Vaginitis is an inflammation of the vaginal mucosa caused by disruption of the normal flora of the genital organs, the entry of pathogenic viruses and bacteria into it, as well as insufficient intimate hygiene or allergies to cosmetics and contraceptives. Acute vaginitis causes a list of unpleasant symptoms that impair quality of life and interfere with healthy sexual relationships. With a prolonged course of the inflammatory process in the vagina, with insufficient or incorrect treatment, vaginitis can develop into a chronic stage, which is fraught with serious complications for the woman’s reproductive system.
Causes and risk factors of the disease
In the clinic, a distinction is made between the concepts of “specific” and “nonspecific” inflammation of the vaginal mucosa. The first group occurs after certain bacteria enter the genital tract, causing a characteristic clinical picture and requiring a certain type of treatment. The most common specific vaginitis is caused by:
- trichomonas;
- gonococci;
- mycoplasma;
- ureaplasma;
- fungi of the genus “Candida”;
- chlamydia;
- herpes and human papilloma viruses.
All these infections are included in the group of sexually transmitted diseases. Infection of the vagina occurs during sexual intercourse from an infected partner (clinically he may be healthy).
A nonspecific process occurs due to the activation of opportunistic vaginal flora, which is present in the genital tract of every woman without causing any clinical symptoms. This flora includes staphylococci, streptococci, Haemophilus influenzae, Escherichia coli and other bacteria. They can cause clinical vaginitis in certain conditions that are risk factors:
- with mechanical damage to the vaginal mucosa (due to surgical interventions, childbirth, abortion);
- uncontrolled use of antibiotics, suppressing the normal flora of the vagina;
- insufficient blood supply to the vaginal mucosa, which is an age-related characteristic of the body (atrophic vaginitis);
- hormonal imbalance in diseases of the ovaries, adrenal glands, menopause;
- allergies to condoms, intimate gels and creams, tampons or suppositories;
- failure to maintain personal hygiene.
Vaginitis is an inflammation of the vaginal mucosa. This disease is very common and is one of the main reasons why women turn to a gynecologist. It can be either infectious or non-infectious in nature. The most common are bacterial vaginosis, thrush and trichomonas vaginitis, after menopause - atrophic vaginitis.
Treatment depends on the immediate cause of vaginitis. In general, the prognosis of the disease is favorable - in most cases it is completely curable. However, in the absence of timely measures, this disease can lead to a number of complications, such as inflammatory diseases of the pelvic organs, infertility, and premature birth. Vaginitis also increases the risk of contracting sexually transmitted infections.
Synonyms Russian
Colpitis, bacterial vaginosis, vulvovaginitis.
English synonyms
Vaginal infections, vaginitis, bacterial vaginosis, vulvovaginitis.
Symptoms
- Changes in color, smell, consistency, amount of vaginal discharge.
- Itching, burning in the genital area.
- Pain, burning, discomfort during urination and/or sexual intercourse.
A woman may have all of these symptoms at the same time, or only some of them. Symptoms of vaginitis may worsen during menstruation or after sexual intercourse.
Although the symptoms are similar for all types of vaginitis, some signs, such as the color and smell of the discharge, may differ depending on the cause of the disease.
General information about the disease
The vagina of a healthy woman contains a certain composition of microorganisms. The majority of them are lactobacilli (Doderlein bacilli, lactic acid bacteria). They participate in maintaining normal vaginal microflora and protect it from infection. Under the influence of female sex hormones, the polysaccharide glycogen is synthesized in the cells of the vaginal mucosa, from which lactic acid is formed with the help of lactobacilli. Thanks to lactic acid, an acidic environment is maintained, which prevents infection and proliferation of microorganisms that may be present in small quantities in the vagina of a healthy woman, but do not lead to disease.
In women of childbearing age, the cells of the vaginal mucosa produce a small amount of secretion. Normally, vaginal discharge is white and has a neutral odor. On certain days of the menstrual cycle, as well as under stress, the amount of discharge may increase.
Vaginitis occurs when the normal microflora of the vagina is disrupted and the balance between normal and pathogenic microorganisms changes. The cause of these changes may be the use of antibacterial or hormonal drugs, the use of oral contraceptives, stress, sexually transmitted diseases, change of sexual partner, diseases of other organs and systems, such as diabetes, hormonal changes during pregnancy or menopause, trauma to the vaginal mucosa . Exposure to chemicals, for example when using vaginal sprays, spermicides, can lead to an allergic reaction, irritation of the mucous membranes and non-infectious vaginitis. Atrophic vaginitis occurs during menopause due to a deficiency of female sex hormones. This leads to thinning, dryness, and irritation of the vaginal mucosa, which makes it easier for infection to penetrate.
The most common types of vaginitis are:
- Bacterial vaginosis. Accounts for 40-50% of all cases of vaginitis. With it, lactobacilli are replaced by other microorganisms (Prevotella, Gardnerella vaginalis, Mycoplasma hominis). In many women it is asymptomatic. The main signs of the disease are copious grayish discharge with an unpleasant odor, pain and burning when urinating.
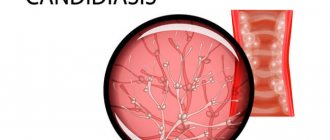
- Thrush (or vaginal candidiasis). Accounts for 20-25% of cases of vaginitis. Caused by microscopic fungi of the genus Candida. During their lifetime, 3 out of 4 women will experience symptoms of vaginal candidiasis at least once. Women are most susceptible to this disease during stress, pregnancy, and when taking antibiotics and other medications. Women with diabetes or HIV infection are prone to recurring episodes of vaginal candidiasis. The most characteristic symptoms of thrush are a white, cheesy vaginal discharge and itching in the genital area.
- Trichomonas vaginitis (trichomoniasis). Accounts for 15-20% of cases of vaginitis. Caused by the simplest single-celled microorganism Trichomonas vaginalis. It is transmitted sexually and affects the vagina, cervix and urethra, and also increases the risk of premature birth in pregnant women. With trichomonas vaginitis, the discharge has a greenish-yellow color and an unpleasant odor.
Who is at risk?
- Pregnant women.
- Women after menopause.
- Women who have multiple sexual partners.
- Women suffering from sexually transmitted infections.
- Women using oral contraceptives.
Diagnostics
If you have symptoms of vaginitis, you must consult a doctor who, after interviewing the patient, a gynecological examination and a number of additional laboratory and instrumental studies, will be able to determine the cause of the disease and prescribe effective treatment.
Laboratory diagnostics
- Microscopic examination of discharge from the genitourinary organs of women (microflora), 3 localizations. This is one of the main methods for detecting vaginitis. A sample of the material is examined under a microscope after preliminary staining with special dyes or without it. Allows you to identify signs of inflammation and detect the pathogen that caused the disease.
- Study of vaginal microbiocenosis with determination of sensitivity to antibiotics. The vaginal discharge is inoculated onto a specific nutrient medium, which makes it possible to detect even a small amount of the pathogen in the material. For vaginitis, a culture for mycoplasma, ureaplasma, chlamydia, Candida fungi, and trichomonas may be prescribed.
- Cytological examination of smears and scrapings from the surface of the cervix and external uterine pharynx - Papanicolaou staining (Pap test). This is a study of cells in the vagina and cervix to identify atypical, malignant cells. Necessary for diagnosing changes that precede cervical cancer. It is mandatory for women over 30 years of age and for women infected with certain types of human papillomavirus.
- Determination of specific immunoglobulins for pathogens of urogenital infections. It is carried out by enzyme-linked immunosorbent assay (ELISA). Allows you to identify antibodies (immunoglobulins) to certain infections - specific proteins that are produced in the body in response to the penetration of a microorganism. In this way, antibodies to yeast-like fungi, ureaplasma, and Trichomonas can be detected.
- Determination of the genetic material of the infectious agent in a woman’s vaginal discharge using the polymerase chain reaction (PCR) method. The DNA of chlamydia, mycoplasma, gardnerella and other pathogens is detected.
Other research methods
- Vaginal pH measurement. This is a study of the acid-base balance of the vagina. Normal vaginal pH is 3.8-4.2. To measure, use special indicator paper, which, upon contact with vaginal discharge, changes color depending on the pH level, or pH meters. With vaginitis, the pH may increase due to a decrease in the number of lactobacilli that form lactic acid.
- Aminotest. Used to diagnose bacterial vaginosis caused by Gardnerella vaginalis, it involves adding one or two drops of vaginal fluid to a 5-10 percent potassium hydroxide solution. The appearance of a fishy odor is a sign of gardnerellosis.
- Colposcopy. This is an examination of the vaginal walls using a special colposcope equipped with an optical system and a light source. Allows you to assess the condition of the vaginal mucosa, identify damage or neoplasms, and also perform a biopsy, that is, take a sample of tissue from the mucous membrane for subsequent microscopic examination.
If a patient is diagnosed with trichomonas vaginitis, the doctor may additionally prescribe tests for other sexually transmitted diseases. Sometimes additional studies are carried out to assess a woman’s hormonal levels.
Treatment
Treatment depends on the cause of vaginitis. Medicines can be used both in the form of suppositories, gels, ointments, and in the form of tablets or injections. The choice of drug, dose, and method of administration depend on the cause of vaginitis, the severity and duration of the disease, the presence of concomitant diseases and conditions. For example, antibiotics are used for bacterial vaginosis, and antifungal drugs are used for thrush. For atrophic vaginitis, a good effect is achieved by taking estrogen in the form of creams or tablets.
Prevention
- Compliance with the rules of intimate hygiene.
- Use of barrier methods of contraception.
- Timely preventive gynecological examinations.
Recommended tests
- Microscopic examination of discharge from the genitourinary organs of women (microflora), 3 localizations
- Culture of flora with determination of sensitivity to antibiotics
- Culture for Mycoplasma hominis with determination of sensitivity to antibiotics (with a titer of 1x10^4 and higher)
- Culture for Ureaplasma species with determination of titer and sensitivity to antibiotics
- Culture of Candida spp./yeast-like fungi with selection of antimycotic drugs
- Culture for Chlamydia trachomatis with determination of sensitivity to antibiotics
- Culture for Trichomonas vaginalis
- Study of vaginal microbiocenosis with determination of sensitivity to antibiotics
- Analysis of vaginal microbiocenosis. 8 indicators, quantitative DNA [real-time PCR] (urogenital smear)
- Analysis of vaginal microbiocenosis. 16 indicators, quantitative DNA [real-time PCR] (urogenital smear)
- Cytological examination of smears and scrapings from the surface of the cervix and external uterine pharynx - Papanicolaou staining (Pap test)
- Mycoplasma hominis, IgA
- Mycoplasma hominis, IgG, titer
- Chlamydia trachomatis, IgA, titer
- Chlamydia trachomatis, IgG, titer
- Chlamydia trachomatis, IgM, titer
- Chlamydia trachomatis, DNA [real-time PCR] (urogenital smear, urine, ejaculate, prostate secretion)
- Ureaplasma species, DNA quantitatively [real-time PCR] (urogenital smear, urine, ejaculate, prostate secretion)
- Trichomonas vaginalis, DNA [real-time PCR] (urogenital smear, urine)
- Trichomonas vaginalis, IgG, titer
- Candida albicans, IgG, titer
- Histological examination of biopsy diagnostic material (endoscopic material, tissues of the female reproductive system, skin, soft tissues)
Types of vaginitis
According to the duration of the inflammatory process, it is divided into several types:
- acute vaginitis.
The inflammatory process develops quickly, more often after unprotected sexual intercourse; manifests itself with violent symptoms, but with a correctly prescribed treatment regimen, it is cured within two weeks;
- subacute vaginitis
– develops against the background of acute inflammation, in the absence of treatment or an incorrectly selected antibiotic therapy regimen. Symptoms become less severe, but continue to occur for more than two weeks;
- chronic vaginitis
diagnosed in cases where symptoms of inflammation persist for more than two months. It is also a consequence of improper treatment or, more often, the result of impaired immunity.
How is colpitis treated?
The treatment tactics are determined by the doctor at the Promedica clinic. It is based on diagnostic data and clinical picture. Typically, the patient undergoes medical treatment with antibacterial, antifungal and antimicrobial drugs, taking into account all indications and individual contraindications. You may also be prescribed symptomatic treatment.
After eliminating the causes of colpitis, it is necessary to restore the balance of the microflora.
If you have been diagnosed with specific vaginitis, then your sexual partner also needs to undergo treatment. To do this, he must also consult a doctor individually.
When treating chronic vaginitis, you may be prescribed physical therapy and taking vitamin and mineral complexes to improve immunity.
Gonorrheal vaginitis
Infectious vaginitis in women caused by gonococcus openly manifests itself in 50% of cases. In other women, the infection has a latent course. The incubation period ranges from 3 to 7 days, that is, the first symptoms after sexual contact with a partner may appear only after a week. The characteristic specific symptoms of the disease are as follows:
- purulent vaginal discharge that is white-yellow or greenish in color;
- severe pain, swelling and hyperemia of the mucous membrane. They are noticeable even without special examination;
- frequent false urge to urinate, resulting from gonorrheal inflammation of the urethra.
This species is characterized by the frequent transition of the disease to a chronic form, which is associated with the resistance of bacteria to common antibiotics.
Symptoms of vaginitis depending on the pathogen
The main signs of vaginal inflammation are general discomfort in the genital area, which manifests itself in irritation, tingling and burning. High temperature, pain in the vagina and general weakness are not characteristic symptoms; their presence indicates the neglect of the process.
Symptoms of vaginitis vary depending on the causative agent of the disease:
- bacterial is characterized by abundant purulent discharge of green or yellow color;
- Trichomonas is characterized by foamy discharge with an unpleasant strong odor, the patient complains of pain in the lower abdomen, in the absence of treatment the temperature can rise to 39°C;
- gonorrheal is manifested by pain, itching and mucous discharge mixed with pus or fragments of dead cells of the vaginal epithelium, and in an advanced form - with the presence of blood;
- Candida is characterized by a curd-like discharge with a sour odor and severe itching;
- atrophic vaginitis makes itself felt by unbearable itching, vaginal dryness, thinning of the vaginal epithelium, and frequent urination. Discharge is practically absent or may be bloody.
The most common type of inflammation is thrush. The disease does not go away on its own and requires complex treatment. For examination and diagnosis, you need to contact a gynecologist.
Trichomonas vaginitis
Sometimes the incubation period lasts up to one month. The absence of a regular sexual partner significantly complicates the search and elimination of the primary source of infection. The acute process is manifested by characteristic symptoms:
- Vaginal discharge: foamy, yellow, gray or greenish in color. A specific sign of infection is the presence of gas bubbles in the secreted secretion;
- the smell of discharge is sweetish and unpleasant;
- a constant burning sensation that gets worse after urination or during sex.
This type of vaginitis can become chronic. The reason for this is the fact that the overwhelming number of trichomonas vaginitis is caused by a mixed infection, for which it is difficult to choose the optimal antibiotic therapy regimen.
Candidal vaginitis
Among women, this type of vaginitis is the most common. Acute fungal inflammation is characterized by white discharge of a cheesy nature and has a sour odor. Itching, pain and irritation intensify after sex and thermal procedures, sometimes becoming unbearably painful.
Despite the known cause of the disease and a wide range of antifungal drugs, the pathogen is still resistant to treatment; then the disease enters the chronic stage, manifesting itself as unexpressed symptoms that intensify after sexual intercourse or during menstruation.
Atrophic vaginitis
The irreversible aging process of a woman’s body also affects the health of her external genitalia. With the onset of menopause, blood circulation in the vaginal mucosa significantly worsens. The number of feeding vessels is significantly reduced, in contrast to which an abundant capillary network develops as a compensatory mechanism. This leads to a complex of clinical symptoms called “atrophic vaginitis.” Its manifestations:
- decrease in vaginal secretion, manifested by pathological dryness of the genital tract and increased susceptibility to sexually transmitted infections;
- bleeding after sexual relations caused by damage to thin-walled capillaries located close to the surface of the vaginal mucosa;
- Dyspareunia is painful sexual intercourse caused by insufficient blood supply and deficiency of vaginal secretions.
Atrophic vaginitis has a slow, gradually progressive course. It is one of the signs marking the end of the reproductive period of a woman’s life.
Nonspecific vaginitis
Disturbance of the normal microflora of the vagina leads to the activation of opportunistic bacteria, which are present in the genital tract, but do not cause clinical symptoms. Features of this type of disease:
- the onset of the disease is characterized by the presence of one of the predisposing factors: childbirth, abortion, surgery, hormonal changes, etc.;
- vaginal discharge is liquid and watery, without pathological impurities or unpleasant odor. The latter can be added in cases of prolonged process, lack of treatment and insufficient hygiene;
- Nonspecific vaginitis is not characterized by pain and impairment of general condition. It occurs in the form of a local inflammatory process.
Diagnostics
The clinical picture and clarification of the disease history significantly simplify the laboratory diagnosis of the disease. The main diagnostic task is to find the causative agent in order to prescribe specific treatment later. There are three main methods for determining microorganisms:
- bacterioscopy – visualization of vaginal secretions under a multiple magnification microscope. The technique is widespread due to its practicality, ease of use and low cost. The disadvantage of the study is low specificity. In many cases, the method allows you to see microorganisms, but does not make it possible to accurately differentiate them;
- a bacteriological method known to many as “seeding”. Vaginal secretions are placed in special conditions on a nutrient medium where microorganisms grow. The procedure has a fairly high specificity, but it often takes up to 7 days to complete. In conditions of progressive disease, such a long wait-and-see approach is unacceptable;
- PCR is a highly informative diagnostic method that allows you to quickly identify the causative agent of the disease. Disadvantages - high cost. Conducting a blind study, simply identifying all the most common sexually transmitted infections, is not a cheap pleasure. The technique is justified by a competent approach, in which selective testing is carried out only for certain infections, justified by the clinical picture of the disease.
How will you be diagnosed with vaginal inflammation?
First, you need to make an appointment with a gynecologist at the Promedica clinic. The doctor will ask you questions and take a complete medical history. Afterwards, the specialist will conduct an examination on a gynecological chair, paying attention to the shade of the mucous membrane of the labia minora, the skin around the entrance to the vagina, and the presence of swelling. During the examination, the doctor will take swabs for:
- bacterioscopy;
- bacteriological culture;
- PCR studies;
- determination of PH (acidic environment of the vagina).
Treatment of vaginitis
Therapeutic tactics are determined by the gynecologist, based on the results of the clinical picture, objective examination and specific diagnostic methods.
From the point of view of selectivity, it is much easier to treat specific vaginitis, for which antibacterial, antifungal or antiviral agents are used, to which the pathogen is known to be sensitive.
The main means of treating specific vaginitis:
- trichomoniasis - drugs that are effective against single-cell microorganisms are used (metronidazole, tinidazole, ornidazole). For an acute form of the disease, a 7-day course of treatment is sufficient, for a chronic form – a 10-day course. The drugs can be taken as tablets or, more commonly, vaginal suppositories;
- gonococcal infection - use antibacterial drugs of the penicillin series, cephalosporins and fluoroquinolones (ceftriaxone, cefixime, penicillin, ofloxacin and others). The greatest effectiveness of treatment is observed with intravenous or intramuscular administration of drugs;
- chlamydia and mycoplasma infection - antibiotics of the doxycycline group, fluoroquinolones and macrolides (erythromycin, josamycin, levofloxacin, moxifloxacin). The course of treatment for uncomplicated forms of the disease does not exceed 10 days. The route of drug administration is oral;
- Candidiasis is effectively treated with antifungal drugs. In the acute form of the disease, fluconazole is prescribed at a dose of 150 mcg (1 tablet) once or two doses (200 mcg each) of itraconazole. Chronic and recurrent forms require a 7-day and sometimes two-week course of treatment.
A more difficult task is the treatment of nonspecific vaginitis, which should pursue the goals of exterminating pathogenic microorganisms and enriching the woman’s genital tract with benign bacteria. This often requires a long course of multicomponent therapy:
- drugs effective against anaerobic bacteria (metronidazole, tinidazole, ornidazole);
- antibiotics of the lincosamide group, covering a wide range of opportunistic microorganisms. Drugs such as clindamycin, dalacin and others can be prescribed in the form of tablets, suppositories and vaginal creams;
- antiseptics. An important component of the treatment of nonspecific vaginitis is intimate hygiene using antiseptic drugs. Chlorhexidine and other antiseptics can be used as vaginal suppositories or douches;
- vaginal suppositories containing “beneficial microorganisms”.
An additional component of the treatment of nonspecific vaginitis is the elimination of the “risk factor”. It includes vitamin therapy, correction of hormonal imbalances, taking antiallergic drugs, etc.
Prevention of colpitis
Both specific and nonspecific methods are used as preventive measures aimed at preventing vaginitis. From a young age, a girl should pay special attention to observing all the rules of personal hygiene. Washing must be carried out using soft hygiene products.
A girl should be taught from childhood to wash herself correctly: movements should be directed from front to back, so that infection does not spread to the genitals. Hygiene measures need to be significantly strengthened during menstruation. If a woman suspects a vaginal infection, she should immediately stop using tampons during menstruation.
Without a doubt, a necessary preventive measure is the absence of casual sex and the mandatory use of a condom.
To prevent weakening of the immune system, chronic diseases of internal organs and inflammation of the genital organs should be treated in a timely manner.
stress for a long time , or undergoes a long course of antibiotic treatment, she should definitely take lactobacilli preparations for some time to prevent changes in the vaginal microflora towards pathology.
An important preventative measure is hardening, as well as preventing a lack of vitamins in the body.
Complications
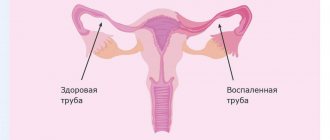
From the vagina, the infection along the ascending path can reach the cervix, into the uterus itself and cause infection of the tubes and ovaries. Late detection, inadequate treatment and lack of measures to prevent relapse can result in complications. The most common complications include:
- inflammation of the cervix, its inner lining and fallopian tubes. This group of complications is especially dangerous during pregnancy. Rising to the ovum, the infection can provoke miscarriage, premature birth, or due to infection of the amniotic fluid, severe pathology in the newborn. This complication can also cause postpartum endometritis, which, in severe cases, requires removal of the uterus;
- urinary tract infection. The urethra in women has a short, wide lumen and opens at the vestibule of the vagina. These factors contribute to the fairly easy penetration of bacteria into the cavity of the bladder, ureters and kidneys, causing inflammation of these organs;
- Severe cases of complicated vaginitis, if left untreated, result in bacteremia (“blood poisoning”) and a septic state. Mortality in such a situation exceeds the number of favorable outcomes of the disease.