccinations.
Complications of vaccination.
Complications of vaccination can be divided into two groups: local - which are found at the site of vaccine administration (swelling, redness, soreness at the injection site; for nasal vaccines (administered through the nose) - runny nose, cough, sore throat)
systemic - represent the response of the whole body to the introduction of the vaccine (headache, allergic reactions, fever, chills, feeling of weakness, otitis media, meningitis, myositis and other complications)
Flu vaccination timing.
The standard time frame for flu vaccination is October-November. It is believed that in the time remaining before the outbreak of the epidemic, a stable immunity will be formed that will protect the vaccinated person from infection. It takes 10-15 days from the moment the vaccine enters the body to develop sufficient immunity against influenza. Vaccination before October is not advisable, as it leads to a drop in the level of antibodies against influenza towards the end of the epidemic and an increased risk of infection.
Methods of administering vaccines
Nasal - by introducing a special vaccine into the nose, which leads to greater development of local immunity, a weaker protective reaction is likely to develop and is currently rarely used
Injection is the standard and most common route for administering the flu vaccine; the vaccine is administered subcutaneously or intramuscularly. Children who have not received a flu vaccine and who have not previously had the flu, the vaccine is administered twice with an interval of 1 month in the amount of half the adult dose.
Types of Vaccines
For specific prevention against influenza, vaccines are used, divided into two large groups: -
live vaccines
(containing weakened and non-infectious viruses) -
inactivated
(do not contain live viruses)
Inactivated vaccines, in turn, are divided into three groups: - whole cell
- contain whole cells of the influenza virus -
split or split vaccines
- contain split cells of the influenza virus containing both surface and internal protein molecules and antigens, due to the high degree of purification they do not contain viral lipids and proteins of the chicken embryo (
Grippol , vaccine Fluarix Begrivak vaccine , Vaxigrip ) - subunit vaccines
- contain only surface viral proteins (hemagglutinin and neuraminidase) (
Grippol plus , Influvac Agrippal vaccine ).
Whole cell and live vaccines
are the most reactogenic, especially in young children, and can cause post-vaccination reactions and complications. Accordingly, the scope of application of such vaccines is very narrow, although it is worth noting that these types of vaccines have a good ability to form immunity against influenza.
Split and subunit vaccines
- do not have such a frequency of complications after administration and at the same time form immunity at a fairly decent level, therefore they are currently a standard in use for the prevention of influenza.
Which of these vaccines is the best?
Most likely, there is a golden mean, in the form of a split vaccine, which has a minimum of side effects, but has the ability to well form immunity to the influenza virus.
Representatives of this type of vaccine are the following vaccines: Vaxigrip , Grippol , Fluarix , Begrivak
The best imported
Imported vaccines on the Russian market in the 2020–2021 season are represented by two drugs: the French Vaxigripp and the Dutch Influvac. According to RBC, they are expected in pharmacies in mid-October - early November.
Vaxigrip
Among the characteristics:
- Manufacturer: SANOFI PASTEUR, SA, France.
- Quadrivalent inactivated influenza split vaccine.
- Contains 15 mcg of influenza virus antigens of each strain, which is recommended by WHO.
- Does not contain adjuvants or preservatives.
- The minimum age for vaccination is 6 months.
Influvac
Among the characteristics:
- Manufacturer: Abbott, Netherlands.
- Quadrivalent subunit inactivated.
- Contains 15 mcg of influenza virus antigens of each strain, which is recommended by WHO.
- Does not contain adjuvants or preservatives.
- The minimum age for vaccination is 6 months.
Can the flu be cured?
Currently, there are two groups of anti-influenza drugs on the pharmaceutical market:
- Adamantane preparations (amantadine, remantadine). This is an old group of drugs to which the virus has developed resistance. Currently, their use is not recommended.
- Neuraminidase inhibitors (oseltamivir, zanamivir). Resistance to this group of drugs in influenza viruses is growing rapidly. In addition, these medications have a number of significant side effects.
There is also a fairly effective, but expensive and complex way to treat seriously ill patients using donor plasma.
All of the above brings us back to the fact that vaccination today is more effective and safer than medications used to treat influenza.
How does the flu shot work?
JSC Family Doctor - Flu Vaccination Vaccination against the flu allows you to prepare for an epidemic by making your body less susceptible to the virus. The influenza vaccine contains influenza virus proteins. The immune system reacts to their entry into the body, beginning to produce specific antibodies to this virus. And when a person who has been vaccinated against influenza encounters a source of influenza infection, the influenza virus encounters a defense already configured in the body against it.
Who can't?
All influenza vaccines have absolute and temporary contraindications, which are indicated in the instructions for the drugs.
Vaccination is not carried out:
- If you are hypersensitive to chicken protein and have a severe allergic reaction to the vaccine. The key here is heavy.
- For an acute illness, a cold, which occurs with a temperature above 38°C.
- If the doctor has reason that the body’s immune response will not be formed. For example, if the patient is taking a therapy that suppresses the immune response.
- The live vaccine is not used in children under 3 years of age, pregnant women and people with impaired immunity.
Remember: The administered vaccine does not cause illness and does not contribute to a more severe course of influenza and other acute respiratory viral infections.
Where does vaccination take place?
For the convenience of residents, this year vaccination will take place at children's and adult clinics in separate vaccination rooms in two shifts. In addition, 54 mobile points have been organized. They operate at 36 metro stations, two stations of the Moscow Central Circle and two railway platforms, as well as four.
Since September 5, 10 additional mobile vaccination points have been placed at some metro stations, as well as near the Kryukovo railway station. Two ambulances will be on duty at each of these points. Mobile vaccination teams will also work in institutions and organizations, in all schools, colleges and universities.
Reaction to vaccination
Local reactions to vaccination usually occur in the area where the vaccine was administered: redness, slight swelling, heaviness at the injection site. Adverse symptoms appear 1-2 days after vaccination and disappear without a trace after 2-3 days.
General reactions are a slight (up to 38 °C) increase in temperature, loss of appetite, malaise. Do not be alarmed: this means that the vaccine “works.”
But if the temperature rises to 38.5 °C and above, there is a feeling of weakness and weakness, severe swelling, pain, suppuration at the injection site, then these are deviations from the norm. In such a case, you should definitely consult a doctor.
What is the flu, and why is it dangerous?
Influenza is an acute respiratory viral infection characterized by:
- sudden and rapid onset;
- increase in body temperature to high numbers;
- chills;
- severe weakness;
- severe aches in muscles and joints;
- headache;
- photophobia, redness of the eyes.
A runny nose and sore throat with the flu are usually mild. Often patients are bothered by a dry, painful cough, which can persist for a long time.
The infection is transmitted by airborne droplets. Typically, the incubation period lasts several days. In this case, a person becomes contagious even before clinical symptoms.
Often, influenza cannot be distinguished from other viral infections. In order to do this, there is a special analysis. Unlike ARVI, influenza has more severe symptoms, a higher incidence of complications and a protracted course. Complications of influenza include: otitis media, bronchitis, laryngitis, pneumonia. In addition, the influenza virus causes specific complications, affecting the nervous system and skeletal muscles.
Vaccine Grippol Plus
It is produced by FC Petrovax LLC and is an improved analogue of the Grippol vaccine, which has been used in domestic immunoprophylaxis since 1996. Grippol Plus is a preservative-free vaccine produced in an individual syringe dose in accordance with the GMP standard.
The vaccine contains purified antigens of current influenza virus strains recommended by WHO for the current epidemic season.
Can be used by children starting from 6 months of age.
Can you get the flu from a vaccine?
Vaccination is carried out with modern, proven drugs that do not contain a live virus and cannot lead to influenza.