Donovanosis (granuloma inguinale, granuloma venereum) is a classic, chronic sexually transmitted disease. It is caused by the bacterium Klebsiella granulomatis (formerly called Calymmatobacterium granulomatis). It is found endemically in underdeveloped countries in tropical and subtropical regions. In the United States, blacks are seven times more likely to be infected than whites. People living in poor socio-economic conditions are most often affected.
Klebsiella granulomatis is a gram-negative bacterium belonging to the family Enterobacteriaceae. Penetrating through the skin, it causes an inflammatory reaction that can lead to the destruction of infected tissue. As part of the inflammatory focus, bacteria are localized inside tissue macrophage cells (Donovan bodies). Donovan Taurus is named after Charles Donovan. He was the first to discover them.
The bacteria are an integral part of the physiological intestinal flora and can very easily be transmitted to the genital area through autoinoculation or sexual intercourse.
The first known name for this condition was "serpiginous ulcer", dating back to 1882. The correct clinical term used today for donovanosis is granuloma inguinale. Granuloma is a type of inflammatory reaction that occurs as a result of injury or infection.
Incubation and symptoms of donovanosis
The content of the article
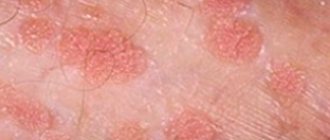
The incubation period - the time from infection to the appearance of the first symptoms - is long and lasts from 10 to 40 days. It manifests itself by the appearance of small painless nodules in the area of the external genitalia (vulva, penis).
Subsequently, the skin over the change ruptures and ulceration of the granulomatous bottom occurs. It spreads by autoinoculation and affects the perineal area, anal area and groin. The ulcers are usually painless and relatively clean. Inguinal lymphadenopathy, an enlargement of the inguinal lymph nodes, is also often present.
The first stage of syphilis is easy to miss!
Syphilis is caused by a microbe that has a spiral shape and is called a pale spirochete. Getting even on a slightly damaged mucous membrane or skin, the pale spirochete penetrates into deeper tissues and then into the blood. At the place where the pale spirochete has penetrated the tissue, at the end of the third week after infection, an ulcer with dense edges and a bottom appears - a chancre.
This ulcer gradually increases over the course of 2-3 weeks, then its growth stops, it begins to shrink and heals, leaving behind a slight compaction. After the appearance of hard chancre, the nearest lymph nodes enlarge.
Many people do not even suspect that they have contracted syphilis, so they begin to treat the wound with antibiotics. As a result, it is delayed, but the infection remains in the body and undermines it from the inside.
Treatment of donovanosis
Antibiotic treatment is very effective. This is why the incidence of this classic sexually transmitted disease is very low in developed countries (about a hundred cases per year are reported in the United States), in contrast to underdeveloped regions where the availability of antibiotics is limited.
Treatment is usually with the following antibiotics:
- sulfamethoxazole trimethoprim (Sinersul) orally for 14 days;
- doxycycline (vibramycin, chiramycin) per os for 14 days;
- azithromycin (Sumamed) orally for 7 days;
Although improvements in the condition appear after the first week of taking antibiotics, treatment should be completed completely to reduce the number of relapses.
Effective preventive measures include:
- avoiding sexual contact with people at risk, especially in endemic areas;
- preventive testing for sexually transmitted diseases.
Diagnostics
Several basic methods are used to detect syphilis:
- Detection of treponema pallidum using a microscope in a scraping taken from a chancre.
- The serological method (Wassermann reaction) - when specific proteins that are produced by the immune system in response to the appearance of treponemes in the body are determined, is not effective for primary syphilis.
- The microprecipitation reaction is a rapid diagnosis, also based on the body’s production of antibodies.
- Specific tests RIF, RIT, RPGA, etc. – difficult to set up, time-consuming and expensive. Used to identify latent syphilis, in complex atypical cases, in differential diagnosis and for the diagnosis of late syphilis.
If treponema is detected immediately using microscopy, additional studies are not required to prove infection. Upon detection of treponema, treatment is prescribed immediately.
Sometimes it is necessary to carry out a whole range of diagnostic measures to establish an accurate diagnosis, so it is impossible to diagnose the disease yourself; you need to consult a doctor.
Ulcus molle (chancroid, soft chancroid)
Ulcus molle is a classic sexually transmitted disease caused by the bacterium Haemophilus ducreyi. Usually found in the tropics - Africa, Asia, Central and South America. The disease occurs 20 times more often in men than in women. Chancroid is particularly important in the context of HIV (AIDS), given the high incidence of both diseases in Africa.
Haemophilus ducreyi is a rod-shaped gram-negative bacterium. In cell culture it takes the form of multirow chains.
Syphilis is treated and not treated
Systematic treatment of syphilis currently gives good results, especially when it is started soon after the first signs of the disease appear. Timely and vigorous treatment of syphilis in the mother during pregnancy is the best way to prevent syphilis in the child. But advanced stages of the disease are incurable.
Treatment of syphilis, as well as gonorrhea, should only be carried out by a doctor. It must be remembered that a cure can be achieved only on the condition that the patient accurately follows every doctor’s prescription and carefully carries out the entire course of treatment.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
Clinical picture of chancroid
Incubation (time from infection to onset of symptoms) is usually 3-5 days. A small spot appears at the site of penetration. The next day a pustule (purulent vesicle) forms on it; after a few hours it ruptures, and small ulcers with a bottom filled with pus are formed. The sores are painful to the touch, and the surrounding skin is often erythematous and edematous (red and swollen). New ulcers around the primary ulcer may result from manual transmission of infection (autoinoculation). The so-called kissing ulcers located opposite each other. In more than 50% of patients, regional lymphadenopathy (enlarged lymph nodes) occurs within 7 days.
Areas prone to ulceration
For men:
- the inner part of the foreskin;
- glans penis;
- external urethral opening;
- coronary sulcus;
- bridle.
For women:
- labia majora;
- entrance to the vagina.
Patients who simultaneously suffer from scabies or genital herpes may experience 50 to 60 ulcers at the same time.
Prevention
Since the mode of transmission of the disease is mainly sexual, preventive measures consist of maintaining fidelity to sexual partners - this is the most effective prevention of sexually transmitted diseases. When having sexual contact with an unverified person, you should always use a condom.
Barrier contraception (condom) provides almost 100% protection against syphilis infection.
In any case, after accidental contact, it is necessary to independently treat the genital area with antiseptic agents: miramistine or chlorhexidine.
If an unplanned contact occurs without protective equipment, or the integrity of the condom is damaged in the process, doctors recommend visiting a prenatal clinic as soon as possible and receiving a preventive injection, which will almost 100% prevent the development of syphilis.
Treatment of chancroid
When prescribing therapy, it should be taken into account that the sensitivity of Haemophilus ducreyi to antibiotics varies in different geographical regions.
Ceftriaxone is considered the most effective. It is administered once intramuscularly.
Alternative drugs are azithromycin per os, trimethoprim/sulfamethoxazole per os, erythromycin per os for 7 days.
Hospitalization is recommended for patients, as rest prevents the occurrence of lymphadenopathy.
Sexual partners should be treated simultaneously with one of the mentioned therapeutic methods.
Lymphogranuloma venereum - symptoms
Lymphogranuloma venereum occurs in men five times more often than in women. The disease is characterized by a relatively long incubation period (the time from infection to the appearance of the first symptoms), amounting to two weeks or more.
A primary, often very small, ulcerative lesion appears on the external genitalia. Accompanied by regional enlargement of lymph nodes. Enlarged lymph nodes in the groin area often merge and can form fistulas (a fistula is an unnatural narrow channel connecting a pathological lesion or organ to the surface of the skin or mucous membranes, or two or more organs together).
Prices for services
Initial appointment with a urologist FOR MEN + ultrasound of the prostate gland (assessment of complaints, medical history, if necessary, rectal digital examination, ultrasound of the prostate gland in men)
Primary appointment – visiting a doctor of a specific specialty for the first time. Includes a conversation with the patient, an initial examination, anamnesis, if necessary, a digital rectal examination, and an ultrasound of the prostate gland. The price is valid from 02/01/2021 The price is not valid for appointments at the branches of Bolshevikov Ave. and Prosveshcheniya Ave. Make an appointment
550 ₽
Repeated appointment with the urologist
Make an appointment
700 ₽
Lymphogranuloma venereum - complications
Late complications can occur several years after the initial lesion:
- Elephantiasis is a syndrome characterized by elastic, hard swelling of the legs (ivory) or external genitalia. This occurs with chronic stagnation of lymph due to inflammatory (filariasis, lymphogranuloma venereum) or non-inflammatory factors. It is important to treat the underlying disease; conservative (compression bandages, massage) and surgical (lymphatic drainage) treatment is also used.
- Genital strictures are cicatricial narrowings that occur as a result of injury or inflammation.
- “Identification reaction” on the skin is an allergic reaction to an inflammatory focus.
- Erythema multiforme is an increased change in the skin, usually the size of a smaller or larger coin. Color varies from light red to brownish red. The central part quickly recedes and becomes pale in color, while the edges of the change persist, retaining a reddish hue.
- Erythema nodosum - manifests itself as painful nodules on the legs. It is more common in young people, especially women. This is an allergic reaction to various microorganisms and medications. During treatment, it is important to eliminate the predisposing factor. The prognosis is very good.
Types of chancre
Chancre is an ulceration that occurs 3-90 (on average 21) days from the moment of infection with syphilis, more often in the area of penetration of the pathogen into the patient’s body.
First, a pink spot (inflammation) forms on the skin, then a dense nodule appears in this place, after 7-10 days it becomes necrotic and turns into an ulcer or erosion. If the resulting chancre is not accompanied by itching or pain, then it is called syphiloma. Syphiloma has a regular round or oval shape and clear boundaries that protrude above the skin. The edges are dense, roll-shaped. The bottom of the syphiloma is red, less often – meat-colored, maybe red-brown, and the chancre itself looks varnished, due to the characteristics of the wound.
The size of syphiloma varies from 5 to 30 mm, but there are ulcers of larger or smaller diameter. The main symptom of chancre is a cartilaginous compaction at the base of the ulcer, which can be felt upon palpation. When pressed, the chancre is painless. The skin around the ulcer is clean, without signs of inflammation.
Chancre is formed due to the penetration of Treponema pallidum (spirochete) into the body. For reproduction, the temperature of the human body is suitable for it and after entering the body it actively forms syphilomas. The chancre themselves can be of different types, shapes and sizes.
Classification
By quantity
Single - chancre in the form of a separate neoplasm, or multiple, which looks like several ulcerations.
By origin
Twin chancres occur during simultaneous infection - when the pathogen enters the patient’s body not in one, but in several “places”. That is, instead of one chancre, two or more can be found.
Chancres formed as a result of infection at different times. They appear one after another, in approximately the same place.
The so-called “kissing” chancre, which occurs on contacting surfaces.
Concomitant diseases can contribute to the formation of multiple syphilomas:
- scabies
- acne
- skin injuries
By depth of penetration into tissue
Syphilomas have different depths of tissue damage.
Ulcerative lesions affect the deep layers of the skin. They can pass through the dermis - right down to the subcutaneous tissue. I have a rough bottom covered with purulent plaque. Erosion is located closer to the surface. The bottom is smooth, shiny, and shaped like a saucer.
To size
In addition to standard sizes from 5 to 10 mm, there are giant and dwarf chancres.
Giant chancres are extremely rare and can reach up to 20 cm in diameter. They are localized mainly in areas of accumulation of fatty tissue: on the abdomen, thighs, and pubis. Syphilomas are called dwarf and are the size of a poppy seed - 1-2 mm; they can only be seen through a magnifying glass. They are rare.
By location
Chancre can be located on different parts of the body:
- genital syphilomas are located on the genitals
- extragenital - on any other parts of the body outside the genitals (Fig. 1)
- bipolar syphilomas occur simultaneously both on the genitals and outside the perineum.
Figure 1. Chancre on the index finger of the left hand and in the area of the inner corner of the left eye. Source: CC0 Public Domain
By shape
In addition to the classic round shape, chancre can have a different appearance.
Slit-shaped syphilomas look like cracks. They can form in the corners of the mouth, on the tongue, near the anus. They are rare. Located in the corners of the mouth, they can be perceived by the owner as non-dangerous “jams”.
Cortical chancre is not like ordinary syphilomas; it is not concave in shape and is covered with a crust. It usually forms on ulcers that are located in places where their contents dry out easily: the surface of the nose, face, corners of the mouth.
Diphtheritic chancre is covered with an ash-gray film, similar to diphtheria. Happens quite often. It can be localized in any area.
The burn chancre quickly increases in diameter, while its borders lose their regular shape and clear outline, and the bottom changes from smooth to red-grained (Fig. 2). Typically, primary syphilomas do not tend to grow. This is an exception.
Figure 2. Burn syphiloma. Source: CC0 Public DomainCaption
Erosive chancre includes many erosions; ulcers can merge. Formed exclusively on the mucous membranes of the genitals.
Chancroid herpetiformis is named for its resemblance to genital herpes. This is an erosive formation, in the field of which there are many small ulcers with clearly defined edges. Similar to Folman's balanitis, but in this case the ulcers do not merge.