Causative agents of viral hepatitis
Pathogenic microbes that affect the liver enter the body with contaminated food, water, and through close contact with infected people. Some pathogens are contained in mucous secretions and saliva of patients, others are transmitted only through blood. Hepatotropic virions have specific proteins on the surface of their shells that “cling” to the liver, multiply in its cells, destroy them, causing hepatitis.
The group of causative agents of this pathology includes several types of viruses:
- Provoking hepatitis A (Botkin's disease): RNA-containing microbe. It lives in sewage and has an oral-fecal route of infection. Causes “jaundice” due to insufficient sanitary processing of food and drinking water, and enters the body from dirty hands. Hepatitis A is acute and lasts several weeks. With adequate treatment, it does not cause irreversible consequences and does not persist in the body.
- The causative agent of hepatitis B: an extremely contagious and pathogenic virus with its own DNA. It is transmitted parenterally: through blood transfusions, through accidental injuries to the mucous membranes and skin, through the use of contaminated medical instruments, through sexual contact, from sick mothers to newborns. Depending on the state of immunity, it causes acute or chronic hepatitis. With a prolonged course, it is integrated into the human genome, recurs, and often leads to cirrhosis and liver cancer. After an acute form of inflammation, the body develops lifelong immunity to hepatitis B. Chronic pathology is incurable.
- Hepatitis C virus: a deadly pathogen, has more than 10 varieties. Transmitted through blood and sexual contact. It provokes a latent disease that leads to irreversible liver damage. It is practically incurable, but with proper therapy, patients can live fully with hepatitis C for decades.
- Hepatitis D virus: a non-enveloped pathogen that parasitizes other viruses. It is not transmitted independently, but together with hepatitis B, complicating its course. Mixed infection several times more often leads to the death of patients from hepatic encephalopathy, severe coma, and subsequent disability.
- Hepatitis E virus: similar to pathogen A. It is transmitted through contaminated water, food, household items, penetrating the gastrointestinal tract. It has the same symptoms, but is more severe than Botkin’s disease, often leading to persistent impairment of liver function.
Scientists claim that in nature there are other types of hepatotropic viruses that infect people, but not all of them have been studied.
Hepatitis B
A typical sexually transmitted disease. It is caused by the hepatitis B virus and is transmitted through contact with infected semen, blood and other body fluids. There are about 250 million people in the world infected with hepatitis B. Ways of contracting
hepatitis B: - Unprotected sexual intercourse with an infected person.
— When using a syringe that was previously used by an infected person. Most often, people who use drugs become infected in this way. — Sharing a razor or toothbrush with an infected person. - When applying a tattoo. The main symptom of
hepatitis B is intoxication of the body due to impaired liver function.
It causes fever, joint pain, increased fatigue, weakness, and sleep disturbances. And in severe cases of the disease there may even be disturbances of consciousness. The hepatitis B virus becomes chronic
and cannot be completely cured. It causes serious damage to the liver, which can cause cirrhosis or the formation of a cancerous tumor in its cells.
Symptoms of viral hepatitis
Manifestations of the disease depend on the viral load and type of infection. The incubation period for hepatitis lasts several weeks. At this time, carriers feel satisfactory, but already pose a danger to others. The first signs of pathology often resemble ARVI:
- physical weakness;
- muscle and joint pain;
- increased sweating;
- temperature rise to +37°C and above.
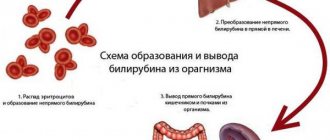
With the development of an acute form of the disease (hepatitis A, B, E), severe fever, headaches, lack of appetite, nausea and vomiting are possible. After a few days, due to disturbances in bilirubin metabolism and hematopoietic functions, symptoms characteristic of liver damage appear:
- yellowing of the whites of the eyes, oral mucosa, skin;
- darkening of urine;
- stool discoloration;
- severe itching on the body;
- the appearance of red spots, spider veins, and bruises on the skin of the palms, shoulders, and neck.
Jaundice with viral hepatitis can be pronounced or barely noticeable. As the pathology develops, other signs join it:
general intoxication: severe weakness, periodic vomiting, upset stool;
dull or sharp pain in the right hypochondrium.
Often, against the background of hepatitis, the liver and spleen increase in size. Some patients experience internal bleeding. In severe cases, inflammation of the internal organs leads to the accumulation of fluid in the abdominal cavity - ascites. Acute forms of hepatitis B and E are fraught with acute intoxication of the body and coma due to extensive liver damage.
With a favorable course of acute hepatitis, the signs of the disease subside within 3–4 weeks. Full recovery takes up to 2–3 months. In older people, residual manifestations are possible for up to 5 months.
With chronic viral hepatitis B and C, patients are unaware of infection for several months or years. These diseases are characterized by periodic disturbances in well-being:
decreased appetite, bitter belching;
discomfort in the right side;
temporary physical weakness, increased fatigue.
Many people learn about the presence of the disease from the results of medical tests, when the process is in an irreversible advanced stage. In almost half of the cases, chronic viral hepatitis leads to loss of liver function, development of fibrosis and cirrhosis. Hepatitis B is a common causative agent of carcinoma, one of the deadly forms of cancer.
What is the liver?
The liver is the largest organ
in the body, weighing about 1.3 kg. It consists of four lobes of different sizes and shapes and is located in the abdominal cavity on the right below the diaphragm. The human liver has many functions: - Detoxification - filtering harmful substances from the blood, such as alcohol. — Accumulation and preservation of nutrients. For example, vitamins A, D, and B12. - Synthesis of amino acids - the “building blocks” of proteins. - Production of digestive enzymes - bile. — Maintaining optimal blood sugar levels. -Produces 80 percent of the body's cholesterol. — Glycogen storage and conversion of glucose into glycogen. - Production of hormones.
Prevention of hepatitis
Infection with viral hepatitis can be prevented by following basic rules of safe behavior (maintaining hygiene standards, avoiding the use of drugs, using disposable equipment, responsible sexual behavior), as well as through vaccination.
Now there are vaccines that reliably protect against hepatitis A and B. Due to the variety of types of the virus, a vaccine against hepatitis C has not yet been developed.
In order to prevent the development of toxic hepatitis, toxic effects on the body, including alcohol consumption, etc., should be limited as much as possible; you should also not indulge in self-medication.
Diagnosis of hepatitis
Manifestations of hepatitis vary and depend directly on the cause of liver damage. There are cases when hepatitis does not have specific symptoms or is completely asymptomatic. Only a detailed survey and thorough examination of the patient allows a specialist to establish hepatitis in such cases. But in order for the diagnosis to be confirmed as final, additional research may be needed.
Laboratory diagnosis of hepatitis includes the following tests:
- Clinical blood test;
- Gamma-GT;
- Coagulogram;
- Direct and total bilirubin;
- AST;
- ALT;
- alkaline phosphatase;
- Albumin (code 79) and total protein in serum;
- Transferrin (code 28);
- Copper in the blood;
- Ceruloplasmin (code 110);
- Ferritin (code 30);
- Total cholesterol;
- HBsAg (code 833 or code 839);
- Anti-HCV, antibodies, ELISA;
- Cytological examination of punctates, as well as scrapings of other tissues and organs;
- A screening study to detect the presence of psychotropic, narcotic and potent substances.
Additional tests to diagnose hepatitis include an abdominal ultrasound.
The most important
The most common forms of hepatitis are A, B and C. The first form is transmitted through food and water, hepatitis B is mainly transmitted through sexual contact, and hepatitis C is transmitted through blood.
You can protect yourself from hepatitis by following basic rules of personal hygiene, getting vaccinated, not using drugs and protecting yourself during sexual contact. Illustration: Coast Guard Tags:
- Hygiene
- Liver
- Alcohol
- Safety
- Viruses
To leave a comment you must be an authorized user
Reasons for development
There is no generally accepted classification of all types of hepatitis. Depending on the reasons that caused the inflammation, there are:
- Infectious hepatitis: viral hepatitis A, B, C, D, E and others; hepatitis developing with yellow fever, cytomegalovirus infection, rubella, mumps, infection with the Epstein-Barr virus, herpes viruses, Lassa fever, HIV infection, etc.; bacterial hepatitis (for example, with syphilis, leptospirosis).
- Toxic hepatitis: alcoholic, drug-induced, and hepatitis caused by poisoning with other chemicals.
- Autoimmune hepatitis.
- Non-alcoholic steatohepatitis.
- Other types of hepatitis.
Autoimmune hepatitis
The incidence of autoimmune hepatitis is about 15-20 people. per 100 thousand population. The disease is usually based on a hereditary predisposition, a kind of congenital defect of the immune system.
The essence of the disease is the development of a pathological immune reaction against one’s own liver cells. Quite often, the pancreas, thyroid, and salivary glands are also involved in the pathological process.
To diagnose autoimmune hepatitis, a number of additional tests may be required, in particular for the presence of antinuclear antibodies and anti-smooth muscle antibodies. Much more often this pathology develops in women.
Treatment of autoimmune hepatitis is prescribed by a doctor; it is usually long-term and depends on the severity of the disease.
Publications in the media
Chronic viral hepatitis (CVH) is a chronic infectious disease caused by hepatotropic viruses; are characterized by a clinical and morphological picture of diffuse liver inflammation (lasting more than 6 months) and a symptom complex of extrahepatic lesions.
Etiology and epidemiology • CHV B (HBV infection). The causative agent is a DNA virus. The main route of transmission is parenteral, as well as through damaged mucous membranes and skin (perinatal, sexual contact, close household contact [shared razor, toothbrush, etc.]). At risk are drug addicts who inject drugs intravenously, homosexual men and persons in contact with blood and its products (for example, patients and medical personnel in surgery departments, hematology and hemodialysis centers). The incubation period is 1–6 months. Approximately 10% of patients experience a chronic course or long-term carriage of • CHV C (HCV infection). Previously, this hepatitis was designated by the term non-A non-B hepatitis, transmitted by the parenteral route. The causative agent is an RNA virus (HCV); isolated in 50–90% of cases of post-transfusion hepatitis. The routes of transmission (parenteral, sexual and possibly perinatal) are similar to those for chronic hepatitis B. The incubation period is from 2 weeks to 6 months. The chronic variant is observed in 30–50% and even 75% of patients (approximately 50% suffer from chronic active hepatitis); a significant proportion of patients develop cirrhosis of the liver • CHV D (HDV infection). The causative agent is a small defective RNA virus (HDV), d-virus); it is contagious only when infected with HBV (since, due to the incomplete genome, it uses HBV proteins for replication). The main route of transmission is parenteral (therapeutic and diagnostic procedures), as well as sexual and perinatal. The epidemiological significance of d-infection is great in regions where anti-d and HBS-Ag carriage is endemic. d-Infection exists in the form of acute infection with simultaneous infection with HBV and d-virus (co-infection) and acute infection with d-virus infection of HBV carriers or patients with chronic hepatitis B (superinfection). CVH D is characterized by a chronic, severe course • CVH E. The causative agent is an RNA virus isolated from patients with acute hepatitis in Mexico, Asia and Africa; outbreaks are observed in the CIS. The main mechanism of transmission is fecal-oral, the leading factor of transmission is infected water. People aged 15–40 years are affected. The incubation period is 15–45 days (average 40 days). The fulminant (fulminant) form of hepatitis is often registered in the 2nd–3rd trimester of pregnancy. Mortality among pregnant women can reach 10–20% • CHV G is classified as hepatitis transmitted parenterally; The disease is transmitted after a blood transfusion or organ transplant; the majority of those affected are adults. Giant multinucleated cells (syncytial giant cell hepatitis) are found in the liver. The virus was not isolated from liver biopsies; clinical and laboratory symptoms were not expressed. Hepatitis G is currently classified as non-A, non-B, non-C hepatitis.
Risk groups • Medical workers • Drug addicts • Recipients of blood and blood products (including patients with cancer and immunodeficiency conditions) • Newborns from mothers infected with HBV and HCV • Family members of persons infected with HBV and HCV • Patients on hemodialysis .
Clinical picture
• Signs of liver damage •• Active process - the liver is enlarged, dense, the edge is pointed, palpation is painful. With a decrease in activity, the size of the liver decreases, palpation is less painful (the consistency does not change significantly). Hepatomegaly is absent in patients with cirrhosis of the liver •• Pain in the liver area (the symptom is not constant, if present, the pain is constant, aching, sometimes intense, intensifies after physical activity) with an active process, with the subsidence of inflammatory phenomena - a decrease in the intensity of the pain syndrome •• Jaundice (parenchymal and secondary mechanical) is often accompanied by itchy skin, and scratches are found on the skin. Often CVH occurs without jaundice •• Telangiectasia and palmar erythema are caused by an increase in the concentration of estrogen and a change in the sensitivity of vascular receptors (opening and expansion of arteriovenous shunts). Their severity correlates with the activity of the process and does not indicate cirrhosis of the liver. Improvement in the functional state of the liver is accompanied by a decrease in the number of spider veins or their disappearance, hyperemia of the palms remains much longer (often until biochemical remission) •• Splenomegaly - with cirrhosis of the liver •• Dyspeptic syndrome (impaired detoxification function of the liver, concomitant pathology of the duodenum and pancreas ): nausea, worse after eating and taking drugs, vomiting, bitterness in the mouth, belching, diarrhea. Also, regardless of food intake, a feeling of heaviness and fullness in the right hypochondrium and epigastric regions is observed •• Asthenic syndrome: weakness, fatigue, decreased performance, irritability, decreased mood •• Amenorrhea, gynecomastia, decreased libido, associated with impaired metabolism of sex hormones in the liver •• Varnished tongue •• Minor liver failure syndrome: drowsiness, thrombohemorrhagic syndrome (bleeding and bruising on the skin, bleeding gums, nosebleeds, hematuria, uterine bleeding, etc.), transient jaundice and ascites; the syndrome is characteristic of an active inflammatory process in the liver •• Loss of body weight •• Increase in body temperature to subfebrile values.
• Extrahepatic manifestations •• Arthritis, arthralgia, polymyalgia •• Periarteritis nodosa •• Carditis •• Lung lesions: fibrosing alveolitis, pulmonary vasculitis, granulomatosis •• Pancreatitis •• Sjogren's syndrome •• Kidney damage: glomerulonephritis •• Skin lesions: late cutaneous porphyria, papular acrodermatitis (Gianotti-Crosti syndrome) •• Lesions of the endocrine system: autoimmune thyroiditis, ovarian dysfunction •• Raynaud's syndrome •• Damage to the nervous system: polyneuropathy, Guillain-Barre syndrome •• Secondary mixed cryoglobulinemia •• Hypoplastic or aplastic anemia.
Laboratory research. Biochemical blood test: increased ESR, hyperproteinemia, dysproteinemia (increased g-globulin content, increased thymol test, decreased blood albumin, decreased mercuric test), increased ALT and AST activity, increased conjugated (direct) bilirubin.
Serological studies
• Determination of CVH markers with the establishment of virus replication activity (in ELISA reactions, DNA hybridization, PCR). • HBV infection •• HBs-Ag (surface (Australian) HBV Ag) marks infection with the virus; appears in the blood 1.5 months after infection •• Ag Pre-S region HBs (Pre-S1 and Pre-S2) appear simultaneously or slightly earlier than HBsAg; mark an actively ongoing infection •• HBc-Ag (nuclear c-Ag) marks the replication of the virus in hepatocytes; discovered only during morphological examination of biopsy specimens or autopsy material of the liver; is not detected in free form in the blood •• HBe-Ag nuclear e-Ag (secretory part of HBc-Ag) indicates virus replication in hepatocytes; appears in serum almost simultaneously with HBs-Ag; may be absent in case of HBV infection caused by a mutant strain of the virus •• Anti-HBc (AT to nuclear Ag) is an important diagnostic marker of infection, especially with negative results of HBs-Ag indication •• Anti-HBc IgM (AT-immunoglobulins of class M to nuclear Ag ) is one of the earliest serum markers of chronic hepatitis B; the most sensitive marker of HBV infection; marks the replication of the virus and the activity of the process in the liver; its disappearance serves as an indicator of either the sanitation of the body from the pathogen, or the development of the integrative phase of HBV infection •• Anti-HBc IgG (AT-immunoglobulins of class G to nuclear Ag) persist for many years; indicate an existing or previously suffered infection •• Anti-HBe (AT to e-Ag) is a serological marker of virus integration; in combination with anti-HBc IgG and anti-HBs indicate the complete completion of the infectious process •• Anti-HBs (protective antibodies to surface Ag) indicate protection against infection; are formed during the vaccination process; may indicate the completion of a viral infection •• Anti-Pre-S (ATs to Pre-S1Ag and Pre-S2Ag) indicate the development of protective immunity at the completion of the infectious process; anti-PreS1 is registered simultaneously with anti-HBc, and anti-PreS2 - in the period of convalescence (evidence of recovery) •• HBV-DNA (HBV DNA) and DNA polymerase are diagnostic markers of virus replication •• HBV replication markers - HBe-Ag, anti-HBeAg IgM, HBV-DNA, HBV-DNA polymerase.
• HCV infection •• Anti-HCV (Ab to hepatitis C virus) appear in the blood within 6 months after infection (on average 3 months); indicate possible infection with the virus or a previous infection •• HCV RNA (HCV RNA) is a diagnostic marker of virus replication •• Markers of HCV replication are anti-HCV IgM and HCV RNA.
• HDV infection •• HDV-Ag (HDV Ag) - appears in the blood 3 weeks after infection; marks viral replication •• Anti-HDV IgM (class M antibody to hepatitis D virus) is considered a more reliable marker of HDV infection than HDV-Ag; indicate viral replication; recorded with high frequency during HDV superinfection as the most common cause of CHV D •• HDV-RNA (HDV RNA) is a diagnostic marker of virus replication •• Markers of HDV replication are anti-HDV IgM, HDV RNA.
Special methods • Ultrasound of the liver and spleen: increased echogenicity of the parenchyma, compaction along the liver vessels, with cirrhosis of the liver - splenomegaly • Radioisotope study of the liver: significant increase in cardioportal time (the time between peaks of activity above the heart and above the liver), enlarged liver, uneven accumulation of radiopharmaceuticals along the edges (fuzzy contours) • Laparoscopy: large compacted white or variegated liver with a pointed edge and a vague pattern of lobules, enhanced pattern of superficial vessels • Liver puncture biopsy: degeneration and necrosis of hepatocytes, lymphomacrophage infiltration and proliferation of connective tissue in the hepatic lobules. Changes are assessed using semi-quantitative methods (histological activity index according to RG Knodell et al and degree of fibrosis according to VJ Desmet et al.). Data from laparoscopy and liver puncture biopsy correlate with each other.
Differential diagnosis • Autoimmune hepatitis • Chronic drug-induced hepatitis • Primary biliary cirrhosis • Primary sclerosing cholangitis • Infectious mononucleosis • Primary and secondary liver tumors • Ischemic hepatitis • Chronic alcoholic hepatitis • Wilson's disease.
Treatment
• Etiotropic: IFN preparations (parenteral forms of natural and/or recombinant a- and b-IFN) - with a high degree of activity of the infectious process (presence of replication markers), as well as with extrahepatic lesions. The effectiveness of treatment is 20–60%.
• Criteria for the effectiveness of IFN treatment •• disappearance of HBV, HCV, HDV replication markers •• normalization of ALT and AST indicators •• improvement of the histological picture of the liver •• reduction or disappearance of symptoms of extrahepatic lesions.
• For chronic HBV infection, IFN is most effective in the presence of the following symptoms •• young age •• female gender •• onset of the disease in adulthood •• duration of the disease up to a year •• icteric form of the manifest manifestation of the disease •• high levels of ALT and AST in the serum blood •• low level of HBV-DNA (less than 200 pg/ml) •• absence of super- and coinfection with hepatitis C, D, G viruses, HIV infection, immunosuppressive therapy, renal failure, signs of cirrhosis.
• For chronic HCV infection, IFN is most effective in the presence of the following signs •• young age •• parenteral route of infection •• low concentration of HCV RNA •• HCV genotype 2a, 3, 4 (not 1b) •• normal iron content in the tissue liver and blood serum •• relatively short duration of the disease •• weakly expressed autoimmune component of inflammation •• absence of signs of cirrhosis, cholestasis.
• Chronic HDV infection is resistant to IFN therapy.
• Treatment regimens with IFN drugs •• For HBV infection ••• Recombinant a-IFN (interferon alpha-2b, for example, intron A) - 2.5–5 million (children up to 5–6 million) IU/m2 daily or 3 times/week subcutaneously or intramuscularly for 6 months ••• Natural a-IFN (interferon alpha-n1) 10 IU 3 times/week (for children - up to 10 IU/m2) for 12 weeks •• With HCV infections ••• Intron A 3 million IU/m2 3 times a week for 12–18 months ••• Interferon alpha-n1 3–5 IU 3 times a week for 48 weeks •• For HDV infection it is recommended intron A 5 million IU daily or 9–10 million IU 3 times a week for 12 months.
• Ways to increase the effectiveness of treatment with IFN drugs •• Combination with antiviral drugs with a different mechanism of action (for example, ribavirin) •• With low activity of the HBV replication process - preliminary treatment with prednisolone (for example, 30 mg / day for 3 weeks, then 15 mg/day for 1 week, then after 2 weeks treatment with IFN) •• For cholestasis, ursodeoxycholic acid is prescribed •• If the iron content in the liver tissue increases, bloodletting, antioxidants are prescribed.
Prevention • Prevention of the spread of infections transmitted parenterally (monitoring biological preparations for the presence of markers of viral replication, using disposable medical instruments, etc.).
Abbreviations • RFP - radiopharmaceutical • CHV - chronic viral hepatitis
ICD-10 • B18 Chronic viral hepatitis
Diagnosis of the disease
Diagnosis of chronic viral hepatitis is based primarily on laboratory methods, since in the early stages the disease is often asymptomatic.
First of all, to confirm the cause of the disease, a blood test for specific markers of viral hepatitis is necessary. These are antigens of the hepatitis B or C virus (viral particles) and antibodies produced by the body in the fight against it. In addition to the qualitative determination (detection) of the antigen, it is also necessary to study the level of viral load (the amount of antigen in a certain volume of blood). This makes it possible to judge the activity of virus reproduction and determine indications for antiviral therapy.
To assess liver function, a biochemical blood test is recommended, which includes determining the level of liver enzymes, bilirubin, protein, protein fractions and other indicators. The doctor gives more specific recommendations based on the individual picture of the course of the disease.
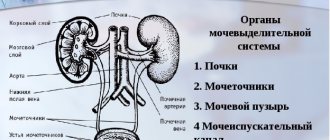
To assess the size and structure of the organ, abdominal ultrasound is recommended: this is the simplest method of visualizing the liver.
To determine the degree of fibrosis, fibroelastography or liver biopsy can be performed - sampling a small amount of liver tissue under ultrasound guidance for further examination under a microscope.
Toxic hepatitis
Drug-induced hepatitis, as one of the common types of toxic hepatitis, can be caused by a variety of medications. In particular, anti-tuberculosis drugs (isoniazid, rifampicin), hormonal contraceptives, tetracycline antibiotics, as well as drugs such as methyldopa, zidovudine, ketoconazole, paracetamol, indomethacin and many others. Moreover, which particular drug will cause toxic liver damage largely depends on the individual sensitivity of the particular patient.
Prevention of drug-induced hepatitis
is the use of medications in strictly prescribed dosages by a doctor. If the drug can have a negative effect on the liver, it is necessary to periodically take a biochemical blood test. If there are deviations from the norm, the doctor may recommend hepatoprotectors.
Alcoholic hepatitis
This is the main form of liver damage that occurs in patients with alcoholism, which develops due to the systematic long-term destructive effects of alcohol and its breakdown products (for example, acetaldehyde) on liver cells.
The severity and speed of development of the disease is directly dependent on the quantity and quality of alcohol consumed, as well as on the initial state of health of the patient and concomitant pathology.
Alcoholic hepatitis can occur in both acute and chronic forms, which often develop into severe cirrhosis of the liver with possible degeneration into a malignant tumor - carcinoma.
Other toxic hepatitis
The most severe forms of toxic hepatitis develop from poisoning with toadstool poison, white phosphorus, carbon tetrachloride, and some industrial poisons. In these cases, immediate hospitalization of the patient and treatment with detoxification and hepatoprotective agents are required.