The role of the renin–angiotensin–aldosterone system in the pathogenesis of atrial fibrillation
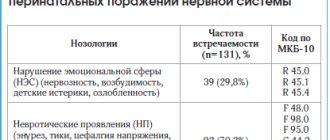
Currently, AF is recognized as a heterogeneous clinical and electrophysiological entity with different mechanisms, triggers, and substrates for the occurrence and maintenance of arrhythmia, which requires different approaches to its treatment and prevention. However, in most cases, treatment of AF remains symptomatic, including preventive anticoagulant and pharmacological therapy. Protective antiarrhythmic therapy has low effectiveness and is associated with a high risk of side effects. These limitations in the use of antiarrhythmic drugs have led to the use of non-pharmacological treatments and the development of specific therapeutic strategies aimed at preventing the development of an electrophysiological environment that supports arrhythmia. In recent years, data have been obtained on the effect of drugs that do not have direct antiarrhythmic properties on the incidence and recurrence of AF. This area of treatment is called “upstream therapy,” literally translated as “therapy directed against the flow” or, more precisely, “not within the framework of conventional antiarrhythmic therapy.” This group of drugs includes drugs that can affect the pathogenetic mechanisms of AF: inflammation, fibrosis, oxidative stress and remodeling of the atrial myocardium. Therefore, unlike antiarrhythmic therapy, which is exclusively symptomatic, “upstream therapy” can be called pathogenetic. One of the promising and promising areas in the treatment of AF is the use of drugs that block the renin-angiotensin-aldosterone system (RAAS). The corresponding section first appeared in new recommendations for the diagnosis and treatment of AF [1]. The role of the RAAS in the pathogenesis of various diseases of the cardiovascular system has long been well known, but recent studies have proven the direct influence of the components of the RAAS on the electrophysiological properties of atrial cardiomyocytes. There are several main pathogenetic mechanisms of the direct effect of the RAAS on the structural and electrophysiological remodeling of the atria: increased fibrosis of atrial tissue, stretching and dilatation of the atria, a direct effect on the function of ion channels and intercellular interaction of atrial cardiomyocytes [3]. The leading link in the pathogenesis of the development and maintenance of AF is changes in the anatomical properties of the atria, which include: dilatation of the atria, dilatation of the pulmonary veins, apoptosis of atrial cardiomyocytes, interstitial fibrosis, increased mass of the atrial myocardium, expression of ion channel genes [4], changes in the distribution of vulnerable areas [5]. Atrial hypertrophy and dilatation reflect the processes of “arrhythmogenic remodeling” [6]. Much less often, heterogeneous areas of fibrosis and fatty infiltration of the atrial myocardium are detected, which may be the outcome of inflammatory or degenerative processes in the heart muscle. AF most often occurs in patients with CHF, which leads to extensive interstitial fibrosis of the atria and increased production of type I collagen [7]. Kostin S. et al. (2002) during an electron microscopic study of biopsy material from the atrium of patients with AF, discovered a violation of intercellular contacts and apoptosis of atrial cardiomyocytes. The described changes, according to the authors, ensure the occurrence and increase the duration of an episode of AF [8]. Experimental work in recent years has revealed an increase in type I angiotensin II receptors and the level of angiotensin-converting enzyme in the left atrium tissue of patients with AF [9,10]. Stimulation of angiotensin II type I receptors initiates a cascade of phosphorylation processes and activates various mitogen-activated protein kinases, which leads to hypertrophy and apoptosis of atrial cardiomyocytes, accumulation of fibroblasts and collagen induction [11]. Increased readiness for the onset of AF is associated with a progressive decrease in the effective refractory period of the atria. These changes are called the phenomenon of electrophysiological remodeling of the atria [1]. The components of the RAAS directly affect changes in the transport of calcium and sodium ions across the cardiomyocyte membrane. Angiotensin II initiates the activation of L-type calcium channels, and similar changes in the transport of calcium ions occur with an increase in aldosterone concentrations [12,13]. A change in the flow of ions through L-type calcium channels leads to a shortening of the action potential, a decrease in the effective refractory period of the atria and the appearance of AF. The influence of the tissue component of the RAAS on the permeability of the cardiomyocyte membrane for sodium ions has been proven. An increase in the concentration of angiotensin II reduces the transport of sodium ions into the cell, thereby changing the excitability threshold of atrial cardiomyocytes [14]. In addition, in vitro studies have proven that an increase in angiotensin II promotes phosphorylation of the CX43 membrane protein and changes in intercellular connections of cardiomyocytes [15]. Violation of intercellular interaction reduces the speed of propagation of the excitation wave through the atria and initiates the appearance of AF. Thus, activation of the RAAS plays a leading role in the development of structural remodeling of the atria, which leads to changes in the electrophysiological properties of atrial tissue and the occurrence of AF. There is reason to believe that blockade of the RAAS can reduce the number of newly diagnosed episodes of AF and prevent repeated paroxysms of arrhythmia. To date, 23 large randomized clinical trials have been conducted to study the effect of ACE inhibitor (ACEI) and angiotensin receptor blocker (ARB) therapy on the incidence of new episodes of AF or its secondary prevention (Table 1). The total number of patients included in the meta-analysis was 87,048 people. For the purpose of primary prevention of AF, ACEIs or ARBs were used in patients with arterial hypertension (AH), CHF, and after myocardial infarction (MI). Secondary prevention of AF was carried out by co-administration of ACE inhibitors or ARBs with antiarrhythmic drugs after cardioversion or to maintain sinus rhythm in patients with persistent AF [16]. Primary prevention of AF using ACE inhibitors or ARBs Arterial hypertension. A total of 6 studies were conducted evaluating the primary prevention of AF with ACE inhibitors or ARBs in patients with hypertension. Of these, only two studies—LIFE (Losartan Intervention For Endpoint Reduction in Hypertension) and VALUE (Valsartan Antihypertensive Long-Term Use Evaluation)—found a statistically significant reduction in the incidence of new cases of AF when prescribing ARBs [17,18]. The remaining studies - CAPP (Captopril Prevention Project), STOP-2 (Swedish Trial in Old Patients With Hypertension-2), HOPE (Heart Outcomes Prevention Evaluation) and TRANSCEND (Telmisartan Randomized Assessment Study in ACE Intolerant Subjects With Cardiovascular Disease) - are reliable There were no differences in the incidence of new cases of AF when taking ACEIs or ARBs [19–22]. Despite the conflicting results of the studies performed, differences in the effectiveness of the treatments can be explained by significant changes in the sample of patients and comparators. Thus, the LIFE and VALUE studies used ARBs, and the CAPP and STOP-2 studies assessed the effectiveness of ACE inhibitors. The LIFE study included patients with hypertension and left ventricular hypertrophy (LVH), while the CAPP, STOP-2, HOPE and TRANSCEND studies were conducted in the general population of patients. Apparently, the low protective effect of ACE inhibitors during primary prevention of AF in the CAPP and STOP-2 studies could be associated with the lack of a treatment substrate in patients without LVH, since structural remodeling of the atria is most significant in severe LVH. Thus, the prescription of ACE inhibitors and ARBs for primary prevention of AF is most justified in hypertensive patients with LVH. The antiarrhythmic effect of these drugs depends on the severity of organic changes in the myocardium and is mediated by their organoprotective properties. Heart failure. The effectiveness of ACEIs and ARBs in the secondary prevention of AF in patients with CHF was demonstrated in three randomized clinical trials: SOLVD (Studies of Left Ventricular Dysfunction), CHARM (Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity) and Val-HeFT (Valsartan Heart Failure Trial) [23–25]. The SOLVD study assessed the effectiveness of enalapril treatment in patients with low left ventricular ejection fraction (LVEF). After 3 years of follow-up, the number of new cases of AF in patients receiving enalapril was more than 4 times lower compared to the placebo group. In addition, a relationship was found between the reduction in the relative risk of AF and LVEF [23]. The results of the CHARM and Val-HeFT studies demonstrated a significant reduction in new cases of AF when treated with candesartan and valsartan. All three studies using ACEIs or ARBs in patients with CHF showed a reduction in the relative risk of new incident AF by approximately 44%, which allows the use of these drugs to be recommended as preventive treatment for the primary prevention of AF [23–25]. Previous myocardial infarction. Only 2 studies have been conducted using ACE inhibitors in patients who have suffered acute MI. The results of the observations turned out to be diametrically opposite. The GISSI-3 study (Gruppo Italiano per lo Studio Della Sopravvivenza Nell'Infarto Miocardico-3) did not reveal a statistically significant reduction in the likelihood of AF within 6 weeks. after acute MI using lisinopril therapy [26]. The TRACE (Trandolapril Cardiac Evaluation) study showed a significant reduction in the likelihood of developing AF over 4 years when patients were treated with trandolapril from the first week after MI [27]. It should be noted that the TRACE study included patients with reduced LVEF, while in the GISSI-3 study, 83% of patients did not have heart failure. It is likely that the use of ACE inhibitors and ARBs for the prevention of AF is primarily justified in patients with CHF, since the appearance of inotropic dysfunction of the LV myocardium significantly increases the risk of developing arrhythmia. Secondary prevention of AF The effectiveness of ACE inhibitors and ARBs in secondary prevention of AF was assessed in patients with persistent AF after cardioversion. As a result, seven studies (out of eight) showed a statistically significant reduction in the risk of AF paroxysms during treatment with ACE inhibitors or ARBs, and these effects persisted for weeks after cardioversion. Most patients included in the studies had hypertension or CHF. Madrid A H et al. (2002, 2004) studied the effectiveness of administering irbesartan in addition to amiodarone. Patients receiving irbesartan had a significantly lower number of AF paroxysms when compared with the control group [28,29]. Ueng et al. (2003) showed that the appointment of enalapril to standard antiarrhythmic therapy with amiodarone significantly reduces the frequency of AF paroxysms in patients after electrical cardioversion [30]. In Van den Berg et al. (1995) it was proven that the administration of lisinopril together with amiodarone significantly reduces the risk of repeated paroxysms of AF in patients with CHF [31]. The effectiveness of ACE inhibitors in secondary prevention of AF was also demonstrated in studies by Grecu et al. (2007) and Belluzzi et al. (2009) [32,33]. Studies have shown that the appointment of ACE inhibitors to standard antiarrhythmic therapy makes it possible to maintain sinus rhythm significantly longer in patients with persistent AF after cardioversion. Tveit et al. (2007) examined the effectiveness of secondary prevention of AF when taking candesartan. Patients receiving ARBs had significantly fewer episodes of AF when compared with placebo [34]. The results of the randomized clinical trial GISSI-AF (Gruppo Italiano per lo Studio della Sopravvivenza nell'Infarto Miocardico - Atrial Fibrillation) showed that taking valsartan at a dose of 320 mg/day. in addition to standard antiarrhythmic therapy does not prevent recurrence of AF during 1 year of follow-up [35]. The results of the study can be called contradictory, since patients in the control group were allowed to take ACE inhibitors, which could reduce the frequency of AF paroxysms in this group. Thus, the GISSI-AF study did not find a significant difference in the frequency of AF attacks when taking ACEIs and ARBs. In a study by Yin et al. (2006) [36] and three papers by Fogari et al. (2006, 2008) demonstrated the antiarrhythmic effect of ACE inhibitors and ARBs in patients with paroxysmal AF [37–39]. The authors showed that the use of drugs that block the RAAS significantly reduces the frequency of relapses of AF and the need for taking loading doses of antiarrhythmic drugs. Currently, there is insufficient evidence to definitively recommend the use of ACEIs and ARBs exclusively for the prevention of AF. The antiarrhythmic effects of drugs in these groups are most obvious in patients with risk factors for AF: hypertension, LVH, or CHF. The results of clinical studies have demonstrated the effectiveness of ACEIs and ARBs in both primary and secondary prevention of AF, due to their ability to prevent the development of structural and electrophysiological remodeling of the atria. The study of the role of the RAAS in the pathogenesis of AF is the most pressing issue in modern cardiology.
References 1. Fuster V., Ryden LE et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation – executive summary // Eur. Heart. J. 2006, Vol. 27, R. 1979–2030. 2. Stevenson WG, Stevenson LW Atrial fibrillation and heart failure–five more years. // N. Engl. J. Med. 2004, Dec 2, Vol. 351(23). R. 2437–2440. 3. Iravanian S., Dudley SC The Renin–Angiotensin–Aldosterone System (RAAS) and Cardiac Arrhythmias // Heart Rhythm. 2008 June; 5(6 Suppl. 1): S.12–17. 4. Cha TJ, Ehrlich JR, Zhang L., Nattel S. Atrial ionic remodeling induced by atrial tachycardia in the presence of congestive heart failure. // Circulation. 2004, Sep 21, Vol. 110(12). R. 1520–1526. 5. Yue L., Feng J., Gaspo R., Li GR, Wang Z., Nattel S. Ionic remodeling underlying action potential changes in a canine model of atrial fibrillation. // Circ. Res., 1997, Vol. 815. P. 12–25. 6. Li D., Karen S., Leung TK, Nattel S. Promotion of atrial fibrillation by heart failure in dogs: atrial remodeling of a different sort. // Circulation. 1999, Vol. 100. R. 87–95. 7. Gronefeld GC, Hohnloser SH Heart failure complicated by atrial fibrillation: mechanistic, prognostic, and therapeutic implications. // J. Cardiovasc. Pharmacol. Ther., 2003, Jun; Vol. 8(2). R. 107–113. 8. Kostin S., Klein G., Szalay Z., Hein S., Bauer EP, Schaper J. Structural correlate of atrial fibrillation in human patients. // Cardiovasc Res. May 2002; Vol. 54(2). R. 361–379. 9. Boldt A., Wetzel U., Weigl J. et al. Expression of angiotensin II receptors in human left and right atrial tissue in atrial fibrillation with and without underlying mitral valve disease. // J Am Coll Cardiol. 2003;42:1785–1792. 10. Goette A., Arndt M., Rocken C. et al. Regulation of angiotensin II receptor subtypes during atrial fibrillation in humans. // Circulation. 2000;101:2678–2681. 11. Oudot A., Vergely C., Ecarnot–Laubriet A. et al. Angiotensin II activates NADPH oxidase in isolated rat hearts subject to ischaemia–reperfusion. // Eur J Pharmacol. 2003;462:145–154. 12. Kaibara M., Mitarai S., Yano K. et al. Involvement of Na+–H+ antiporter in regulation of L–type Ca2+ channel current by angiotensin II in rabbit ventricular myocytes. // Circ Res. 1994;75:1121–1125. 13. Benitah JP, Vassort G. Aldosterone upregulates Ca2+ current in adult rat cardiomyocytes. // Circ Res. 1999;85:1139–1145. 14. Shang LL, Sanyal S, Pfahnl AE et al. NF–B–dependent transcriptional regulation of the cardiac scn5a sodium channel by angiotensin II. Am J Physiol Cell Physiol. 2008;294:C372–92007. 15. Kasi VS, Xiao HD, Shang LL et al. Cardiac–restricted angiotensin–converting enzyme overexpression causes conduction defects and connexin dysregulation. // Am J Physiol Heart Circ Physiol. 2007;293:H182–H192. 16. Schneider MP, Tsushung A., Bohm M. et al. Prevention of Atrial Fibrillation by Renin–Angiotensin System Inhibition // Journal of the American College of Cardiology. 2010; 55:2299–307. 17. Wachtell K., Lehto M., Gerdts E. et al. Angiotensin II receptor blockade reduces new–onset atrial fibrillation and subsequent stroke compared to atenolol: the Losartan Intervention for End Point Reduction in Hypertension (LIFE) study. // J Am Coll Cardiol. 2005, 45:712–9. 18. Schmieder RE, Kjeldsen SE, Julius S., McInnes GT, Zanchetti A., Hua TA Reduced incidence of new–onset atrial fibrillation with angiotensin II receptor blockade: the VALUE trial. // J Hypertens. 2008;26:403–11. 19. Hansson L., Lindholm L.H., Niskanen L. et al. Effect of angiotensin converting–enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPPP) randomized trial. // Lancet. 1999;353:611–6. 20. Hansson L., Lindholm L.H., Ekbom T. et al. Randomized trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients With Hypertension–2 study. // Lancet. 1999;354:1751–6. 21. Salehian O., Healey J., Stambler B. et al. Impact of ramipril on the incidence of atrial fibrillation: results of the Heart Outcomes Prevention Evaluation study. // Am Heart J. 2007;154:448–53. 22. Yusuf S., Teo K., Anderson C. et al. Effects of the angiotensin–receptor blocker telmisartan on cardiovascular events in high–risk patients intolerant to angiotensin–converting enzyme inhibitors: a randomized controlled trial. // Lancet. 2008;372:1174–83. 23. Vermes E, Tardif JC, Bourassa MG et al. Enalapril decreases the incidence of atrial fibrillation in patients with left ventricular dysfunction: insight from the Studies of Left Ventricular Dysfunction (SOLVD) trials. // Circulation 2003;107:2926–31. 24. Ducharme A., Swedberg K., Pfeffer MA et al. Prevention of atrial fibrillation in patients with symptomatic chronic heart failure by candesartan in the Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity (CHARM) program. // Am Heart J. 2006;152:86–92. 25. Maggioni AP, Latini R, Carson PE et al. Valsartan reduces the incidence of atrial fibrillation in patients with heart failure: results from the Valsartan Heart Failure Trial (Val–HeFT). // Am Heart J. 2005;149:548–57. 26. Pizzetti F., Turazza FM, Franzosi MG et al. Incidence and prognostic significance of atrial fibrillation in acute myocardial infarction: the GISSI–3 data. //Heart. 2001;86:527–32. 27. Pedersen OD, Bagger H., Kober L., Torp–Pedersen C. Trandolapril reduces the incidence of atrial fibrillation after acute myocardial infarction in patients with left ventricular dysfunction. // Circulation. 1999;100:376–80. 28. Madrid AH, Bueno MG, Rebollo JM et al. Use of irbesartan to maintain sinus rhythm in patients with long–lasting persistent atrial fibrillation: a prospective and randomized study. // Circulation. 2002;106:331–6. 29. Madrid AH, Marin IM, Cervantes CE et al. Prevention of recurrences in patients with single atrial fibrillation. The dose–dependent effect of angiotensin II receptor blockers. // J Renin Angiotensin Aldosterone Syst. 2004;5:114–20. 30. Ueng KC, Tsai TP, Yu WC et al. Use of enalapril to facilitate sinus rhythm maintenance after external cardioversion of long–standing persistent atrial fibrillation. Results of a prospective and controlled study. // Eur Heart J. 2003;24:2090–8. 31. Van den Berg MP, Crijns HJ, Van Veldhuisen DJ, Griep N., De Kam PJ, Lie KI Effects of lisinopril in patients with heart failure and chronic atrial fibrillation. // J Card Fail 1995;1:355–63. 32. Grecu M., Olteanu RO, Olteanu SS, Georgescu CA Does treatment with ACE inhibitors prevent the long term recurrences of single atrial fibrillation after cardioversion? // Rom J Intern Med. 2007;45:29–33. 33. Belluzzi F., Sernesi L., Preti P., Salinaro F., Fonte ML, Perlini S. Prevention of recurrent lone atrial fibrillation by the angiotensin–II converting enzyme inhibitor ramipril in normotensive patients. // J Am Coll Cardiol. 2009;53:24–9. 34. Tveit A., Grundvold I., Olufsen M. et al. Candesartan in the prevention of relapsing atrial fibrillation. // Int J Cardiol. 2007;120:85–91. 35. Disertori M., Latini R., Barlera S. et al. Valsartan for prevention of recurrent atrial fibrillation. // N Engl J Med. 2009;360:1606–17. 36. Yin Y., Dalal D., Liu Z. et al. Prospective randomized study comparing amiodarone vs. amiodarone plus losartan vs. amiodarone plus perindopril for the prevention of atrial fibrillation recurrence in patients with lone paroxysmal atrial fibrillation. // Eur Heart J 2006;27:1841–6. 37. Fogari R., Derosa G., Ferrari I. et al. Effect of valsartan and ramipril on atrial fibrillation recurrence and P–wave dispersion in hypertensive patients with recurrent symptomatic lone atrial fibrillation. // Am J Hypertens. 2008;21:1034–9. 38. Fogari R., Mugellini A., Destro M. et al. Losartan and prevention of atrial fibrillation recurrence in hypertensive patients. // J Cardiovasc Pharmacol. 2006;47:46–50. 39. Fogari R., Zoppi A., Mugellini A. et al. Comparative evaluation of effect of valsartan/amlodipine and atenolol/amlodipine combinations on atrial fibrillation recurrence in hypertensive patients with type 2 diabetes mellitus. // J Cardiovasc Pharmacol. 2008;51:217–22.
Mechanism of operation
Due to a decrease in blood pressure in the juxtaglomerular cells of the nephron, the proteolytic enzyme renin begins to be released, which is a hormone-like substance. Under the influence of renin, the decapeptide angiotensin I is cleaved from the protein α 2 -globulin fraction of the blood - angiotensinogen, through limited proteolysis, which is converted into angiotensin II under the influence of angiotensin-converting factor (ACE). Angiotensin II, in turn, exhibits a vasoconstrictor effect and stimulates the release of aldosterone by the adrenal cortex, under the influence of which the reabsorption of sodium and water ions in the distal nephron increases, which leads to an increase in circulating blood volume (CBV).
Due to the increase in blood volume and the direct vasoconstrictive effect of angiotensin II, blood pressure increases.