Composition and dosage forms
The drug is available in the form of tablets for oral administration: white or cream-colored, biconvex, with a characteristic medicinal odor. Dosage of the active component: 50 and 150 mg.
The active ingredient of the drug is tolperisone hydrochloride, which has a relaxing effect on the fibers of muscle tissue. Each tablet, in addition to the active component, contains auxiliary and formative components:
- lactose;
- lemon acid;
- stearic acid;
- crospovidone.
The drug shell contains: talc, titanium dioxide, polyvinyl chloride and other components.
Conclusion
1. When choosing tactics for conservative treatment of patients with the initial stages of coxarthrosis, one should distinguish the category of patients with a predominance in the clinical picture of an exacerbation phase of the arthritic type, characterized by persistent synovitis and inflammatory laboratory changes.
2. Adding the oral drug Mydocalm in a daily dosage of 150 mg to the complex conservative treatment regimen reliably allows for an early clinical effect.
3. The centrally acting muscle relaxant tolperisone (Mydocalm), having an n-cholinolytic effect, has a pronounced positive pathogenetic effect on the symptoms and progression of OA.
4. It is recommended to include tolperisone (Mydocalm) in regulatory documents for the treatment of patients with OA of large joints.
Mechanism of action of the drug Tolperisone
The drug selectively inhibits the activity of parts of the brain responsible for regulating the motor functions of muscles. It has a central anticholinergic effect, has a slight antispasmodic effect, expands the lumen and reduces vascular tone. Tolperisone does not affect the activity of the peripheral nervous system.
The drug tablets dissolve and are absorbed into the blood in the gastrointestinal tract. Their active component has a bioavailability of about 20%. The effect of the medicine begins 20–30 minutes after administration, reaching a maximum within 1–1.5 hours. The effect lasts 4–5 hours. The medication does not accumulate in the body. All its substances are transformed in the liver. Metabolites are excreted through the kidneys in the urine within 6–8 hours.
For what diseases is Tolperisone indicated?
It is recommended to use the drug in the following conditions:
- increased tone, muscle spasms;
- spastic contractures of the limbs;
- cerebral palsy;
- dysfunction of the spinal cord;
- rigidity, muscle dystonia;
- obliterating sclerosis of the extremities;
- Raynaud's syndrome;
- diabetic angiopathy, thromboangiitis and other manifestations of arterial damage;
- Parkinson's disease;
- acrocyanosis, dysbasia, other painful conditions caused by disorders of vascular innervation;
- disturbances of venous circulation and lymph movement in conditions after thrombosis;
- vascular encephalopathy;
- infantile spastic paralysis;
- trophic ulcers of the lower extremities;
- epilepsy.
The medication is approved for use from the age of 1 year.
Introduction
Osteoarthritis (OA) is a heterogeneous group of diseases of various etiologies with similar biological, morphological, clinical manifestations, which are based on damage to all components of the joint, primarily cartilage, as well as subchondral bone, synovial membrane, ligaments, capsule, periarticular muscles [1] . The disease is an important medical, social and economic problem due to its widespread prevalence (6.43% in the population, correlates with age and reaches maximum values of 13.6% in people over 45 years old), a significant deterioration in the quality of life of patients due to constant pain syndrome, as well as high disability [2].
Despite the high negative significance of this pathology, modern regulatory documents on the provision of specialized care for OA have not been developed. The existing standard of care for patients with coxarthrosis from 2005 is recommended for use in federal specialized medical institutions [3], and the relatively modern standard from 2012 regulates exclusively primary health care provided on an outpatient basis [4]. Both orders include only symptomatic drugs, while etiopathogenetic therapy is not indicated. Therefore, practicing doctors use clinical recommendations and treatment protocols for patients with OA in their work [5]. According to these documents, a generally accepted treatment regimen involves 3 successive stages [6, 7]:
1) non-pharmacological methods: lifestyle changes, excess weight loss, physical exercise, use of orthopedic products, physiotherapeutic and spa treatment;
2) drug therapy: NSAIDs, non-selective COX-2 inhibitors (paracetamol, diclofenac, ibuprofen, ketoprofen, naproxen), moderately selective COX-2 inhibitors (meloxicam, nimesulide, aceclofenac), selective COX-2 inhibitors (celecoxib, etoricoxib), opioid analgesics (tramadol) if NSAIDs are ineffective, intra-articular administration of corticosteroids (methylprednisolone or triamcinolone), chondroprotectors (chondroitin sulfate, glucosamine sulfate, hyaluronic acid derivatives), interleukin 1 inhibitor - diacerein, unsaponifiable compounds of avocado and soy (NSAC) - piaskledin;
3) surgical treatment - endoprosthetics.
The first nonspecific symptoms of OA (pain, limited range of motion) appear even in the absence of radiological changes in the joint and are most likely caused by muscle spasm. However, in most domestic clinical recommendations there is no such class of drugs as centrally acting muscle relaxants, while the Kazakhstan Protocol for the Treatment of OA (2013) contains such drugs [8]. The inclusion of centrally acting muscle relaxants in the complex conservative treatment regimen for OA of large joints, especially in the initial stages of the pathology, seems to be pathogenetically justified and an appropriate addition to the generally accepted treatment regimen.
The purpose of the study was to compare the effectiveness of the generally accepted regimen of conservative drug therapy for hip OA (NSAIDs + chondroprotectors) and a modified regimen (NSAIDs + chondroprotectors + centrally acting muscle relaxant - tolperisone).
When is Tolperisone contraindicated?
It is necessary to refuse treatment with the drug during pregnancy and lactation. There is not enough information about the effect of the active substance on fetal formation. The systemic effect that it causes can affect the condition of both mother and child and cause irreversible disorders.
Other contraindications for use:
- myasthenia gravis;
- individual hypersensitivity to the components of the drug;
Signs of a possible allergic reaction to Tolperisone: bronchospasm, skin itching, urticaria, the appearance of red spots - erythema, anaphylactic shock, Quincke's edema.
Results and discussion
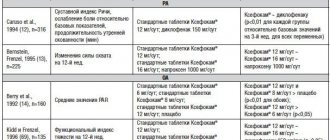
Upon admission, patients in both groups had the following levels of the studied criteria (Tables 2, 3).
Table 2. Clinical indicators of the studied criteria at admission
Table 3. Paraclinical and laboratory indicators of the studied criteria upon admission
As can be seen from table. 2 and 3, no significant, statistically significant differences in the studied criteria were found in the groups of patients.
The dynamics of therapy effectiveness criteria in the comparison group are presented in Fig. 1.
Rice. 1. Dynamics of the studied criteria for the effectiveness of treatment in the comparison group.
In the majority of patients in the comparison group ( n
=34) the increase in the amplitude of flexion, extension and rotation of the hip had a statistically significant increase (11±30;
p
<0.05).
The VAS pain index value decreased by more than 20 mm ( p
<0.01). At the same time, the severity of synovitis and laboratory criteria also had positive dynamics, but did not always have statistical confirmation (Table 4).
Table 4. Dynamics of clinical and laboratory criteria for the effectiveness of therapy in the comparison group
Thus, by the end of observation in this group of patients, all studied criteria had positive dynamics compared to the initial values: the amplitude of hip movements and the severity of pain showed statistically significant changes, and changes in the severity synovitis and laboratory parameters were unreliable.
The changes in the studied data in the main observation group looked somewhat different (Fig. 2).
Rice. 2. Dynamics of the studied criteria for the effectiveness of treatment in the main observation group.
In the main group, the same trends were observed as in the comparison group: most significant and reliable ( p
<0.01) the intensity of the pain syndrome on the VAS scale decreased - minus 33 mm, in addition,
the amplitude of all hip movements increased p The severity of synovitis and laboratory criteria also had positive, statistically insignificant dynamics (Table 5).
Table 5. Dynamics of clinical and laboratory criteria for the effectiveness of therapy in the main group
Thus, the differences between the groups consisted primarily in more reliable and pronounced clinical (the amplitude of hip movements increased: 11±30 at p<0.05 in the comparison group and 14± 20 at p
<0.01 in the main group) and subjectively stated paraclinical (pain intensity on the VAS scale decreased by 21 mm in the first group and by 33 mm in the second,
p
<0.01) effects of therapy (Fig. 3, 4).
Rice. 3. Dynamics of the amplitude of hip movements in the control and main groups upon admission and on the 12th day of therapy.
Rice. 4. Dynamics of VAS in the control and main groups upon admission and on the 12th day of therapy.
Side effects of the drug
During treatment with Tolperisone tablets, the following may appear:
- muscle weakness;
- dyspnea;
- increased fatigue;
- dizziness;
- drowsiness during the daytime;
- decreased blood pressure;
- pain in the stomach and abdominal cavity;
- nausea, vomiting.
In the absence of a serious threat to the physical condition, such symptoms do not require discontinuation of the drug.
Use of Tolperisone: instructions
The treatment regimen depends on the characteristics of the painful manifestations. General recommendations:
- 1 tablet with a dosage of 50 mg. 2–3 times a day for adults in the first days of therapy;
- 150 mg each. up to three times a day - if the drug is well tolerated in the subsequent period.
For children under 15 years of age, the dosage is selected taking into account body weight:
- 2–4 mg per 1 kg of weight: children from 1 to 6 years old;
- 5 mg per 1 kg. weight: from 7 to 14 years.
The time of eating does not affect the absorption of the drug.
An overdose of the drug is fraught with respiratory problems, cardiac depression, and vascular collapse. It is important to use it strictly as prescribed by the doctor, after carefully studying the instructions. After taking each dose, monitor changes in physical condition.
Buy Tolperisone-OBL film-coated tablets 150 mg No. 30 in pharmacies
MANUFACTURERS Obolensk Pharmaceutical Enterprise (Russia) GROUP Centrally acting muscle relaxants
COMPOSITION The active substance is tolperisone.
INTERNATIONAL NON-PROPENTED NAME Tolperisone
SYNONYMS Mydocalm
PHARMACOLOGICAL ACTION Muscle relaxant with a central mechanism of action. It has a membrane-stabilizing effect, inhibits the conduction of nerve impulses in primary afferent fibers and motor neurons, which leads to blocking of spinal mono- and polysynaptic reflexes. Probably mediates blocking the release of mediators by inhibiting the entry of Ca+2 into synapses. Inhibits the conduction of excitation along the reticulospinal tract in the brain stem. Regardless of the influence of the central nervous system, it increases peripheral blood flow. The weak antispasmodic and antiadrenergic effect of tolperisone may play a role in the development of this effect. After oral administration, tolperisone is well absorbed from the small intestine. The maximum concentration in the blood plasma is achieved 30 minutes-1 hour after administration; bioavailability due to pronounced first-pass metabolism is about 20%. Tolperisone is extensively metabolized in the liver and kidneys. Excreted in urine almost exclusively (more than 99%) in the form of metabolites. The pharmacological activity of the metabolites is unknown.
INDICATIONS FOR USE Treatment of pathologically increased tone and spasms of striated muscles caused by organic neurological pathology (including damage to the pyramidal tracts, multiple sclerosis, stroke, myelopathy, encephalomyelitis). Treatment of increased tone and muscle spasms, muscle contractures accompanying diseases of the musculoskeletal system (spondylosis, spondyloarthrosis, arthrosis of large joints, cervical and lumbar pain syndromes). Rehabilitation treatment after surgical interventions in orthopedics and traumatology. As part of combination therapy for obliterating vascular diseases (obliterating atherosclerosis, diabetic angiopathy, thromboangiitis obliterans, Raynaud's disease), as well as diseases resulting from impaired vascular innervation (acrocyanosis, intermittent angioedema).
CONTRAINDICATIONS Myasthenia gravis, age under 18 years, hypersensitivity to the components of the drug, pregnancy, lactation. Due to the presence of lactose, patients with lactose intolerance, lactase deficiency or glucose-galactose malabsorption should not take the drug.
SIDE EFFECTS: Muscle weakness, headache, arterial hypotension, nausea, vomiting, gastralgia (usually resolves with dose reduction), rarely - hypersensitivity reactions (itching, erythema, urticaria, angioedema, bronchospasm, anaphylactic shock).
INTERACTION Tolperisone has an effect on the central nervous system, but does not cause a sedative effect, therefore it can be used in combination with sedatives, hypnotics, and tranquilizers. Does not enhance the effect of alcohol on the central nervous system. Increases the severity of the action of niflumic acid, so when used simultaneously, the dose of the latter can be reduced. Medicines for general anesthesia, peripheral muscle relaxants, psychoactive drugs, clonidine enhance the effect.
METHOD OF APPLICATION AND DOSAGE Orally. For adults, the initial dose is 50 mg 2-3 times a day, with a gradual increase to 150 mg 2-3 times a day. The duration of treatment depends on the severity and nature of the disease.
OVERDOSE Symptoms: respiratory and cardiac depression, decreased blood pressure. Treatment: symptomatic.
SPECIAL INSTRUCTIONS During the treatment period, care must be taken when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
STORAGE CONDITIONS List B. In a dry place, protected from light, at a temperature not exceeding 25 degrees C. Keep out of the reach of children!
special instructions
The therapeutic effect of the drug is enhanced and prolonged when combined with peripheral muscle relaxants, Clonidine, psychoactive and anesthetic agents. Tolperisone reduces the speed of motor skills and mental reactions, affects concentration. During the treatment period, it is necessary to refrain from driving and working with complex mechanisms.
The combination of the drug with alcohol is unacceptable, as it leads to serious intoxication, a sharp decrease in vascular tone, and damage to the central nervous system.