Chronic hepatitis is a group of liver diseases that develop after suffering viral hepatitis, taking certain medications, alcohol abuse and with a duration of the inflammatory process of more than 6 months. In addition, it occurs in patients with chronic diseases of the abdominal organs - gastritis, enterocolitis, pancreatitis, peptic ulcer and cholelithiasis, after gastrectomy, as well as in diseases not related to the gastrointestinal tract: various infectious diseases, collagenoses. All chronic hepatitis can be divided into the following forms: chronic persistent hepatitis, chronic active hepatitis, chronic cholestatic hepatitis.
Chronic persistent hepatitis
The most benign form. There may be complaints of minor aching pain or heaviness in the right hypochondrium, intermittent general weakness, and fatigue. Often patients do not feel their illness, there are no complaints at all. The liver is slightly enlarged, slightly painful, the spleen is rarely enlarged, there is no jaundice. treatment of chronic hepatitis Changes in biochemical blood tests - increased transaminases, thymol test only during an exacerbation. The course is perennial and does not progress. With a rational lifestyle (diet, alcohol prohibition), recovery is possible.
Treatment. Meals should be 4 times a day with the complete exclusion of mushrooms, canned, smoked and dried foods, fried foods, chocolate products, cream and pastries, alcohol, and limit the consumption of animal fats (fatty meats, duck, goose, pork). 1-2 times a year courses of vitamin therapy (group B, ascorbic acid, rutin). Taking choleretic drugs is not recommended. Once every 6-12 months, the patient undergoes a blood test for liver tests.
Causes of toxic hepatitis
There are several reasons that cause toxic liver damage:
- industrial poisons - organophosphorus pesticides, insecticides, trichlorethylene, metals and metalloids, arsenic, aldehydes, phenols, etc.;
- plant alkaloids - strychnine, quinine, aconite, cocaine, colchicine, hyoscine, etc.;
- toxins of poisonous mushrooms;
- alcoholic drinks;
- medicinal hepatotoxins - anticonvulsants, antituberculosis, psychotropic drugs, antibiotics, cytostatics and more.
Risk factors that increase the likelihood of toxic hepatitis include:
- unfavorable environmental situation;
- frequent stress;
- poor nutrition;
- long-term uncontrolled use of medications;
- alcohol abuse;
- concomitant diseases of the hepatobiliary system (associated with impaired excretion of bile from the body).
Chronic active hepatitis (CHAT)
This form develops after viral (infectious) hepatitis with pronounced inflammatory-necrotic changes.
Complaints: general weakness, fatigue, significant decrease in ability to work, nausea, loss of appetite, heaviness and pain in the right hypochondrium. In addition to these complaints, patients, depending on the severity of the disease, develop hemorrhagic syndrome (bleeding from the gums and nose, subcutaneous hemorrhages), an increase in temperature from low subfebrile to high numbers, “spider veins” appear on the chest and shoulders, and damage to other organs occurs: pain in joints, inflammatory processes in the lungs, kidneys, heart, pleurisy (inflammation of the pleura with accumulation of fluid in the pleural cavity). The liver is enlarged, painful, dense, and in most cases the spleen is also enlarged.
Recognition. Biochemical blood tests: transaminase activity can exceed normal levels by 5-10 times, depending on the severity of the process, protein fractions of the blood are disturbed - albumin decreases, gamma globulins increase significantly. The level of bilirubin in the blood increases. Prothrombin decreases. Ultrasound and scanning (radioisotope examination of organs) reveal an enlarged liver and spleen and their diffuse changes. Approximately half of the patients experience a transition to liver cirrhosis; periods of remission can last from several years to several months. Treatment is similar to that for chronic persistent hepatitis.
Treatment of chronic hepatitis is contraindicated by taking choleretic, liver extracts such as sirepar, anabolic hormones (retabolil), or any physiotherapeutic procedures. Prescribing Legalon, Karsil, Essentiale is not advisable, as they can cause an increase in inflammation. Treatment with corticosteroids (prednisolone), levamisole (Decaris) only as prescribed and under the supervision of a physician. In case of severely active CAH, patients are referred to VTEC to determine the disability group due to persistent loss of ability to work.
Causes of chronic viral hepatitis
The disease is caused by hepatitis B, C and D (delta) viruses - the hepatitis A virus, as a rule, provokes an acute form of the disease. The most common cause of chronic hepatitis is the hepatitis C virus; it is found in 77.97% of cases of newly diagnosed chronic hepatitis in Russia. Every year, it infects about 50 thousand people throughout the country.3 The next most common is the hepatitis B virus. According to WHO, at least 257 million people worldwide are sick with it.4 In Russia, the incidence averages 10.78 people per 100 thousand ,5 but varies greatly by region. Hepatitis D can only accompany and aggravate hepatitis B, since it is not self-sufficient in terms of reproduction.
Invading liver cells, hepatitis B and C viruses leave particles of their antigens on the surface of the membranes. The immune system begins to view infected hepatocytes as foreign cells and attacks them. If the immune response is adequate, such an attack, although accompanied by symptoms of liver damage (clinical manifestations of acute viral hepatitis), quite quickly destroys infected cells. But the immune system cannot cope with the virus itself, and its activity is not enough to completely eliminate the infectious agent, as a result of which chronic hepatitis develops.
The liver has enormous regeneration capabilities, but since in chronic hepatitis the inflammatory process can last for years and decades, sooner or later the organ’s reserves may be depleted. In this case, connective (fibrous, scar) tissue is formed in place of the dead cells. It is not able to perform the functions of hepatocytes, and fibrotic degeneration of the liver can result in the development of liver failure. Another long-term, but very dangerous outcome of chronic hepatitis is the degeneration of hepatocytes and the formation of hepatocellular carcinoma (liver cancer).
If the infection occurs in adulthood, and the activity of the inflammatory process is low, chronic viral hepatitis can last for several decades. In this case, there is a possibility that the patient will die from causes unrelated to chronic hepatitis. If the infection entered the body in youth, and the inflammatory process is active, the likelihood of unfavorable developments is much higher. According to WHO, 720 thousand people die annually from liver cirrhosis due to viral hepatitis and 420 thousand die from hepatocellular carcinoma.4 Chronic hepatitis B with the delta agent (combined infection B and D) develops especially quickly and unfavorably.6
Classification of hepatitis
Chronic viral hepatitis is classified according to its causes and is divided into the following types:
- chronic viral hepatitis B;
- chronic viral hepatitis C;
- chronic viral hepatitis B with delta agent.
According to the degree of activity of the pathological process, the following types of chronic hepatitis are distinguished:
- with minimal activity;
- with moderate activity;
- with pronounced activity.
In addition, there are four stages of development of liver fibrosis - from mildly expressed to entailing a violation of the architectonics (characteristic structure of tissues) of the organ. The higher the stage of fibrosis, the more pronounced the pathological changes.
Chronic cholestatic hepatitis
Liver disease of a diffuse nature as a result of inflammation along the small bile ducts, stagnation of bile in the liver tissue.
The manifestations and complaints are the same as with other chronic hepatitis, but jaundice is more pronounced, which causes more severe skin itching, sometimes even before the skin turns yellow. Under the skin, in the corners of the eyes, yellow dense spots-xanthomas and xanthelasmas appear. A biochemical blood test shows a higher level of bilirubin, alkaline phosphatase (5 or more times higher than normal), and cholesterol. The principles of dietary nutrition and treatment are the same as for chronic active hepatitis, as well as vitamins A, E, B, Vicasol, to reduce skin itching - drugs that bind bile acids (bilignin, cholestyramine), choleretic.
Hepatitis is an inflammation of the liver. If the inflammatory process lasts less than 6 months, hepatitis is acute; if it lasts more than 6 months, it is chronic.
Hepatitis can be caused by various factors. There are infectious and non-infectious hepatitis. Among infectious diseases, the most common are viral ones, but there are hepatitis caused by bacteria and parasites. Non-infectious ones can be caused by toxic substances, including alcohol, diseases of other organs and systems of the body. Chronic alcoholism is one of the main causes of non-infectious hepatitis: approximately 20% of patients suffering from alcoholism for 5-6 years develop alcoholic liver damage.
As a rule, acute hepatitis ends in complete recovery. Sometimes the disease becomes chronic, which can last for months or years, and in some cases leads to cirrhosis or liver cancer.
Synonyms Russian
Non-infectious hepatitis, alcoholic hepatitis, non-alcoholic steatohepatitis, fatty hepatosis, drug-induced hepatitis, toxic hepatitis, toxic-allergic hepatitis, idiopathic hepatitis, autoimmune hepatitis, reactive hepatitis, chronic persistent hepatitis, chronic active hepatitis, necrotizing hepatitis, lobular hepatitis, neonatal hepatitis, acute hepatitis, chronic hepatitis.
English synonyms
Acutehepatitis, chronichepatitis, nonviral hepatitis, noninfectious hepatitis, non-alcoholic hepatitis, non-alcoholic steatohepatitis, NASH, toxic hepatitis, autoimmune hepatitis, neonatal hepatitis, d-induced hepatitis, alcoholic hepatitis.
Symptoms
In the initial stages, hepatitis may occur unnoticed. The first signs of the disease are usually nonspecific. The intensity of symptoms depends on the cause of hepatitis, the activity and duration of the pathological process. The main symptoms of hepatitis are:
- weakness, malaise;
- yellowness of the skin, sclera;
- pain in muscles and joints;
- loss of appetite;
- nausea, vomiting, heaviness in the stomach;
- fever.
General information about the disease
The liver is one of the most important human organs. It is located in the upper right part of the abdominal cavity, bordered by the diaphragm, right kidney, intestinal loops, stomach and consists of two main lobes (right and left), which are formed by thousands of lobules. The lobules consist of hepatocytes - cells responsible for performing the main functions of the liver. The liver is supplied by the hepatic artery, which carries oxygen-rich blood, and the portal vein, which carries blood from the gastrointestinal tract. The outflow of blood is carried out through the hepatic vein. There is also a complex system of bile ducts through which the synthesized bile enters the gallbladder, where it accumulates, and into the intestines.
The liver performs a number of vital functions: synthesizes proteins (albumin, coagulation factors), cholesterol, enzymes, hormones, bile, cleanses the blood of excess hormones, metabolic products, toxins and microorganisms that enter the blood through the digestive system, participates in the metabolism of carbohydrates, vitamins, microelements.
Exposure to a number of factors can lead to liver damage and disruption of its function. With hepatitis, the liver tissue becomes inflamed, leukocytes accumulate in it, areas of necrosis (death) may appear, and a small amount of connective fibrous tissue appears. However, in general, unlike cirrhosis, the structure of the liver lobules is not disturbed. Inflammation is accompanied by stagnation of bile and dysfunction of hepatocytes.
Depending on the cause of occurrence, the following types of non-infectious hepatitis are distinguished.
- Alcoholic hepatitis. It is formed as a result of many years of alcohol abuse, which disrupts the metabolism in hepatocytes, leading to their destruction.
- Non-alcoholic steatohepatitis. This is a condition in which changes in the liver resemble alcoholic hepatitis, but are not associated with alcohol intake. Non-alcoholic steatohepatitis can be combined with metabolic diseases: obesity, diabetes. In some cases, it occurs in people without concomitant diseases and even in children.
- Drug-induced hepatitis. Taking a number of medications - antibiotics, anti-tuberculosis drugs, oral contraceptives - sometimes leads to hepatitis. The likelihood of toxic effects of drugs on the liver is determined by individual tolerance to the drugs.
- Toxic hepatitis. It can be caused by poisonous mushrooms, alcohol substitutes, arsenic compounds, toluene, benzene, lead and other substances that have a direct destructive effect on liver cells.
- Autoimmune hepatitis. With this disease, the immune system is disrupted, which begins to destroy its own, normal liver cells. The mechanism of development of autoimmune hepatitis is not fully understood.
- Metabolic hepatitis. Caused by hereditary metabolic diseases, such as hemochromatosis (increased absorption of iron in the intestine with its deposition in the tissues of the body) or Wilson's disease (a disorder of copper metabolism with its deposition in the liver and other organs).
- Reactive hepatitis. It can be formed as a result of exposure to toxins and metabolic products that enter the blood during diseases of other organs (stomach ulcers, pancreatitis, endocrine and autoimmune diseases).
- Primary biliary hepatitis. Associated with impaired patency of the bile ducts, impaired outflow of bile, which leads to damage to liver tissue.
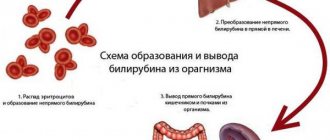
Liver cells in hepatitis can be damaged not only as a result of direct exposure to toxic substances, but also due to the pathological activity of cells of the body's own immune system. As a result, the functioning of the liver is disrupted, which leads to the characteristic symptoms of hepatitis: the liver increases in size, there is a feeling of heaviness in the abdomen, the outflow of bile necessary for the digestion of fats slows down, which causes nausea, vomiting, flatulence, stool disorders (diarrhea or constipation ). Violation of protein (albumin) synthesis leads to a decrease in the osmotic pressure of the blood and the release of fluid into the tissue, which causes edema. A decrease in the number of clotting factors leads to increased bleeding. The purification of the blood from toxic substances is impaired, which is manifested by weakness, malaise, and fever. Yellowness of the skin and mucous membranes is caused by an increase in bilirubin levels. It is formed during the destruction of red blood cells, binds to glucuronic acid in the liver (direct, bound bilirubin is formed) and is excreted in the bile. With hepatitis, this process is disrupted and direct bilirubin enters the blood.
Who is at risk?
- Alcohol abusers.
- Obese people.
- Patients with chronic autoimmune and endocrine diseases.
- Patients who require long-term use of medications that have a toxic effect on the liver.
- Contact with high doses of toxic chemicals.
Diagnostics
Manifestations of hepatitis depend on the immediate cause of liver damage. In some cases, hepatitis may have nonspecific symptoms or even be asymptomatic. A thorough interview and examination of the patient helps the doctor suspect hepatitis, but additional research is needed to make a final diagnosis.
Laboratory diagnostics
- General blood analysis. An increased level of white blood cells is a sign of the infectious nature of hepatitis.
- Prothrombin index. This is the ratio of the blood clotting time of a healthy person to the clotting time of a sick person. Prothrombin is a precursor of thrombin and is involved in blood clotting. The test is used to evaluate the rate of blood clotting. In the initial stages of hepatitis, the prothrombin index is normal; in severe cases of the disease it can be reduced.
- Fibrinogen. A blood clotting factor that is synthesized by liver cells. When liver tissue is damaged, fibrinogen is reduced.
- AST (aspartate aminotransferase), ALT (alanine aminotransferase). Liver enzymes that enter the bloodstream when liver tissue is damaged. With hepatitis, they may be increased.
- Gamma-glutamyl transpeptidase (gamma-GT). A liver enzyme, the amount of which increases with damage to the liver and bile ducts.
- Alkaline phosphatase. An enzyme that is found in all tissues of the body, but in the greatest quantities in bones, kidneys and liver. In case of hepatitis, it may be increased.
- Total bilirubin. Bilirubin in hepatitis is increased mainly due to the direct (bound) fraction.
- Total whey protein. With hepatitis, the level of total protein can be reduced by reducing the amount of albumin.
- Total cholesterol. This substance is synthesized in the liver and is an element of cell membranes, a precursor of bile acids and some hormones. In case of hepatitis, it may be lowered, which indicates a violation of the synthetic function of the liver.
- Tests for hepatitis B, C, D. The presence of hepatitis viruses in the body is determined as a possible cause of the disease.
- Ferritin, transferrin. Ferritin is a protein that binds iron in the liver, and transferrin is a protein that transports iron from the intestines to the liver. Their levels may be elevated in hemochromatosis.
- Copper, ceruloplasmin. The level of these substances is measured when Wilson's disease is suspected, in which the concentration of ceruloplasmin decreases and the concentration of copper increases.
- Screening study for the presence of narcotic, psychotropic and potent substances. Determination of compounds that could cause hepatitis.
Additional Research
- Ultrasound of the abdominal organs. Used to determine the size and structure of the liver. With hepatitis, the liver may be enlarged.
- X-ray, CT, MRI. Helps determine the size and structure of the liver, and exclude other liver diseases.
- Retrograde cholangiography. This is an x-ray examination, which is carried out after the injection of a contrast agent into the bile ducts, visible in the image. Used to assess the patency of the bile ducts.
- Liver biopsy. Taking a sample of liver tissue using a thin, hollow needle that is inserted through the skin of the abdominal wall after preliminary anesthesia. It is carried out under ultrasound control. Microscopy of the sample taken reveals inflammation of the liver tissue, accumulation of leukocytes, and a small amount of connective tissue while maintaining the structure of the liver lobules.
Treatment
Treatment of acute hepatitis is based, first of all, on stopping the impact of the pathological factor on the liver and is aimed at preventing the disease from becoming chronic. Most acute hepatitis is completely curable. Chronic hepatitis, depending on the cause and activity of the process, can last from 6 months to several years. A long course involves regular examinations, strict adherence to the doctor’s recommendations, changes in the patient’s lifestyle - this is necessary for the prevention of liver cirrhosis, liver failure, and liver cancer.
Prevention
- Quitting alcohol and drugs.
- Follow the instructions and recommendations of the doctor when taking medications.
- Use of protective equipment when working with toxic chemicals.
- Fighting excess weight.
Recommended tests
- General blood analysis
- Coagulogram No. 2 (prothrombin (according to Quick), INR, fibrinogen)
- Alanine aminotransferase (ALT)
- Aspartate aminotransferase (AST)
- Gamma-glutamyl transpeptidase (gamma-GT)
- Total alkaline phosphatase
- Total bilirubin
- Direct bilirubin
- Total protein in whey
- Serum albumin
- Total cholesterol
- Transferrin
- Ferritin
- Ceruloplasmin
- Copper in the blood
- HBsAg, hypersensitive
- Anti-HCV, antibodies
- Screening study for the presence of narcotic, psychotropic and potent substances
- Cytological examination of punctates, scrapings of other organs and tissues
Complications of toxic hepatitis
In case of mild poisoning, timely treatment of toxic hepatitis leads to complete relief from the disease. In more severe cases, massive liver damage can lead to serious complications.
Liver failure
– a complex of symptoms, including weight loss, swelling of the face and legs, jaundice, accumulation of ascitic fluid, subcutaneous hemorrhages, mental and neuromuscular disorders.
Cirrhosis of the liver
– replacement of hepatocytes with fibrous connective tissue.
Hepatic coma
– a progressive disruption of the organ and central nervous system, which can lead to death.
Treatment of toxic hepatitis
First of all, the treatment of toxic hepatitis involves the most complete elimination of contact with the toxic substance. Patients are prescribed strict bed rest. If toxins penetrate through the digestive tract, gastric lavage is performed before starting drug therapy. Further, in order to remove poison from the body, patients with toxic hepatitis may be advised to take adsorbents, drip infusion of electrolyte solutions, and in case of severe liver damage, blood purification (plasmapheresis or hemosorption).
To activate the process of eliminating toxic substances during the treatment of hepatitis, choleretic drugs can be used, and in case of mushroom poisoning, antidotes can be used. In order to maintain liver function, vitamin therapy is carried out using B vitamins and ascorbic acid.
Diagnostics
Diagnosis of toxic hepatitis includes instrumental and laboratory methods that are also used in identifying other acute and chronic liver lesions. During the first medical consultation, a physical examination and history taking are performed. In most cases, this allows you to get a rough idea of the reasons that triggered the development of toxic hepatitis.
Laboratory methods for diagnosing liver damage:
- biochemical blood test - determination of the level of direct, indirect and total bilirubin, alkaline phosphatase, AlT and AST and γ-GTP;
- coagulogram - prescribed to assess the state of the hemostatic system;
- general blood and urine tests;
- tests to exclude the presence of other forms of hepatitis.
Instrumental diagnostic techniques:
- Ultrasound of the abdominal organs;
- liver scintigraphy;
- MRI;
- laparoscopic examination with targeted puncture biopsy of the liver.