Alcoholic hepatitis is part of a group of liver lesions not associated with infection. This type of inflammation, unlike viral hepatitis, is not transmitted from a patient to a healthy one, but is associated exclusively with prolonged alcohol consumption and the formation of alcohol dependence in a person. The disease is considered the main etiological cause of liver cirrhosis.
The prevalence of alcoholic hepatitis, according to statistical studies, in different countries is from 7 to 10 per 100 thousand population. An assessment of the health status of people who abuse alcohol allows us to conclude that 25–40% will develop liver inflammation within a few years, progressing to the stage of cell destruction and complete failure of this important organ.
The International Statistical Classification (ICD-10) identifies a group of diseases under the general term “alcoholic liver disease.” Among them, hepatitis is encoded by K70.1. The disease is most common among the male population aged 30 to 55 years.
The effect of alcohol on the liver
The breakdown of alcohol begins when it enters the human stomach. The juice constantly contains the enzyme alcohol dehydrogenase, which oxidizes up to 25% of the ingested ethanol and converts it into acetaldehyde. Thus, ¼ part is absorbed into the blood bypassing the liver. The presence of food (especially fatty foods) delays absorption, but does not neutralize toxic products.
The opposite effect is possible if the patient is taking medications from the group of H2-histamine receptor blockers. They reduce the concentration of alcohol dehydrogenase in the stomach and sharply increase the volume of ethanol entering the blood.
Alcohol is carried by the bloodstream to all organs, enters any fluids and tissues, causing significant damage to the functioning of cells.
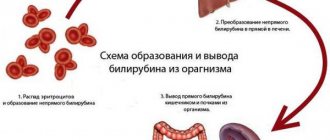
The enzymatic system of the liver enters the fight for neutralization due to its specific active proteins. The transformation reaction begins with the action of alcohol dehydrogenases and the transformation of ethanol into acetaldehyde (aka acetaldehyde, ethanal, methyl formaldehyde).
The substance is several tens of times more dangerous in its toxic properties than alcohol itself. It is classified as a first-order carcinogen due to its ability to destroy the DNA of genes and cause cancerous degeneration. Therefore, the negative consequences of the action, in addition to alcoholic hepatitis, include the development of malignant tumors of the stomach, esophagus and liver. Further transformation occurs under the influence of acetaldehyde dehydrogenase. It converts methyl formaldehyde into acetic acid and non-toxic substances that are excreted in the urine.
It is important that with constant consumption of alcoholic beverages, the synthesis of necessary enzymes lags behind the need. This leads to increased exposure of the liver to undegraded acetaldehyde. Liver cells (hepatocytes) respond with an inflammatory response.
In the pathogenesis of alcoholic hepatitis, damage to other organs of the digestive system plays a significant role:
- pancreas (pancreatitis);
- stomach (gastritis);
- gallbladder (cholecystitis).
Pathogenetic mechanisms of liver intoxication
The main metabolite of ethyl alcohol, acetaldehyde itself has a damaging effect on hepatocytes. This connection calls:
- damage to cell membranes and, accordingly, their necrosis;
- increased synthesis of triglycerides and their deposition in hepatocytes;
- impaired synthesis of serum albumin (this protein determines the colloid osmotic pressure of the blood);
- violation of the filtration function of the liver;
- stimulation of lipid peroxidation processes.
In place of damaged hepatocytes, foci of connective tissue form. This leads to a deterioration in the blood supply to liver cells, progression of the inflammatory reaction, and activation of carcinogenesis processes. It has been established that one of the most dangerous forms of cancer, hepatocellular carcinoma, in the vast majority of cases develops against the background of progressive cirrhosis.
Features of women's lesions
More severe and rapid liver damage in women is explained by:
- A physiological feature of the composition of gastric juice in the female body is that women have significantly less production and content of the enzyme alcohol dehydrogenase than men, therefore, ethanol is not broken down in the stomach, enters the liver in massive quantities and represents a significant burden.
- A larger mass of adipose tissue in the body and a smaller mass of water, which leads to a lack of dilution of ethanol, increases its toxicity. Fats in the liver parenchyma enhance oxidative reactions, promote rapid inflammation and outcome in fibrosis.
- An imbalance of estrogen during menopause, which negatively affects alcohol intoxication.
All factors indicate a significant reduction in time of alcohol abuse for women compared with men for the same liver damage
Treatment of alcoholic hepatitis requires taking into account gender characteristics and their correction.
Content:
- What kind of disease
- Forms and symptoms of the disease
- Diagnostic methods
- How is the treatment carried out?
- Diet
Alcoholic hepatitis or steatohepatitis is a common complication of chronic alcohol dependence. The disease is characterized by signs of severe inflammation, fatty degeneration, and fibrosis.
Without timely treatment it leads to the death of the patient.
What does the dose of alcohol matter?
The development of alcoholic hepatitis is due to:
- dose of ethanol contained;
- quality of the alcoholic drink;
- duration of use.
The daily amount of alcohol for the development of hepatitis and cirrhosis of the liver is:
- for an adult man 50–80 g;
- women – 30–40;
- teenager – 15–20.
Doctors categorically deny the safety of beer.
Men drink 3–5 liters at a time, which is equivalent to 120–200 g of ethanol and is 3–4 times higher than the permissible norms
For a teenager, 0.5 liters of “non-alcoholic” beer poses a danger. According to the preparation technology, it must contain up to 5% ethanol. In addition, with beer, the load on the liver increases due to the carbohydrates contained, which are processed into fats and remain in the parenchymal cells.
A special role in the development of the acute form of alcoholic hepatitis is given to poisoning with surrogates of alcohol-containing household liquids. Toxic substances in these cases are, in addition to alcohol:
- isopropyl alcohol;
- diethyl phthalate;
- methyl alcohol;
- polyhexamethylene guanidine hydrochloride (component of disinfectants);
- acetaldehyde.
Most attending physicians (gastroenterologists, hepatologists) consider it important in making a diagnosis not to specify the dose of the drink consumed by the patient, but to determine the regularity of alcohol entering the body.
Causes of the disease
The disease is formed as a result of prolonged abuse of alcoholic beverages, especially surrogates. The speed of its development is determined by the doses taken, the strength and quality of the alcohol. The individual characteristics of the drinker’s body are of no small importance. Usually, after 5-7 years of regular drinking, serious complications appear. The pathology develops most quickly in persons with congenital deficiency of enzymes that neutralize ethanol and in weakened patients.
Risk factors
For the occurrence of hepatitis in the liver against the background of alcohol abuse, the following are important:
- malnutrition (deficiency of fruits and vegetables, meat products);
- treatment with hepatotoxic drugs and herbs (for example, St. John's wort should be taken according to its name);
- infection by viruses with a predominant effect on liver cells;
- lack of immunity;
- genetic predisposition in the form of inhibition of the synthesis of the necessary set of enzymes.
The clinical course of alcoholic hepatitis is associated with a combination of all of these factors. Depending on the duration and symptomatic complex of the lesion, it is customary to distinguish between acute and chronic forms.
Consequences and complications
Severe complications occur with liver cirrhosis. Among them it is worth highlighting:
- Variceal bleeding due to portal hypertension .
- Hepatic encephalopathy.
- Ascites.
- Infection. This is a common complication in severe hepatitis and cirrhosis . The most common causes are spontaneous bacterial peritonitis , bacteremia , respiratory infection, and urinary tract infections.
- Hepatorenal syndrome . This is the development of renal failure with severe impairment of liver function.
- Hepatocellular carcinoma.
Acute form
The acute form of alcoholic hepatitis is caused by rapidly progressing inflammatory and destructive processes in the liver cells, most often after a long period of heavy drinking against the background of liver cirrhosis that has already begun. In severe cases, the outcome is liver failure and death from coma. The duration of the course ranges from 3 to 5 weeks.
The acute form of hepatitis is caused by a one-time “impact” of alcohol on the liver
There are 4 clinical variants that differ in symptoms and prognosis.
Jaundice hepatitis is most common among people suffering from alcoholism. Symptoms of alcoholic hepatitis in this type are:
- yellowness of the skin and mucous membranes;
- paroxysmal nausea;
- weaknesses;
- loss of appetite;
- diarrhea followed by constipation;
- weight loss;
- dull pain in the right hypochondrium.
Patients are prone to bacterial infection with fever, inflammatory diseases of the urinary system. Skin itching is not typical. Hepatorenal syndrome is diagnosed during examination.
Latent (hidden) – there are practically no symptoms, detected by transaminase tests.
Cholestatic – found in 13% of patients, signs of impaired bile secretion are concentrated:
- significant yellowness of the skin and mucous membranes;
- darkening of urine;
- intense itching and scratching on the skin;
- discoloration of stool.
Differential diagnosis is always carried out with mechanical jaundice formed against the background of cholelithiasis, tumors of the liver and pancreas, and inflammation of the bile ducts.
Fulminant is the most severe fulminant form, as it quickly leads to:
- to brain damage (encephalopathy) with cell swelling;
- accompanied by hemorrhagic syndrome with hemorrhages;
- simultaneous kidney damage with a block of filtration function to the degree of renal failure;
- state of hypoglycemia;
- addition of infection.
It differs from others in the rapid necrosis of hepatocytes. Patients quickly develop confusion to a comatose state and severe jaundice.
Encephalopathy is characterized by swelling of brain tissue
A liver odor appears from the mouth, and the temperature is constantly high. Unlike viral hepatitis, acute forms are not accompanied by an enlarged spleen. The lack of timely treatment of alcoholic hepatitis in this case quickly leads to irreversible changes and death of the patient.
The most severe course is observed in patients with acute hepatitis against the background of existing liver cirrhosis.
Toxic hepatitis occurs with a pronounced stop in the movement of bile in the ducts (cholestasis). With this pathology, the destruction of hepatocytes is less pronounced. In severe forms it leads to acute liver failure.
Pathogenesis
acetaldehyde, plays a role in liver damage . It enters into a chemical bond with intracellular components (proteins in the first place) and disrupts their functions. Under the influence of acetaldehyde, the cell membrane and phospholipids are destroyed, the transport of substances through the membrane is disrupted, and the level of cytokines increases - this is the reason for the appearance of first steatosis , then hepatitis , fibrosis and cirrhosis . When interacting with acetaldehyde, substances with antigenic properties are formed. They, in turn, increase the activity of stellate cells. Activated cells play a major role in fibrogenesis—the development and progression of liver fibrosis. Thus, acetaldehyde causes immune-mediated damage to liver cells. In addition, in people who drink alcohol for a long time, intestinal permeability increases significantly. As a result, waste products of intestinal bacteria enter the bloodstream, in response to which pro-inflammatory cytokines and tumor necrosis factor TNFα are produced, which damages hepatocytes and is of great importance in the development of alcoholic hepatitis. With the development of cirrhosis, the liver venules expand, the arterioles narrow, which leads to an increase in pressure in the portal vein system (portal hypertension develops with characteristic manifestations - varicose veins of the stomach, esophagus, anterior abdominal wall, enlarged spleen and ascites).
Features of the chronic form
Chronic alcoholic hepatitis occurs with long-term constant consumption of alcohol; detection shows its presence in 1/3 of patients with alcoholism. Symptoms are mild and may be completely absent. The diagnosis is made when violations are detected by laboratory methods and compared with the patient’s alcohol history.
A detailed survey reveals some signs of pathology:
- loss of appetite;
- tendency to constant bloating;
- rare attacks of nausea;
- insomnia;
- decreased libido (sexual desire) due to impaired synthesis of sex hormones.
Palpation reveals a dense, painful edge of the liver protruding from under the right hypochondrium, signs of organ enlargement. This form of liver damage is also called alcoholic steatohepatitis, since fatty degeneration occurs in hepatocytes.
According to the clinical course, degrees are distinguished:
- mild – the patient has no complaints, but examination reveals an enlarged liver;
- medium - in addition to the enlarged organ, the patient has obvious pain in the right hypochondrium, yellowness of the sclera and skin, weight loss, loss of appetite;
- severe – characterized by a significant enlargement of the liver and spleen, the onset of cirrhosis.
Literature:
- Scheme of differential diagnosis of alcoholic and viral hepatitis [Text]: (Methodological recommendations) / Ministry of Health of the USSR; [Comp. Lebedev S.P., Mukhin A.S., Potekaeva M.A. and etc.]. — Moscow: b. i., 1979. - 8 p.
- Alcoholic liver disease: method. recommendations / Military medical. acad. them. CM. Kirov
- 2004 (State Unitary Enterprise of the Republic of Kazakhstan Republic, type. P.F. Anokhin).
- Differentiated approach to the management of patients with alcoholic hepatitis: abstract of thesis. ... Candidate of Medical Sciences: 01/14/28 / Komkova Inna Igorevna; [Place of protection: First Moscow. state honey. univ. them. THEM. Sechenov]. - Moscow, 2013. - 24 p.
The text was checked by expert doctors: Head of the socio-psychological service of the Alkoklinik MC, psychologist Yu.P. Baranova, L.A. Serova, a psychiatrist-narcologist.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!
Diagnostics
In the diagnostic process, it is difficult to determine the fact of alcohol abuse. The behavior of patients at work and at home differs significantly. Often patients hide their weakness and do not understand the meaning. Establishing the etiology of liver damage helps to establish:
- tendency to binge drink;
- development of abstinence;
- prolonged use of alcohol;
- hangover;
- inability to refuse alcohol-containing liquids.
To decide how best to treat the patient, it is necessary to exclude toxic hepatitis. The examination includes laboratory tests:
- on liver transaminases (aspartic and alanine); in case of hepatitis, aspartic is several times higher than alanine;
- moderately altered thymol test;
- an increase in bilirubin in the blood and urine indicates a difficult outflow of bile;
- gammaglutamyl transpeptidase increased activity;
- increase in immunoglobulin A.
Ultrasound and Dopplerography of the abdominal cavity reveals a disturbed structure of the liver, an increase in the size of the organ, an expansion of the diameter of the portal vein, as a sign of portal hypertension.
The radionuclide hepatosplenoscintigraphy method involves the use of specific isotopes deposited in the liver parenchyma. Based on the picture of the absorbed substance, one can judge the degree of damage to the organ.
Computed tomography – clarifies the presence of changes in the structure of the liver
It is important that it is possible to confirm the alcoholic etiology of hepatitis only by characteristic signs on a biopsy. They are to detect:
- alcoholic hyaline (Mallory body);
- changes in hepatocytes and stellate reticuloepitheliocytes.
Differential diagnosis of chronic form
Diagnostics needs to identify differences with non-alcoholic steatohepatitis in metabolic disorders and drug-induced hepatitis. Metabolic steatohepatitis is more often observed in women aged 40 to 60 years who suffer from:
- obesity,
- diabetes mellitus
At the same time, triglycerides accumulate in the liver, which can damage cell membranes and stimulate the development of fibrous tissue (the path to cirrhosis).
A blood test reveals a violation of the composition of fat components, a sharp increase in triglycerides, and hyperglycemia. There is no jaundice in the symptoms. Drug-induced steatohepatitis occurs as a result of side effects of medications with long-term use:
- drugs from the estrogen group;
- Amiodarone;
- high doses of acetylsalicylic acid;
- Sulfamethoxazole;
- calcium antagonists;
- anti-inflammatory drugs of the aminoquinolone series (Delagil, Plaquenil).
In the pathogenesis of this type of hepatitis, it is important to suppress the process of fatty acid oxidation at the level of hepatocyte mitochondria and activate the peroxide type of lipid oxidation. The doctor can find out what drugs the patient took, their dangerous dosage and duration of treatment. The outcome of non-alcoholic steatohepatitis also becomes cirrhosis of the liver. Rarely, fatty degeneration is droplet in nature and causes a fulminant form of acute hepatitis.
The final confirmation of non-alcoholic lesions can only be based on the results of a liver biopsy. Statistics show the presence of steatohepatitis in 7–9% of cases of all studies. Some experts consider it necessary to take into account the disease as a separate nosology.
Fatty liver hepatosis, treatment
Fatty liver
without the presence of fibrosis is not a precirrhotic condition. When you stop drinking alcohol, the organ structure is usually restored within 4-6 weeks.
With fatty liver hepatosis
a diet with a sufficient amount of protein, polyunsaturated fatty acids (vegetable oils, fish), preparations containing silymarin (hepatoprotectors-antioxidants), multivitamin pills containing microelements is prescribed, zinc is especially important, since it is a component of the enzymes alcohol dehydrogenase, superoxide dismutase (antioxidant body system), enzymes that stimulate the immune system.
In addition to the diet for the treatment of fatty liver disease
vitamins are needed. You should definitely prescribe alpha-tocopherol either with vitamin preparations, or increase the consumption of vitamin E-containing products: mainly unrefined vegetable oils, yolk, nuts, buckwheat, parsley, sprouted wheat seeds.
Treatment of alcoholic hepatitis
Cure alcoholic hepatitis is only possible if you completely stop drinking alcohol. There should be no substitutions for less concentrated drinks. The patient is offered a strict diet that provides the necessary calorie content, but excludes any toxic effects on the liver.
Typical table No. 5 is assigned:
- The calorie content of the diet should be at least 2000 kcal per day;
- protein products are prescribed at the rate of 1 g per kilogram of the patient’s weight;
- An essential component is B vitamins and folic acid.
In the hospital, in the absence of appetite and refusal to eat, nutrition is provided through a tube or intravenous administration of amino acids and nutritional mixtures.
Patients often suffer from alcohol withdrawal and require parallel treatment from a narcologist
The specialist tries to explain whether it is possible to drink beer or cognac, thereby destroying the stereotypical behavior of an alcoholic.
In severe forms of alcoholic hepatitis, courses of antibiotics are used to prevent bacterial infections. Fluoroquinolone group drugs work better.
Hepatoprotectors have a selective effect on liver cells. It is believed that they restore oxidative processes in hepatocytes and promote parenchyma regeneration. Protectors based on:
- milk thistle flavonoids;
- bear bile (Ursosan);
- Admetionine;
- essential phospholipids.
Ursodeoxycholic acid contained in Ursosan reduces cholesterol synthesis and helps replenish the lack of bile during digestion. The transformation of the inflammatory process into fibrosis and the formation of cirrhosis has only one treatment option - liver transplantation. The operations are still rarely carried out; they involve searching for a donor and are expensive.
How is the treatment carried out?
To eliminate the disease, an integrated approach is used. But treatment will be ineffective if the patient does not stop drinking alcohol. In mild cases of the disease, this is enough to restore the liver.
Drug therapy:
- Essential phospholipids. They reduce fatty changes in the liver, have an antioxidant effect, slow down fibrosis, and activate the regeneration of hepatocytes.
- Preparations based on ursodeoxycholic acid. Used as cytoprotectors.
- Hepatoprotectors. Block the production of acetaldehyde, restore damaged cell membranes.
- Glucocorticosteroids. Used for hepatic cell failure syndrome.
- In the acute form, detoxification is necessary. Using droppers, plasma-substituting solutions are administered to prevent fibrosis and means to restore electrolyte balance.
- Infusion of amino acids. Prescribed to reduce the consumption of protein reserves and improve metabolism in brain structures.
In case of irreversible disorders, organ transplantation is required.
Forecast
Alcoholic hepatitis occurs in two forms:
- Progressive – accounts for about 20% of cases, characterized by small focal lesions of the liver parenchyma resulting in cirrhosis. Accompanied by the clinic described above. Allows you to achieve stabilization of metabolic rates and stop inflammation if treatment is started on time and is not accompanied by repeated binges.
- Persistent - the form is characterized by a stable course and reversibility of processes in the liver. The asymptomatic picture lasts up to 10 years. There is no deterioration even with rare alcohol consumption.
In the absence of alcohol cessation, mortality in the acute phase of hepatitis against the background of another binge is up to 60%. The prognosis for increased life expectancy increases significantly for patients who were able to stop the addiction.
However, even with good results of therapy, one should remember the high risk of malignancy and monitor nutrition.
The problem of treating alcoholic hepatitis is solved by different specialists. It is important that in the presence of liver damage, narcologists and psychiatrists cannot prescribe potent drugs. The choice of therapy is limited according to the destructive processes in the liver tissue. Therefore, experts advise alcohol-dependent people to contact them as early as possible.