Treatment under the compulsory medical insurance policy is possible!
Submit your application
Follow the news, subscribe to our social networks
Details
Heart rhythm disorders (arrhythmias) are conditions in which the heart beats irregularly, too fast, or too slow. With frequent heart contractions - above 100 beats per minute in adults, this condition is called tachycardia, with rare - less than 60 beats per minute, it is called bradycardia. Some types of arrhythmia have no symptoms. If the arrhythmia is symptomatic, then the main complaints are palpitations or a feeling of a pause between heartbeats. Sometimes patients may complain of dizziness, fainting, shortness of breath or chest pain. Most types of arrhythmia are not a serious threat to the patient, but complications such as stroke or heart failure can often occur, and sometimes the arrhythmia can lead to cardiac arrest.
The Innovative Vascular Center employs experienced cardiologists who will help determine exactly why cardiac arrhythmia occurs and prescribe the correct treatment. In addition to drug therapy, our clinic implants artificial pacemakers (pacemakers) of any configuration. Timely and correct treatment allows our patients to avoid many complications, which means prolonging life and improving its quality.
What is atrial fibrillation?
Atrial fibrillation is the most common type of arrhythmia, in which the atria contract chaotically and irregularly.
The sinus node, located in the right atrium, produces an impulse with a frequency of 60-80 per minute, which is transmitted throughout the conduction system of the heart. The organ contracts, forming a sinus rhythm. With atrial fibrillation, many foci of electrical excitation appear in them, as a result of which the atrium contracts very quickly, and at this moment the sinus node does not work. Paroxysms (episodes) of AF can be short and asymptomatic, or can last several days or months. AF itself is not dangerous, but in a third of all cases it leads to the development of ischemic stroke.
Why is atrial fibrillation dangerous?
The average Russian patient with atrial fibrillation is a 72-year-old man with coronary heart disease. AF itself is not a life-threatening condition, but can lead to the development of a severe clinical situation.
Ischemic stroke 75% of all strokes are ischemic strokes. Every third ischemic stroke occurs as a result of AF. How does this happen? With atrial fibrillation, the blood in the heart is turbulent and thrombosis occurs in the left atrium. This clot clogs the blood vessels and causes a cerebral infarction.
Myocardial infarction 6 out of 10 patients with AF have a history of coronary heart disease. If there is AF and coronary artery disease, then the risk of developing myocardial infarction increases 5 times.
Disability and death A European study based on data from 4,000 patients found that one in three people who had an ischemic stroke due to AF and did not take anticoagulants died within three months. The study showed an increase in the risk of disability by 43%, this is due to long-term rehabilitation.
| In 2020, the European Society of Cardiology developed an ABC algorithm of actions for atrial fibrillation: A - anticoagulants B - control of heart rate C - control of a person’s lifestyle |
Treatment of atrial fibrillation and flutter
What are the recommendations for antithrombotic therapy? How to choose a drug for preventive antiarrhythmic therapy?
Atrial fibrillation (AF) is one of the most common tachyarrhythmias in clinical practice, its prevalence in the general population ranges from 0.3 to 0.4% [1]. The detection of AF increases with age. Thus, among people under 60 years of age it is approximately 1% of cases, and in the age group over 80 years of age it is more than 6%. About 50% of patients with atrial fibrillation in the United States are over 70 years of age, and more than 30% of those hospitalized for cardiac arrhythmias are patients with this arrhythmia [2]. Atrial flutter (AFL) is a significantly less common arrhythmia compared to AF. In most countries, AF and AFL are considered different rhythm disorders and are not combined under the common term “atrial fibrillation.” In our opinion, this approach should be considered correct for many reasons.
Prevention of thromboembolic complications and relapses of atrial fibrillation and flutter
Atrial fibrillation and flutter worsen hemodynamics, aggravate the course of the underlying disease and lead to an increase in mortality by 1.5-2 times in patients with organic heart disease. Non-valvular (non-rheumatic) AF increases the risk of ischemic stroke by 2-7 times compared to the control group (patients without AF), and rheumatic mitral disease and chronic AF - by 15-17 times [3]. The incidence of ischemic stroke in non-rheumatic atrial fibrillation averages about 5% of cases per year and increases with age. Cerebral emboli recur in 30-70% of patients. The risk of another stroke is highest during the first year. The risk of stroke is low in patients with idiopathic AF under 60 years of age (1% per year), slightly higher (2% per year) at the age of 60-70 years. In this regard, most patients with frequent and/or prolonged paroxysms of atrial fibrillation, as well as its permanent form, should be prevented from thromboembolic complications. A meta-analysis of all studies on primary and secondary prevention of strokes showed that indirect anticoagulants reduce the risk of developing the latter by 47-79% (on average by 61%), and aspirin by a little more than 20%. It should be noted that when using aspirin, a statistically significant reduction in the incidence of ischemic stroke and other systemic embolisms is possible only with a fairly high dose of the drug (325 mg/day) [4]. At the same time, in the Copenhagen AFASAK Study [5], the number of thromboembolic complications in the groups of patients receiving aspirin 75 mg/day and placebo did not differ significantly.
In this regard, patients with AF who are at high risk for thromboembolic complications: heart failure, EF 35% or less, arterial hypertension, ischemic stroke or transient ischemic attack in history, etc., should be prescribed indirect anticoagulants (maintaining the International Normalized ratio - INR - on average at the level of 2.0-3.0). For patients with non-valvular (non-rheumatic) atrial fibrillation who are not at high risk, continuous use of aspirin (325 mg/day) is advisable. There is an opinion that in patients under 60 years of age with idiopathic AF, in whom the risk of thromboembolic complications is very low (almost the same as in people without rhythm disturbances), preventive therapy may not be required. Antithrombotic therapy in patients with AFL should obviously be based on taking into account the same risk factors as in AF, since there is evidence that the risk of thromboembolic complications in AFL is higher than in sinus rhythm, but somewhat lower than in AF [ 6].
International experts offer the following specific recommendations for antithrombotic therapy for various groups of patients with atrial fibrillation, depending on the level of risk of thromboembolic complications [7]:
- age less than 60 years (no heart disease - lone AF) - aspirin 325 mg/day or no treatment;
- age less than 60 years (heart disease, but no risk factors such as congestive heart failure, EF 35% or less, arterial hypertension) - aspirin 325 mg/day;
- age 60 years or more (diabetes mellitus or coronary artery disease) - oral anticoagulants (INR 2.0-3.0);
- age 75 years or more (especially women) - oral anticoagulants (INR up to 2.0);
- heart failure - oral anticoagulants (INR 2.0-3.0);
- LVEF 35% or less - oral anticoagulants (INR 2.0-3.0);
- thyrotoxicosis - oral anticoagulants (INR 2.0-3.0);
- arterial hypertension - oral anticoagulants (INR 2.0-3.0);
- rheumatic heart defects (mitral stenosis) - oral anticoagulants (INR 2.5-3.5 or more);
- artificial heart valves - oral anticoagulants (INR 2.5-3.5 or more);
- history of thromboembolism - oral anticoagulants (INR 2.5-3.5 or more);
- the presence of a thrombus in the atrium, according to TPEchoCG, - oral anticoagulants (INR 2.5-3.5 or more).
The international normalized ratio should be monitored with indirect anticoagulants at the beginning of therapy at least once a week, and subsequently monthly.
In most cases, patients with recurrent paroxysmal and persistent atrial fibrillation in the absence of clinical symptoms of arrhythmia or their insignificant severity do not need to be prescribed antiarrhythmic drugs. In such patients, prophylaxis of thromboembolic complications (aspirin or indirect anticoagulants) and heart rate control are carried out. If clinical symptoms are pronounced, anti-relapse and relief therapy is required, combined with heart rate control and antithrombotic treatment.
In case of frequent attacks of atrial fibrillation and flutter, the effectiveness of antiarrhythmics or their combinations is assessed clinically; in case of rare attacks, TES or VEM is performed for this purpose after 3-5 days of taking the drug, and when using amiodarone - after saturation with it. To prevent relapses of AF/AFL in patients without organic heart disease, antiarrhythmic drugs of classes 1A, 1C and 3 are used. In patients with asymptomatic LV dysfunction or symptomatic heart failure, and possibly with significant myocardial hypertrophy, therapy with class 1 antiarrhythmics is contraindicated due to the risk of worsening life prognosis.
To prevent paroxysms of atrial fibrillation and atrial flutter, the following antiarrhythmics are used: quinidine (kinylentine, quinidine durules, etc.) - 750-1500 mg/day; disopyramide - 400-800 mg/day; propafenone - 450-900 mg/day; allapinin - 75-150 mg/day; etacizin - 150-200 mg/day; flecainide - 200-300 mg/day; amiodarone (maintenance dose) - 100-400 mg/day; sotalol - 160-320 mg/day; dofetilide - 500-1000 mcg/day. Verapamil, diltiazem and cardiac glycosides should not be used for anti-relapse therapy of AF and AFL in patients with Wolff-Parkinson-White syndrome (WPU), since these drugs reduce the refractoriness of the accessory atrioventricular conduction pathway and can cause aggravation of the arrhythmia.
In patients with sick sinus syndrome and paroxysms of atrial fibrillation and flutter (bradycardia-tachycardia syndrome), there are expanded indications for implantation of an electrical pacemaker (pacemaker). Permanent pacing is indicated in such patients both for the treatment of symptomatic bradyarrhythmia and for the safe administration of preventive and/or curative antiarrhythmic therapy. To prevent and relieve attacks of AF and AFL in patients without pacemakers, class 1A antiarrhythmics with anticholinergic effects (disopyramide, procainamide, quinidine) can be used. In hypertrophic cardiomyopathy, amiodarone is prescribed to prevent tachyarrhythmia paroxysms, and beta-blockers or calcium antagonists (verapamil, diltiazem) are prescribed to reduce the frequency of ventricular contractions.
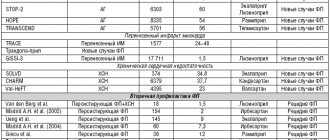
As a rule, treatment with antiarrhythmics requires monitoring the width of the QRS complex (especially when class 1C antiarrhythmics are used) and the duration of the QT interval (when treated with class 1A and 3 antiarrhythmics). The width of the QRS complex should not increase by more than 150% of the initial level, and the corrected QT interval should not exceed 500 ms. Amiodarone has the greatest effect in preventing arrhythmia [14, 15, 16, 17]. A meta-analysis of published results from placebo-controlled studies involving 1465 patients showed that the use of low maintenance doses of amiodarone (less than 400 mg/day) did not cause an increase in lung and liver damage compared with the placebo group [8]. Some clinical studies have demonstrated a higher preventive effectiveness of class 1C drugs (propafenone, flecainide) compared to class 1A antiarrhythmics (quinidine, disopyramide). According to our data, the effectiveness of propafenone is 65%, ethacyzine - 61% [9, 10].
Choice of drug for prophylactic antiarrhythmic therapy of paroxysmal and persistent atrial fibrillation and flutter
We can agree with the opinion expressed in international recommendations for the management of patients with atrial fibrillation [7], according to which anti-relapse therapy in patients without heart pathology or with minimal structural changes should begin with class 1C antiarrhythmics (propafenone, flecainide). Let's add to them domestic drugs of the same class (allapinin and etacizin), as well as sotalol; they are quite effective and devoid of pronounced extracardiac side effects. If the listed antiarrhythmics do not prevent relapses of AF/AFL or their use is accompanied by side effects, you should proceed to prescribing amiodarone and dofetilide. Then, if necessary, class 1A drugs (disopyramide, quinidine) or non-pharmacological treatments are used. Probably, in patients with so-called “adrenergic” AF, one can expect a greater effect from therapy with amiodarone or sotalol, and in “vagal” AF it is advisable to start treatment with disopyramide.
Coronary heart disease, especially in the presence of post-infarction cardiosclerosis, and heart failure increase the risk of manifestation of the arrhythmogenic properties of antiarrhythmic drugs. Therefore, treatment of atrial fibrillation and flutter in patients with congestive heart failure is usually limited to the use of amiodarone and dofetilide. While the high efficacy and safety of amiodarone in heart failure and coronary artery disease (including myocardial infarction) has been proven for a long time, similar results for dofetilide were obtained in the recent placebo-controlled studies DIAMOND CHF and DIAMOND MI [11].
For patients with coronary heart disease, the recommended sequence of prescribing antiarrhythmics is as follows: sotalol; amiodarone, dofetilide; disopyramide, procainamide, quinidine.
Arterial hypertension, leading to hypertrophy of the left ventricular myocardium, increases the risk of developing polymorphic ventricular tachycardia “torsades de pointes”. In this regard, to prevent relapses of AF/AFL in patients with high blood pressure, preference is given to antiarrhythmic drugs that do not significantly affect the duration of repolarization and the QT interval (class 1C), as well as amiodarone, although it prolongs it, but extremely rarely causes ventricular tachycardia . Thus, the algorithm for pharmacotherapy of this rhythm disorder in arterial hypertension appears to be as follows: LV myocardial hypertrophy of 1.4 cm or more - use only amiodarone; There is no left ventricular myocardial hypertrophy or it is less than 1.4 cm - start treatment with propafenone, flecainide (bear in mind the possibility of using domestic class 1C antiarrhythmics allapinin and etacizin), and if they are ineffective, use amiodarone, dofetilide, sotalol. At the next stage of treatment (ineffectiveness or occurrence of side effects of the above drugs), disopyramide, procainamide, and quinidine are prescribed [7].
It is quite possible that with the emergence of new results from controlled studies on the effectiveness and safety of antiarrhythmic drugs in patients with various diseases of the cardiovascular system, changes will be made to the above recommendations for the prevention of relapses of paroxysmal and persistent AF, since at present the relevant information is clearly insufficient.
If there is no effect from monotherapy, combinations of antiarrhythmic drugs are used, starting with half doses. An addition, and in some cases an alternative to preventive therapy, as mentioned above, may be the prescription of drugs that worsen AV conduction and reduce the frequency of ventricular contractions during paroxysms of AF/AFL. The use of drugs that impair conduction in the AV junction is justified even in the absence of effect from preventive antiarrhythmic therapy. When using them, it is necessary to ensure that the heart rate at rest is from 60 to 80 per minute, and with moderate physical activity - no more than 100-110 per minute. Cardiac glycosides are ineffective for controlling heart rate in patients leading an active lifestyle, since in such cases the primary mechanism for reducing the frequency of ventricular contractions is an increase in parasympathetic tone. Therefore, it is obvious that cardiac glycosides can be chosen only in two clinical situations: if the patient suffers from heart failure or has low physical activity. In all other cases, preference should be given to calcium antagonists (verapamil, diltiazem) or beta-blockers. In case of prolonged attacks of atrial fibrillation or flutter, as well as in their permanent form, combinations of the above drugs can be used to reduce heart rate.
Relief of paroxysms of fibrillation and atrial flutter
The primary task during an attack of the tachysystolic form of AF/AFL is to reduce the heart rate, and then, if the paroxysm does not stop on its own, stop it. Control of the ventricular contraction rate (decrease to 70-90 per minute) is carried out by intravenous administration or oral administration of verapamil, diltiazem, beta-blockers, intravenous administration of cardiac glycosides (preference is given to digoxin), amiodarone. In patients with reduced LV contractile function (congestive heart failure or EF less than 40%), heart rate is reduced only with cardiac glycosides or amiodarone. Before stopping tachysystolic forms of atrial fibrillation and atrial flutter (especially atrial flutter) with class 1A antiarrhythmics (disopyramide, procainamide, quinidine), conduction blockade in the AV node is required, since the above-mentioned antiarrhythmic drugs have an anticholinergic effect (most pronounced with disopyramide) and can significantly increase the frequency contractions of the ventricles.
Considering the risk of thromboembolism during prolonged paroxysm of AF, the issue of stopping it must be resolved within 48 hours, since if the duration of an attack of AF exceeds two days, it is necessary to prescribe indirect anticoagulants (maintaining the INR at the level of 2.0-3.0) for 3-4 weeks before and after electrical or drug cardioversion. Currently, the most widely used indirect anticoagulants are coumarin derivatives: warfarin and syncumar. If the duration of AF is unknown, the use of indirect anticoagulants before and after cardioversion is also necessary. Similar prevention of thromboembolic complications should be carried out in case of atrial flutter.
For pharmacological cardioversion, the following antiarrhythmics are used:
- amiodarone 5-7 mg/kg - intravenous infusion over 30-60 minutes (15 mg/min);
- ibutilide 1 mg - intravenous administration over 10 minutes (if necessary, repeated administration of 1 mg);
- novocainamide 1-1.5 g (up to 15-17 mg/kg) - intravenous infusion at a rate of 30-50 mg/min;
- propafenone 1.5-2 mg/kg - intravenous administration over 10-20 minutes;
- flecainide 1.5-3 mg/kg - intravenous administration over 10-20 minutes.
The international recommendations for cardiopulmonary resuscitation and emergency cardiac care [12] and the ACC/AHA/ECC recommendations for the treatment of patients with atrial fibrillation [7] note that it is advisable to relieve paroxysm in patients with heart failure or EF less than 40% mainly with amiodarone. The use of other antiarrhythmics should be limited due to the rather high risk of developing arrhythmogenic effects and the negative impact of these drugs on hemodynamics.
The use of verapamil and cardiac glycosides is contraindicated in patients with AF/AFL and Wolff-Parkinson-White syndrome. In the presence of the latter, AF/AFL is treated with drugs that impair conduction along the Kent bundle: amiodarone, procainamide, propafenone, flecainide, etc.
Oral relief of atrial fibrillation and flutter with quinidine, procainamide, propafenone, flecainide, dofetilide, etc. is possible.
Atrial flutter (type 1) can be relieved or converted to AF by frequent transesophageal or endocardial atrial pacemaker. Stimulation is prescribed for a duration of 10-30 seconds with a pulse frequency that is 15-20% higher than the frequency of atrial contractions, i.e. 300-350 (400) pulses per minute.
When AF/AFL is accompanied by severe heart failure (cardiac asthma, pulmonary edema), hypotension (systolic pressure less than 90 mm Hg), increased pain and/or worsening myocardial ischemia, immediate electrical pulse therapy (EPT) is indicated.
In case of atrial fibrillation, EIT begins with a discharge with a power of 200 J; for biphasic current, the energy of the first discharge is less. If it turns out to be ineffective, discharges of higher power (300-360 J) are successively applied. Atrial flutter is often relieved by a low-energy shock (50-100 J).
Electropulse therapy can also be chosen for the planned restoration of sinus rhythm in patients with prolonged paroxysms of AF/AFL. Medical cardioversion is recommended if EIT is not possible, undesirable, or fails to restore sinus rhythm. In case of an attack of AF/AFL lasting more than 48 hours, indirect anticoagulants before cardioversion can not be used for a long time if transesophageal echocardiography (TPEchocardiography) excludes the presence of thrombi in the atria (in 95% of cases they are localized in the left atrial appendage). This is the so-called early cardioversion: intravenous administration of heparin (increase in aPTT by 1.5-2 times compared to the control value) or short-term administration of an indirect anticoagulant (bringing the INR to 2.0-3.0) before cardioversion and four weeks of indirect administration anticoagulants after restoration of sinus rhythm. According to preliminary data from the ACUTE multicentre study [13], the incidence of thromboembolic complications is significantly lower when using TPEchoCG and short courses of preventive therapy with heparin or warfarin (in the absence of a thrombus) or longer-term administration of an indirect anticoagulant (if a thrombus is re-detected after three weeks of warfarin treatment) before EIT, than with traditional therapy carried out “blindly” with indirect anticoagulants for 3-4 weeks before and after electrical cardioversion, and is 1.2% and 2.9%, respectively. In patients who do not receive anticoagulants before cardioversion, thromboembolic complications develop in 1-6% of cases.
For severe paroxysms of AF and AFL, refractory to drug treatment, non-pharmacological treatment methods are used: destruction of the AV connection with implantation of an electrical pacemaker, “modification” of the AV connection, implantation of an atrial defibrillator or special pacemakers, radiofrequency catheter destruction of the impulse circulation path in the right atrium during AFL and sources ectopic impulses in patients with focal atrial fibrillation, “corridor” and “labyrinth” operations.
Literature
1. Kastor JA Arrhithmias. Philadelphia: WB Saunders company 1994. P.25-124. 2. Bialy D., Lehmann MN, Schumacher DN et al. Hospitalization for arrhythmias in the United States: importance of atrial fibrillation (abstr) // J. Am. Coll. Cardiol. 1992; 19:41A. 3. Wolf PA, Dawber TR, Thomas HE, Kannel WB Epidemiologic assessment of chronic atrial fibrillation and risk of stroke: the Framingham study // Neurology. 1978; 28: 973-77. 4. The Stroke Prevention in Atrial Fibrillation Study Group Investigators. Stroke prevention in atrial fibrillation study: final results//Circulation. 1991; 84:527-539. 5. Petersen P., Boysen G., Godtfredsen J. et al. Placebo-controlled, randomized trial of warfarin and aspirin for prevention of thromboembolic complications in chronic atrial fibrillation. The Copenhagen AFASAK study // Lancet. 1989; 1: 175-179. 6. Biblo LA, Ynan Z, Quan KJ et al. Risk of stroke in patients with atrial flutter // Am. J. Cardiol. 2000; 87: 346-349. 7. ACC/AHA/ESC guidelines for management of patients with atrial fibrillation//Circulation. 2001; 104: 2118-2150. 8. Vorperian VR, Havighurst TC, Miller S., Janyary CT Adverse effect of low dose amiodarone: a meta-analysis // JACC. 1997; 30: 791-798. 9. Bunin Yu. A., Fedyakina L. F., Bayroshevsky P. A., Kazankov Yu. N. Combined preventive antiarrhythmic therapy with etatsizin and propranolol for paroxysmal fibrillation and atrial flutter. Materials of the VII Russian National Congress “Man and Medicine”. Moscow, 2000. P. 124. 10. Semykin V.N., Bunin Yu.A., Fedyakina L.F. Comparative effectiveness of combined antiarrhythmic therapy with propafenone, verapamil and diltiazem for paroxysmal fibrillation and atrial flutter. Materials of the VII Russian National Congress “Man and Medicine”. Moscow, 2000. pp. 123-124. 11. Sager PT New advances in class III antiarrhytmic drug therapy. Curr. Opin. Cardiol. 2000; 15: 41-53. 12. Guidelines 2000 for cardiopulmonary resuscitation and emergency cardiovascular care // Circulation. 2000; 102 (suppl I): I-158-165. 13. Design of a clinical trial for the assessment of cardiversion using transesophageal echocardiography (the ACUTE multicenter study) // Am. J. Cardiol. 1998; 81: 877-883. 14. Bunin Yu. A., Firstova M. I., Enukashvili R. R. Maintenance antiarrhythmic therapy after restoration of sinus rhythm in patients with a permanent form of atrial fibrillation. Materials of the 5th All-Russian Congress of Cardiologists. Chelyabinsk, 1996. P. 28. 15. Bunin Y., Fediakina L. Low doses of amiodarone in preventing of paroxysmal atrial fibrillation and flutter. International academy of cardiology. 2nd international congress on heart disease. Abstract book of the congress, Washington, USA, 2001. 16. Gold RL, Haffajec CI Charoz G. et al. Amiodarone for refractory atrial fibrillation // Am. J. Cardiol. 1986; 57: 124-127. 17. Miller JM, Zipes DP Management of the patient with cardiac arrhythmias. In Braunwald E., Zipes D., Libby P. (eds). Heart disease. A textbook of cardiovascular medicine. Philadelphia: WB Saunders company. 2001. P. 731-736.
How do I know if I have atrial fibrillation?
The most common symptoms of AF are palpitations, shortness of breath and general weakness. You should not trust subjective sensations - you need to do a cardiogram or conduct daily Holter ECG monitoring.
Holter will help more accurately determine the presence of paroxysms. If the paroxysm lasts 30 seconds or more, you can consult a doctor for anticoagulants. There are 40 thousand heartbeats per day, of which there may be 400 extrasystoles (heartbeats out of rhythm) - this is the norm.
It happens that a person does not feel paroxysms - for example, when they happen at night. This is bad because small blood clots can form that will block small vessels in the brain. Loss of blood supply to some areas will lead to their death, which significantly increases the risk of developing dementia.
In young people, extrasystoles may have extra-cardiac causes - it is necessary to check the levels of ferritin, hemoglobin, thyroid hormones, examine the gastrointestinal tract in order to exclude reflux-esophagitis, which also causes rhythm disturbances, including atrial fibrillation. People with AF need to undergo liver, kidney and general blood tests every 6 months.
| There are three forms of atrial fibrillation: — Permanent form — Persistent form (AF goes away with medical help) — Paroxysmal form (AF appears and goes away on its own) |
Epidemiology of paroxysmal atrial fibrillation
Atrial fibrillation and flutter are the most common and dangerous types of heart rhythm disturbances and occur in 0.4–1.0% of cases in the population [1, 2].
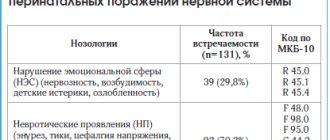
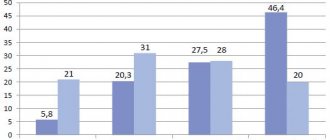
The incidence of atrial fibrillation/flutter increases with age. According to the Framingham Study, the incidence of atrial fibrillation (AF) doubles every 10 years of life: 0.55% in patients aged 50–59 years and 8.8% in patients aged 81–90 years [3]. Over the past 20 years, there has been a trend towards an increase in the incidence of AF, especially among men. In addition, there has been an increase in the number of hospitalizations for MA; in the USA, for example, this parameter increased 2.5 times over the period from 1985 to 1999 [4, 5]. The negative impact of atrial fibrillation/flutter was also studied: the risk of thromboembolic complications increased by 4–5 times, the mortality rate by 1.5–2.0 times [6, 7]. This pathology can lead to the development and progression of heart failure and a decrease in quality of life. Among patients hospitalized for cardiac arrhythmias, AF occurs in 34%, atrial flutter – in 4% of cases.
As a rule, at the very beginning, MA is paroxysmal. The prevalence of AF paroxysms varies, according to various sources, in the range of 22–65%. Of these, in 35–78% of cases, the paroxysmal form of arrhythmia becomes persistent [8].
Definition, classification of paroxysms of flickering
The term “paroxysmal atrial fibrillation” refers to a rhythm disturbance associated with chaotic contraction of individual groups of atrial muscle fibers, lasting no more than 7 days with the possibility of spontaneous relief. The frequency of atrial waves can reach up to 600 beats/min. Due to the variability of atrioventricular conduction under these conditions, partly due to the hidden conduction of some impulses, the ventricles contract randomly. In the absence of additional disturbance of atrioventricular conduction, the ventricular rate is about 100–150 beats per minute (tachysystolic atrial fibrillation). It is believed that the electrophysiological basis of atrial fibrillation is multiple small circles of impulse circulation in the atrial myocardium. Attacks of atrial fibrillation, especially the normo- and bradysystolic forms, often do not cause pronounced hemodynamic disorders and may not be accompanied by a noticeable deterioration in the patient’s condition and well-being.
In terms of prescribing differentiated therapy, it is noteworthy to distinguish two forms of paroxysmal MA: with a predominance of the tone of the parasympathetic nervous system (“vagal” paroxysmal MA) and with a predominance of the tone of the sympathetic nervous system (“adrenergic”, “catecholamine” paroxysmal arrhythmia) [9].
Definition, classification of flutter paroxysms
Atrial flutter is a regular contraction of the atria at a rate of about 250–350 beats per minute. The ventricular rhythm may be regular or irregular. The frequency and regularity of the ventricular rhythm during atrial flutter is determined by atrioventricular conduction, which can change. Atrial flutter occurs 10–20 times less frequently than paroxysmal fibrillation. Sometimes atrial fibrillation and flutter alternate in one patient. The term “atrial fibrillation” was proposed by G.F. Lang to designate atrial fibrillation and flutter due to the commonality of some pathogenetic and clinical features, however, in the diagnosis, arrhythmia must be specifically designated as fibrillation or flutter.
With the paroxysmal form of flutter, the frequency of paroxysms can be very different: from once a year to several times a day. Paroxysms can be triggered by physical activity, emotional stress, hot weather, drinking too much, alcohol, and even intestinal upset. Paroxysms sometimes go away on their own, but sometimes drug treatment is required. Some people with MA do not feel it, while others notice a slight irregularity in their heart rhythm. You may also experience dizziness, pressure, and chest pain.
Atrial flutter, being one of the forms of AF, differs little in clinical manifestations from atrial fibrillation, but is characterized by somewhat greater persistence of paroxysms and greater resistance to antiarrhythmic drugs. There are regular (rhythmic) and irregular forms of this arrhythmia. The latter is clinically more similar to atrial fibrillation. In addition, there are two main types of atrial flutter: 1 – classic (typical); 2 – very fast (atypical) [10].
Pathogenesis of atrial fibrillation/flutter
It was found that AF is predominantly an atrial tachyarrhythmia, which begins and forms in the left atrium, where several microreentry circles occur. Atrial flutter, on the other hand, usually occurs in the right atrium - in its lower part. The macroreentry circle, which underlies atrial flutter, is located mainly in the area (bridge) of the right atrium connecting the mouth of the inferior vena cava and the tricuspid valve annulus. Naturally, in our time, methods of treating paroxysms of atrial fibrillation and atrial flutter - these two related, but still different atrial tachyarrhythmias - should be considered separately.
Diagnosis of atrial fibrillation/flutter
In AF, the electrocardiogram (ECG) shows no P wave, diastole is filled with small waves of irregular configuration and rhythm, more noticeable in lead VI. Their frequency is 300–600 beats per minute (usually not counted). Ventricular complexes follow an irregular rhythm and are usually not deformed. With a very fast ventricular rhythm (more than 150 beats/min), blockade of the leg, usually the right one, of the atrioventricular bundle is possible. Under the influence of treatment, as well as in the presence of atrioventricular conduction disturbances along with atrial fibrillation, the ventricular rate may be lower. At a frequency of less than 60 beats/min, we speak of the bradysystolic form of atrial fibrillation. Occasionally, atrial fibrillation is combined with complete atrioventricular block. At the same time, the ventricular rhythm is rare and regular. In persons with paroxysms of atrial fibrillation, when recording an ECG outside the paroxysm, especially soon after it, a more or less pronounced deformation of the P wave is often detected.
With atrial flutter, the ECG reveals regular atrial waves without diastolic pauses, having a characteristic sawtooth appearance, more clearly expressed in lead AVF. Atrial waves fill the ventricular diastole, they are also superimposed on the ventricular complexes, slightly deforming them. Ventricular complexes can follow rhythmically - after every second (then the ventricular rhythm is about 120-160 beats / min), third, etc. atrial wave, or arrhythmically, if the ratio of atrial and ventricular contractions is not constant. With a frequent ventricular rhythm, a violation of intraventricular conduction is possible, more often - blockade of the right leg of the atrioventricular bundle. With a frequent and regular ventricular rhythm, flutter is difficult to distinguish by ECG from other supraventricular tachycardias. If it is possible to temporarily reduce atrioventricular conduction (using carotid sinus massage, digoxin or 5 mg verapamil), the ECG picture becomes more characteristic.
Treatment of atrial fibrillation
When treating patients with atrial fibrillation and flutter at the prehospital stage, the feasibility of restoring sinus rhythm should be assessed. The absolute indication for restoration of sinus rhythm during the development of paroxysmal AF is the development of pulmonary edema or arrhythmogenic shock. In this case, emergency cardioversion should be performed prehospital.
Contraindications to restoring sinus rhythm at the prehospital stage include:
- the duration of paroxysm of atrial fibrillation is more than two days;
- proven dilatation of the left atrium (antero-posterior size 4.5 cm, according to echocardiography);
- presence of blood clots in the atria or a history of thromboembolic complications;
- development of paroxysm against the background of acute coronary syndrome (in the presence of stable hemodynamics);
- development of paroxysm against the background of pronounced electrolyte disturbances;
- decompensation of thyrotoxicosis;
- severe chronic hemodynamic disorders and some others.
In such cases, treatment should be aimed at stabilizing hemodynamics, preventing thromboembolism and controlling the heart rate in order to maintain it within 60–90 beats/min.
The drug of choice for heart rate control is cardiac glycosides, particularly digoxin. Further tactics are determined in the hospital. Persistent normosystolic form of AF without signs of heart failure does not require antiarrhythmic therapy at all [11].
It is known that 50–60% of recently developed (less than 48 hours) paroxysms of AF cease spontaneously. S. Ogawa et al. [12] in the J-RHYTHM study found that parameters such as mortality and the number of complications when stopping paroxysms of atrial fibrillation do not depend on the chosen treatment tactics (lowering the heart rate or restoring sinus rhythm). Similar results were obtained in their study by SH Hohnloser et al. [13].
Starting to characterize the methods of drug treatment of paroxysms of AF, we consider it necessary to emphasize that an antiarrhythmic drug has not yet been synthesized that can eliminate paroxysms of atrial fibrillation in every patient. The doctor must have a set of various effective drugs in order to be able to adequately replace one drug with another. Typically, treatment of AF paroxysm begins with an intravenous infusion of potassium chloride solution, often together with digoxin. Potassium chloride itself often eliminates paroxysms of AF after 3–5 infusions. In addition, an increase in plasma potassium concentration by 0.5–1.5 µm/l creates a favorable background for the subsequent action of other antiarrhythmic drugs.
In case of failure with the use of cardiac glycoside and potassium chloride or in the presence of contraindications to the use of cardiac glycosides, procainamide is administered. If necessary, this can be done earlier, for example, after 1-2 infusions of potassium chloride solution. According to the observations of various authors, the results of treatment of AF with procainamide are noticeably improved if it is administered to patients 20–30 minutes after intravenous infusion of a solution of potassium chloride and cardiac glycoside. In this way, sinus rhythm was restored in 65% of patients who did not respond at the prehospital stage to a sufficiently large dose of procainamide (up to 15 ml of a 10% solution) administered intravenously [14].
Effective antiarrhythmic drugs that are recommended for clinical use for the purpose of conversion of atrial AF are the IC class drugs propafenone and flecainide. They are effective when administered intravenously and orally. Sinus rhythm in patients with AF is restored 2–6 hours after oral administration. According to a placebo-controlled study by Yu.A. Bunina et al. [15], the effectiveness of propafenone in AF (single oral dose of 600 mg, observation for 8 hours) is about 80%. However, several randomized controlled studies emphasize the limited ability of intravenously administered propafenone to convert atrial flutter (no more than 40%). Our observations also indicate a rather low effectiveness of propafenone in the oral treatment of atrial flutter.
The use of class IC antiarrhythmics is contraindicated in patients with acute myocardial ischemia (unstable angina, myocardial infarction). A meta-analysis showed that antiarrhythmics of classes IC, IA and III have approximately the same effectiveness in stopping AF. However, no evidence was found of any effect of these drugs on the survival and quality of life of patients [16].
If a paroxysm of AF is preceded by an increase in sinus rhythm, if the paroxysm occurs in the daytime under the influence of stressors, physical or emotional stress, it must be assumed that the basis of such paroxysm is a hypersympathicotonic mechanism. Verapamil, diltiazem and β-blockers are first-line drugs for emergency intravenous reduction of heart rate, because these antiarrhythmics are highly effective and quickly (within 5-10 minutes) exert their effect. With intravenous digoxin, a sustained slowdown in ventricular rate is achieved much later (after 2–4 hours). For patients with a high risk of systemic embolism (atrial fibrillation/flutter lasting more than 2 days), in order to reduce the heart rate, amiodarone is a reserve drug, after the use of which it is possible to restore sinus rhythm and, consequently, the appearance of “normalizing” thromboembolism [17].
A number of international recommendations [18, 19] note that the relief of paroxysmal fibrillation/flutter in patients with heart failure or a left ventricular ejection fraction of less than 40% should be carried out with amiodarone. Other antiarrhythmics should be used with caution or not be used due to the relatively high risk of developing arrhythmogenic effects and negative effects on hemodynamics. A meta-analysis of the results of placebo-controlled studies of cardioversion of AF with amiodarone showed late relief of arrhythmia paroxysms: a significant difference in effectiveness between amiodarone and placebo was noted no earlier than 6 hours after their intravenous use. Taking this into account, after an intravenous “loading” dose of amiodarone is administered, it is then advisable to continue its intravenous infusion for 6–2 hours.
In a study by R.D. Kurbanova et al. [20] found that a course of treatment with a saturating dose of amiodarone helps restore sinus rhythm in 30% of patients with dilated cardiomyopathy complicated by AF. At the same time, long-term treatment with amiodarone helps maintain sinus rhythm in the next 6 months and compensates for heart failure. A meta-analysis also showed that treatment with amiodarone facilitates the procedure for restoring sinus rhythm and has a positive effect on patient survival [21].
In the study by S.A. Filenko [22] found that in patients with coronary heart disease, the paroxysmal form of AF occurs in the sympathetic and mixed types. In a study of drugs that have an anti-relapse effect on paroxysmal fibrillation, it was shown that amiodarone is the most effective, and in patients with paroxysmal AF of the sympathetic type, metoprolol also turned out to be effective.
S.A. Starichkov et al. [23] studied patients with arterial hypertension (AH) suffering from AF. Analysis of the results showed that the use of a combination of amiodarone and metoprolol for hypertension makes it possible to reduce the doses of antiarrhythmic drugs used and contributes not only to more effective control of blood pressure levels, but also to the prevention of AF paroxysms in 71% of patients. The use of β-blockers, both as monotherapy and in combination with amiodarone, leads to normalization of heart rate variability and has a positive effect on the processes of myocardial remodeling in various chambers of the heart.
It is known that blockade of type 1 angiotensin II receptors, in addition to lowering blood pressure, can lead to a decrease in myocardial remodeling and hypertrophy, normalization of electrolyte balance, and has indirect anti-ischemic and anti-adrenergic effects [24]. In the study by Yu.G. Schwartz et al. [25] treatment with losartan in patients with a combination of paroxysms of AF and hypertension was accompanied by a significant decrease in the frequency of arrhythmia paroxysms, in contrast to patients treated with nifedipine and atenolol. The authors believe that the likely mechanism for the positive effect of losartan on the course of AF paroxysms is a direct effect on the myocardium. Even J. Mayet [26] suggested that regression of left ventricular hypertrophy is associated with the antiarrhythmic effect of antihypertensive therapy.
One promising avenue for the treatment of arrhythmias is the use of omega-3-polyunsaturated fatty acids (ω-3-PUFA). In 2005, a study was published showing that consumption of fatty fish rich in long-chain ω-3-PUFA may reduce the risk of AF [27]. The authors explained this antiarrhythmic effect of ω-3-PUFA by reducing blood pressure and improving left ventricular diastolic function.
I.V. Antonchenko et al. [28] found that one of the possible mechanisms of the protective effect of ω-3-PUFA in patients with paroxysmal AF is reverse electrical remodeling of the atrial myocardium. The addition of ω-3-PUFAs to relief therapy reduces the number of episodes of AF and the time of their relief. However, the electrophysiological effects of using ω-3-PUFA at a dose of 1 g/day occur no earlier than the 20th day of administration.
The treatment tactics for paroxysms of atrial flutter largely depend on the severity of hemodynamic disorders and the patient’s well-being. This arrhythmia often does not cause severe hemodynamic disturbances and is little felt by the patient even with significant ventricular tachysystole. In addition, such paroxysms are usually difficult to stop with intravenous administration of antiarrhythmics, which can even cause a deterioration in the patient’s condition. Therefore, in these cases, emergency treatment is usually not required.
Speaking about drug treatment of this arrhythmia, it should be borne in mind that, according to the authors of the “Sicilian Gambit” concept [29], paroxysms of type I atrial flutter are better controlled by class IA drugs (quinidine, procainamide, disopyramide). However, when using drugs of this class there is a risk of paradoxical acceleration of the ventricular rate, so it is better to first use verapamil or beta-blockers. Paroxysms of type II atrial flutter are better controlled by class I3 drugs, in particular amiodarone. Domestic authors note the high effectiveness of nibentan in relieving paroxysms of fibrillation and especially atrial flutter [30].
It has now been proven that mental disorders worsen the course of arrhythmias, in particular AF, by complicating clinical manifestations and reducing quality of life. There is also an opinion that patients with depressive disorders have a violation of the autonomic regulation of heart rhythm (decreased parasympathetic and increased sympathetic tone), which increases the risk of AF.
In the study by B.A. Tatarsky et al. [31] the addition of Afobazole was accompanied by a pronounced anxiolytic effect without severe sedation, effective correction of autonomic disorders, and the absence of drug dependence and withdrawal syndrome. It was found that Afobazole treatment of patients with paroxysmal AF without pronounced structural changes in the heart was accompanied by a decrease in the frequency of paroxysms, the duration of arrhythmia episodes, and easier tolerability; there was a tendency to transform into an asymptomatic form.
The effectiveness of nibentan in relieving paroxysmal atrial fibrillation and atrial flutter is more than 80% [32]. Nibentan and ibutilide should be used only in specialized departments under ECG control (contraindicated in patients with heart failure, prolonged QT interval and sick sinus syndrome).
In patients with Wolff–Parkinson–White syndrome, the frequency of ventricular contractions during fibrillation/flutter, as a rule, is higher than in patients without ventricular preexcitation syndrome, and reaches 220–250 beats per minute or more, and tachycardia with abnormal rhythm and wide QRS complexes. The use of verapamil, diltiazem, and cardiac glycosides is contraindicated in Wolff–Parkinson–White syndrome, because, by reducing the refractoriness of the Kent bundle, they can increase the heart rate and even cause ventricular fibrillation. Atrial fibrillation/flutter is treated with drugs that impair conduction along the accessory atrioventricular conduction pathway. International recommendations for the treatment of patients with AF [19] suggest primarily using intravenous procainamide or ibutilide for this purpose.
Conclusion
In conclusion, it must be emphasized that the goal of antiarrhythmic therapy, like any other, is not only to eliminate and prevent paroxysmal arrhythmias, but also to improve the life prognosis, as well as reduce the mortality of patients, and for this it is very important to prevent the negative hemodynamic and proarrhythmic effects of the drugs used . The development of “antiarrhythmic drugs of the future” to provide sinus rhythm control must be based on a combination of efficacy and safety of therapy. Drugs with improved electrical, structural, and triggering properties are likely to reduce mortality and complications in patients with atrial fibrillation/flutter in the future.
Information about the authors: Volkov Viktor Evgenievich – candidate of medical sciences, researcher at the Federal State Institution RKNPK. Email; Yulia Vladimirovna Dotsenko – Candidate of Medical Sciences, researcher at the Federal State Institution RKNPK. Kiryushina Irina Evgenievna – doctor geneticist of the Federal State Institution RKNPK
The main drugs for preventing stroke in AF are anticoagulants
The main drugs for patients with AF that prevent stroke are anticoagulants, the effect of which reduces blood clotting. They prevent the formation of blood clots and therefore reduce the risk of stroke. Coagulation is a normal protective reaction of the body to damage to the vascular wall. With atrial fibrillation, anticoagulants are absolutely necessary for almost everyone.
The most famous anticoagulants in Russia are Eliquis, Xarelto and Pradaxa.
Also, some patients can take Warfarin (with INR monitoring). It is prescribed for low glomerular filtration rate (or creatinine clearance - an indicator of kidney function) or for prosthetic valves.
When taking Warfarin, it is necessary to monitor the INR in the blood (International Normalized Ratio) - the indicator should be from 2.0 to 3.0.
| The main drugs for patients with AF that prevent stroke are anticoagulants, the effect of which reduces blood clotting. With atrial fibrillation, anticoagulants are absolutely necessary for almost everyone. |
Treatment
Conservative treatment of atrial fibrillation (atrial fibrillation)
Atrial fibrillation is a risk factor for ischemic stroke, which develops as a result of the formation of blood clots in the cavity of the left atrium. The first-line treatment for atrial fibrillation is drugs that prevent blood clots. They are prescribed by a doctor, because... monitoring of the blood coagulation system is required. These drugs are indicated for almost all patients who suffer from atrial fibrillation, regardless of whether the arrhythmia is constantly present or occurs in attacks (paroxysmal form of arrhythmia). The risk of stroke is the same both in the presence of a chronic form of arrhythmia and in a paroxysmal form of arrhythmia.
In patients with paroxysmal atrial fibrillation, the issue of preventing the occurrence of arrhythmia attacks is addressed. If the attack occurs for the first time, antiarrhythmic drugs are not prescribed. Medications may be recommended to control heart rate and improve tolerance to repeated episodes of arrhythmias. Antiarrhythmic drugs are also not prescribed if the patient’s arrhythmia attacks are asymptomatic and do not reduce his quality of life. If rhythm disturbances recur and paroxysm tolerance deteriorates, the cardiologist-arrhythmologist, together with the patient, decides on the prescription of antiarrhythmic drugs or surgical treatment of arrhythmia (catheter ablation).
If a prolonged attack of atrial fibrillation develops, which does not go away on its own, it is necessary to contact a specialist cardiologist-arrhythmologist, who will choose the most suitable method for stopping the arrhythmia for the patient. A technique for medicinal restoration of normal heart rhythm has been developed, as well as a procedure for restoring rhythm using electrical cardioversion. To restore the rhythm, a certain medication preparation is necessary, the regimen of which will be determined by the doctor, based on the individual characteristics of the course of the disease. With the advent of the latest highly effective antiarrhythmic drugs, preference is given to drug restoration of rhythm.
When transforming the paroxysmal form of atrial fibrillation into a chronic form, the main task is to control the heart rate. In the presence of tachysystole (high heart rate), drugs are prescribed that reduce the heart rate, the primary of which are beta-blockers. An integral part of the treatment of atrial fibrillation is the treatment of the disease that provoked the rhythm disturbance - coronary heart disease, heart failure, arterial hypertension, disorders of the thyroid gland and others.
It is necessary to contact a cardiologist-arrhythmologist if:
- development of an attack of atrial fibrillation for the first time in life,
- development of another attack of arrhythmia that cannot be controlled by usual means,
- ineffectiveness of previously prescribed antiarrhythmic therapy.
Anticoagulants can only be taken as prescribed by a doctor.
Standard dosage: Xarelto 20 mg / once a day Eliquis 5 mg / 2 times a day Pradaxa 150 mg / 2 times a day
Studies show that patients are more comfortable taking Xarelto - taking it once a day is easier to remember, especially for older people.
"Wafarin": take one tablet in the evening, take the INR test after 3-4 days. If the INR does not reach 2.0, then the doctor should increase the dosage. The INR should be taken every 3-4 days until the desired level is reached. Then you need to take an INR test every 3 weeks.
Important: all medications and their dosage are prescribed strictly during an in-person consultation with a doctor! This information is for informational purposes only and cannot be a guide to action. Self-medication for arrhythmia is unacceptable and can have serious health consequences.
| Reducing the dosage of anticoagulants mainly depends on only three parameters: — Creatinine clearance is less than 50. — The patient’s weight is less than 65 kg. — The patient’s age is over 85 years. In other cases, reducing the dosage risks a stroke. |
Anticoagulants thin the blood - is it dangerous?
Like any blood thinners, anticoagulants can cause bleeding. However, the risk of bleeding is 10 times lower than the risk of stroke. If a person has spontaneous bruises, nosebleeds, heavy menstruation, or blood in the urine, this is not an indication that the dosage needs to be reduced. Minor bleeding does not cause death, unlike a stroke. If you have the above symptoms of bleeding, you need to come for an examination to your attending physician - a gynecologist, urologist and, of course, a cardiologist.
| If a person takes anticoagulants, he must take a general blood test, creatinine, glomerular filtration rate (creatinine clearance), potassium, sodium, ALT, AST every 6 months. |
Dangerous or useless drugs
● 50% of strokes in AF are associated with the fact that a person takes aspirin. Neither aspirin, nor Clopidogrel, nor their combination protects a person from the development of ischemic stroke. ● Many people take blood-thinning drugs when there is no reason for this, others are ready to replace anticoagulants with Cardiomagnyl, Mildronate, Riboxin - this cannot be done. ● “Preductal” can cause extrasystole and increase arrhythmia; it is used only for coronary heart disease. ● The heart cannot be “nourished” with anything; there are no “vitamins for the heart.” The heart is a reflection of your lifestyle - nutrition, movement, sleep.
Etiology of AF and cardiovascular risks
Atrial fibrillation is defined as a supraventricular tachyarrhythmia characterized by chaotic electrical activity of the atria at a high rate (350-700 per minute) and an irregular ventricular rhythm1. Previously, the term “atrial fibrillation” was widely used, which quite accurately conveys the essence of atrial fibrillation.
According to foreign studies, AF is the most common form of tachyarrhythmia in the world and occurs in 2% of the population2. There are valvular and non-valvular AF (NVAF). In the first case, AF is associated with damage to the heart valves and overload of the left atrium with pressure or volume, due to which fibrillation begins. The most common cause of valvular AF is rheumatic mitral valve stenosis or replacement1. All other cases of atrial fibrillation are defined as non-valvular.
NFP occurs against the background of a number of diseases and conditions, such as coronary heart disease, hypertension, primary myocardial diseases, diabetes mellitus, pheochromocytoma, as well as alcohol abuse, excess body weight and hypokalemia3. Due to the chaotic movement of blood in the fibrillating left atrium, the prerequisites are created for the formation of blood clots, which can spread through the left ventricle throughout the systemic circulation. Thromboembolic complications are the most dangerous complications of AF. These include:
- ischemic cardioembolic stroke;
- heart attacks of internal organs;
- thromboembolism of the vessels of the extremities.
In a cardioembolic stroke, an embolus (thrombus) located in the left atrium breaks off and enters the arterial system of the brain.
According to a number of epidemiological studies, NFP increases the risk of stroke by 2.6-4.5 times, depending on the clinical parameters of patients4. Moreover, for women, these risks, other things being equal, are higher than for men5.
A stroke that occurs during NAF is severe and more often leads to disability than a stroke in patients without AF6. The basis for the prevention of thromboembolism in NFP is oral anticoagulants. They reduce the activity of blood clotting and thus prevent the formation of emboli (blood clots). 10 years ago, the drug of choice was the vitamin K antagonist warfarin, but direct oral anticoagulants (DOACs) appeared, in particular apixaban, which have a number of advantages over warfarin, which allowed DOACs to become the standard for stroke prevention in NAF.
Why do you need to control your lifestyle?
Because it affects the size of the left atrium. The more severe the obesity, the larger the size of the left atrium. If a person is overweight, the pressure in the heart increases, the volume of circulating blood increases, and the left atrium stretches. The larger the left atrium is from normal (400 mm), the higher the risk of developing atrial fibrillation.
Situations
With normal left atrium size, the effectiveness of radiofrequency ablation can reach 70%. The larger the size of the left atrium, the lower the effectiveness of RFA.
● If a patient is undergoing radiofrequency ablation, it is important to remember: the more abnormal the atrial function is, the higher the risk of recurrent atrial fibrillation. ● When a person’s heart rhythm is lost, during an ultrasound they pay attention to the size of the left atrium: if it is slightly dilated, it makes sense to try to restore this rhythm using medications or electrical pulse therapy. But if the left atrium is significantly dilated, there is no particular point in restoring the rhythm - sooner or later it will break down again.
What to do?
● Control your weight. ● Avoid alcohol - alcohol increases the risk of bleeding and aggravates the course of the arrhythmia or increases the frequency of breakdowns of this arrhythmia. ● Stop smoking. ● Stop taking dietary supplements - most of them can enhance the effect of anticoagulants. ● Increase physical activity. ● Monitor the condition of the thyroid gland by an endocrinologist.
Slow heartbeat - bradycardia
Bradycardia is a condition where the heart beats so slowly that it cannot pump enough blood to meet the body's needs. If bradycardia is left untreated, it can lead to extreme fatigue, dizziness, or fainting because not enough blood is supplied to the brain. This condition can be corrected by using an electronic pacemaker, which makes the heart beat normally.
Bradycardia occurs for various reasons:
- Sick sinus syndrome
The appearance of sinus bradycardia as a result of a “malfunction” in the sinus node (the natural pacemaker of the heart) occurs when discharges for contractions occur too infrequently. A weak sinus node can develop with age or be a consequence of illness. Some medications may also cause or worsen bradycardia. This arrhythmia may be temporary or permanent. It can be treated with medications or an electronic pacemaker.
- Blockage of the heart pathways
Heart block is a slowing or interruption of the electrical signal to the lower chambers of the heart (ventricles) that cause the heart muscle to contract. The heart's electrical conduction system typically sends signals from the upper chambers of the heart (atria) to the lower chambers (ventricles), which causes coordinated contractions of the heart muscle. Complete blockade of the atrioventricular node can manifest as a sudden loss of consciousness, since the ventricles contract very rarely without stimulus from the sinus node. An artificial pacemaker can eliminate this problem and normalize heart function.