Pharmacodynamics and pharmacokinetics
Pharmacodynamics
Metabolic drug that has antihypoxic and trophic effects. This high molecular weight compound is obtained by extraction from myocardial of pigs or cattle. Its structure is similar to hemoglobin and plays a major role in redox processes in the body. The mechanism of action is associated with the presence of iron in the molecule, during the transition of which from one state to another, reactions and metabolic processes are accelerated, tissue hypoxia
It has high activity against superoxide, which is a strong oxidizing agent - cytochrome neutralizes oxygen radicals and acts as a “trap”. Inhibition of oxygen radicals in the lens of the eye is important in preventing the development of cataracts .
Pharmacokinetics
Completely absorbed and penetrates into the cells of all tissues.
The role of the cytochrome P450 system in the human body
Metabolism of drugs in the liver occurs in two stages. The first stage of biotransformation occurs under the action of cytochrome P450 , monooxygenase and cytochrome C reductase . As a result of oxidative reactions, polar groups and metabolites are formed. Cytochrome P450 plays an important role in oxidative processes, since the cytochrome system does most of this work. This system is represented by proteins that begin metabolism in the small intestine, but most of it occurs in the liver.
Cytochrome isoenzymes are presented in more than 55 forms and each is capable of metabolizing several drugs that are suitable for its structure. This creates the basis for the interaction of drugs entering the body at the same time, and knowing this, severe adverse drug reactions can be prevented. Here are some examples of drug interaction. Drugs that increase enzyme activity are called stimulants. For example, rifampicin , carbamazepine , phenytoin are strong stimulants of the cytochrome system , and a drug taken at the same time and metabolized by this system will be quickly eliminated from the body without exerting its effect. Therefore, these drugs should not be taken together.
There is another type of interaction when, along with one medicine, a person uses another - a cytochrome (for example, antidepressants , ketoconazole , fluoroquinolones , omeprazole , cimetidine , metronidazole , chloramphenicol and many others). At the same time, its metabolism slows down, its half-life increases, and the risk of overdose and the development of adverse reactions increases.
The role of the cytochrome P450 family in the pathogenesis and treatment of NAFLD
Oksana Mikhailovna Drapkina , professor, doctor of medical sciences:
– We continue our program. Our lectures and discussions on gynecology are ending, we have completely entered into the regulations, so we will try not to leave them. Professor Tatyana Evgenievna Polunina opens the section of gastroenterology. Lectures “The role of the cytochrome P450 family in the pathogenesis and treatment of non-alcoholic fatty liver disease.”
Tatyana Evgenievna Polunina , professor, doctor of medical sciences:
– Cytochromes P450 (CYP 450) is the name of a large family of universal enzymes in the human body. Cytochromes P450 play an important role in the oxidation of numerous compounds, such as endogenous compounds (steroids, bile acids, fatty acids, prostaglandins, leukotrienes, biogenic amines), as well as exogenous compounds (drugs, industrial pollution, pesticides, carcinogens and mutagens), the latter are called xenobiotics.
In this slide you can see where the cytochromes P450 are located. They are located in the hepatocyte, in the cytosol. The endoplasmic reticulum is the basis for the location. And, in particular, the lipid membrane, which contains a bilayer of phospholipids, has several connected structures on it. This is a cytochrome, which includes iron protein, nicotinamide adenine dinucleotide and oxidoreductase, which is included in the complex of metabolism of drugs and the above presented xenobiotics.
The most common representatives of this group that clinicians turn to are cytochromes P452 AC, P450 2D, P450 2E1, P450 3A4. These enzymes catalyze a wide range of metabolic reactions and one cytochrome can metabolize several drugs that have different chemical structures. The same drug has different effects in cytochrome P450 and in different organs. And, in particular, the most important cytochrome that we pay attention to is cytochrome P450 2E - the most important isoenzyme of cytochrome P450, it breaks down low-density lipoproteins.
Currently, not only phenotyping methods have been developed that are based on the substrate specificity of certain cytochrome P450 isoenzymes, but also the activity of a particular enzyme and metabolism is determined by the pharmacokinetics of the marker substrate and changes in the concentrations of the unchanged substance and its metabolite. But the determination of cytochrome P450 isoenzymes by identifying the genes for the corresponding isoenzymes is carried out using a polymerase chain reaction. This is called cytochrome P450 isoenzyme genotyping.
On this slide we see that in the hepatocyte the place where the endoplasmic reticulum, cytochromes P450, of which there are more than 50, and drugs that are broken down in a certain cytochrome are located, in some cases it combines with the cytochrome and forms a vesicle that damages the hepatocyte, causing at the same time stress and cytokines; leads to activation of the tumor necrotic factor and, in particular, is a trigger factor for the launch of caspases, which manifests itself with catalytic processes.
Non-alcoholic fatty liver disease, which was subsequently identified as a nosological entity, began to be called non-alcoholic fatty liver disease (NAFLD) since 1980, after discovering changes in the liver of non-alcoholic patients that were similar to those seen in alcohol-induced damage.
The natural history of non-alcoholic fatty liver disease includes steatosis as an initial stage, which, without progressing, can be asymptomatic, and steatohepatitis, which is accompanied by terrible vegetative manifestations, cytolysis syndrome and dyspeptic manifestations. With the development of fibrosis, a rather serious problem arises - liver cirrhosis, and subsequently portal hypertension and carcinoma develop.
I would like to draw your attention to the fact that back in 1894, Kiernan proposed a certain liver architecture, which consists of a beam structure. On the periphery of the beams, which consist of polygonal hepatocytes, there is a triad: bile duct, portal vein and artery. This slide represents a normal healthy liver and fatty infiltration of hepatocytes. Liver steatosis, which is one of the first phases of development of non-alcoholic fatty liver disease, is presented in morphological form in this diagram.
The next option for the development of the inflammatory process, which leads to fibrous tissue spreading throughout the liver, we see steatohepatitis and subsequently cirrhosis of the liver with the development of portal hypertension. Most often, this is micronodular cirrhosis of the liver, which is already quite clearly established in the stages of development of non-alcoholic fatty liver disease, it is accompanied by portal hypertension, varicose veins of the esophagus, stomach, complications that are typical for cirrhosis of the liver, and death.
With non-alcoholic steatohepatitis, the most common developments are those that are most often associated as concomitant diseases: diabetes mellitus, obesity. In patients, non-alcoholic steatohepatitis develops up to 75%, and if diabetes mellitus and obesity are combined, then 90% of patients have non-alcoholic fatty liver disease.
The liver is undoubtedly the main target organ affected by metabolic syndrome. Insulin resistance is a key feature that is the basis for intrahepatocyte lipid accumulation, fatty liver, non-alcoholic steatohepatitis and liver cirrhosis.
I would like to draw attention to the fact that metabolic syndrome includes not only impaired glucose tolerance, but also dyslipidemia, abdominal-visceral obesity, insulin resistance and hyperinsulinemia, arterial hypertension, early atherosclerosis, impaired hemostasis, hyperuricemia, hyperandrogenism. I would like to say that non-alcoholic fatty liver disease, steatosis, is part of the metabolic syndrome and is currently a quintet that used to be called the “deadly quartet”.
The risk factors presented on this slide sometimes vary from country to country, with US positions and European positions differing slightly. But, nevertheless, waist circumference, levels of triglycerides, lipoproteins, blood pressure, in particular 130/85, glucose levels are indicators that must be monitored in a patient with metabolic syndrome.
Diseases associated with lipid metabolism are: non-alcoholic fatty liver disease, type 2 diabetes mellitus, coronary liver disease, hypertension.
In the pathogenesis scheme, insulin resistance of adipose tissue is of particular importance. An increase in lipogenesis, that is, an increase in the level of fatty acids, an increase in the synthesis of triglycerides and lipotoxicity lead to the development of insulin resistance, and this leads to metabolic dysfunction, stress of the endoplasmic reticulum, in which the metabolism of fatty acids and in particular lipoproteins also occurs, and to the activation of inflammation . These are Kupffer cells and stellate cells, which further lead not only to the fact that the level of very low density lipids increases, but undoubtedly this leads to the development of steatohepatitis with fibrosis, and we get the activity of a process that moves towards cirrhosis of the liver.
At the hepatocyte level, fatty acids undergo esterification into triglycerides and are exported as low-density lipoproteins, a situation in the normal hepatocyte that is associated with oxidation in mitochondria, peroxisomes and microsomes.
Undoubtedly, in the mechanism of insulin resistance, which is presented here, a key role belongs to the tumor necrotic factor, free radicals, leptin, fatty acids and increased lipolysis, which leads to the absorption of fatty acids, to a violation of β-oxidation of fatty acids in mitochondria and also to the accumulation of fatty acids in hepatocyte.
Induction of cytochromes P450 4A11 and P450 2E1 leads to lipid peroxidation, which undoubtedly leads to the activation of factors associated with the accumulation of triglycerides. Hyperinsulinemia is a key factor that leads to insulin resistance. It also leads to an increase in glycolysis, fatty acid synthesis and triglyceride accumulation in hepatocytes.
The next slide shows the mechanism of interaction between microsomal oxidation and mitochondrial β-oxidation. Note that mitochondrial Ω-oxidation and mitochondrial β-oxidation lead to the triggering of so-called peroxisomal β-oxidation receptors and in particular peroxisome proliferator-activated receptors. This leads to the expression of the accumulation of a certain protein and, accordingly, acetyl-coenzyme A, which accumulates and triggers a mechanism that leads to an overload of dicarboxylic fatty acids.
In the next slide you see that steatohepatitis and fibrosis are formed against the background of mitochondrial reactive oxygen species. The key to triggering fibrosis is undoubtedly the accumulation of malondialdehyde, which leads to the formation of inflammatory infiltrates, fibrosis and activation of stellate cells. Stellate cells trigger the induction of cytokines such as tumor necrotic factor and transforming growth factors. Depletion of the antioxidant system leads to the launch of Fas-legand, a mitochondrial reactive oxygen species, hepatocyte necrosis occurs, and fibrous tissue subsequently develops, which is the basis for the development of cirrhosis.
This slide shows a diagram; you see excess lipids that accumulate in the hepatocyte. Mitochondrial dysfunction and dysfunction of cytochrome P450 leads to activation of lipid peroxidation, the launch of Kupffer cells, inflammatory cytokines, activation of stellate cells and apoptosis, which subsequently leads to the development of hepatocyte necrosis.
Metabolic syndrome is very important because non-alcoholic fatty liver disease is part of the metabolic syndrome. And not only on the hepatocyte, in which there is an increase in the level of low-density and very low-density lipoproteins, triglycerides (this is very important), but also on the endothelial cell. Endothelial dysfunction occurs and a moment is also triggered that is associated with lipid peroxidation, the accumulation of substances that affect atherosclerosis, sudden death, and heart attacks.
Undoubtedly, the increase in free fatty acid levels is associated with adipocytes. And a decrease in esterified cholesterol in particular also leads to various stresses of the nuclear receptor. And the so-called activated peroxisome proliferator receptor is especially important at present; it is to it that all the attention of scientists who work with obesity, diabetes, and non-alcoholic fatty liver disease is directed.
A monocyte (macrophage), in some cases, by increasing the level of inflammatory responders (tumor-necrotic factor, interleukins-6, membrane toll-like receptors, free fatty acids) also triggers events that are associated specifically with the pathological effects of fatty acids.
The criteria for assessing insulin resistance have been known to everyone since 1985. It is determined by the HOMA index - Homeostasis Model Assessment, and the more modern QUICKI index - Quantitave Insulin Sensitivity. Insulin concentration, serum glucose, and norms are presented here.
We would like to point out that not all patients with non-alcoholic fatty liver disease need a liver biopsy. We currently have points that enable us to determine the level of fatty infiltration of the liver. And in particular this is a fibrotest.
In the algorithm for diagnosing non-alcoholic fatty liver disease, we pay attention not only to specific signs, but also to the activity of the enzymes alanine and aspartic transaminase, gamma-glutamyl transpeptidase, alkaline phosphatase, and we pay attention to alcohol intake, which was discussed by previous colleagues. And I would like to draw attention, of course, to risk factors: metabolic syndrome, insulin resistance, diabetes. Therapy is prescribed to correct this situation, and, if necessary, a liver biopsy. Undoubtedly, absolute indications for biopsy are required. And if the body mass index exceeds 35 and 40, then measures related to surgical treatment are already being carried out.
I would like to draw your attention to a number of medications (non-steroidal - anti-inflammatory glucocorticosis, and steroid drugs, tetracycline antibiotics), a number of nutritional factors (fasting, rapid weight loss, surgical interventions, metabolic genetic factors, in particular, hereditary hemochromatosis, various poisons) and other concomitant diseases. This is very important for differential diagnosis.
At the stage of steatosis, treatment of obesity, insulin resistance, and dyslipidemia is important. In the stage of steatohepatitis, the most important point is the elimination of oxidative stress, inflammation and fibrosis.
Excessive induction of cytochrome P450 2E has detrimental effects on hepatocytes due to the release of free radicals. Essential phospholipids act not only as antioxidants, but also serve as a very important factor for reducing the activity of cytochrome 2E1, as shown in the works of M. Aleynik. The results of some studies suggest that the introduction of essential phospholipids can reduce the induction of cytochrome P450 2E (work by Vladimir Trofimovich Ivashkin, who was presented with Marina Viktorovna Mayevskaya in Russian sources in 2004).
Stellate cells take part in the formation of the final stage of non-alcoholic fatty liver disease. And in laboratory experiments, it has been demonstrated that complete prevention of stellate cell activation using CYP2E1 inhibitors prevents the development of cirrhosis.
I would like to draw your attention to the fact that not only the Russian author M. Aleynik, but also the Japanese author Akiyama in the journal “Hepatology” in 2009, based on a model of alcoholic liver damage, also pays attention to cytochrome P450 2E, acetyl-CoA oxidase and nicotinamide adenine dinucleotide oxidases, that essential phospholipids exhibit anti-inflammatory, anti-apoptotic and anti-fibrotic activity in this pathology.
This is a theoretical version of the assumption of the use of cytochrome P450 inhibitors, and in particular the drug “Essentiale”, which is the reference, and is the most important point for the inhibition of cytochromes P450 2E and, accordingly, P450 4A11. This prevents lipid oxidation, glycolysis and reduces fatty acid synthesis.
The following drugs are used in the treatment of non-alcoholic fatty liver disease: insulin sensitizers, antioxidants, hepatoprotectors, antimicrobials.
But I would like to draw attention to membrane phospholipids. They are the main lipid components of cell membranes. Damage to phospholipid membranes leads to cytolysis syndrome, and excess reactive oxygen species leads to damage to phospholipid membranes based on microsomal γ-oxidation and peroxymal β-oxidation. Accordingly, damage to phospholipid membranes results in cell death, which leads to the initiation of fibrosis and activation of stellate cells.
Damage to the liver structure is damage to the membranes. In the version of essential phospholipids, it is a material that restores cell membranes instead of lipids. Restoring the liver structure makes it possible to restore liver function.
Our patients suffer not only from alcoholic fatty liver disease, alcoholic hepatitis, but also from other liver diseases, this is an indisputable fact. I would like to draw your attention to the fact that according to E. Kunz (2008 monograph), essential phospholipids have an antifibrotic effect, an effect that stabilizes bile and the hepatocyte membrane.
This is a publication that was released in 2008 based on pharmacological and clinical data. Therapy with essential phospholipids seems to be the preferred choice for significantly reducing the manifestations and eliminating fatty liver disease of various etiologies, which has developed due to alcohol consumption, obesity, and even if the cause cannot be discerned.
I would like to point out that there are several studies on Essential. These studies are well known to everyone. But I would like to say that even with diabetes mellitus, Essentiale makes it possible to normalize the level of glucose, glycated hemoglobin, and serum cholesterol in patients with non-alcoholic liver disease.
In conclusion, I would like to say that liver damage characterized by fat accumulation in the absence of alcohol abuse is known as non-alcoholic fatty liver disease. Risk factors include obesity and type 2 diabetes. In the pathogenesis of non-alcoholic fatty liver disease, particular importance is given to the excessive activity of cytochromes P450 2E1. Clinical variants of the course of the disease: pain in the right hypochondrium, asthenovegetative and dyspeptic disorders, hepatomegaly. And our diagnostic algorithm is based on the consistent exclusion of alcoholic and iatrogenic, as well as viral liver damage.
When analyzing laboratory and instrumental studies, the syndromes of cytolysis and cholestasis are very important. Fatty liver degeneration based on the results of a morphological study is an expert assessment. Treatment requires weight loss, long-term use of insulin sensitizers, antioxidants and hepatoprotectors “Essentiale N” in a dose of 5-10 ml intravenously, switching to a tablet form, two capsules three times a day. Undoubtedly, it is difficult to lose weight, but it is necessary to correct the function of the liver and other organs.
Thank you for your attention.
Indications for use
Injection:
- asphyxia of newborns;
- poisoning with sleeping pills, alcohol and drugs;
- viral hepatitis with hepatic coma ;
- ischemic and dystrophic lesions of the myocardium ;
- bronchial asthma with respiratory failure;
- pneumonia;
- chronic circulatory failure;
- severe injuries;
- cerebrovascular accidents;
- respiratory failure;
- operations on the chest.
Eye drops:
- corneal dystrophy;
- keratitis;
- corneal clouding.
Cytochrome C, instructions for use (Method and dosage)
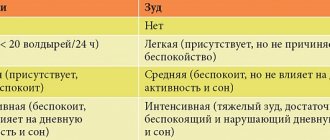
The drug Cytochrome C is administered intravenously or intramuscularly. Before using the drug, it is necessary to check your sensitivity to it. To do this, inject 0.1 ml intradermally and wait 30 minutes. If there is no reaction ( hives , facial redness, itching), you can start injections. The dose is 10-20 mg 1-2 times a day. Treatment is carried out for 14 days.
For heart failure - 20 mg intravenously over 6-8 hours, diluted in 200 ml of saline. The daily dose ranges from 30 mg to 80 mg.
In the period after heart surgery - 10 mg intravenously 2 times a day.
For hepatic coma , shock, poisoning - 50-100 mg intravenously.
For asphyxia in newborns, 10 mg is injected into the umbilical vein immediately after birth.
For bronchial asthma - intramuscularly 5-10 mg 2 times a day.
Before conducting a repeat course, a biological test is done.
Function
In the mitochondria of eukaryotes and aerobic prokaryotes, cytochrome b is a component of the respiratory chain complex III (1.10.2.2) - also known as the bc1 complex or ubiquinol-cytochrome c reductase. Plant chloroplasts and cyanobacteria contain a similar protein, cytochrome b6, a component of plastoquinone plastocyanin reductase (1.10.99.1), also known as the b6f complex. These complexes are involved in electron transfer, pumping protons to create proton motive force (PMF). This proton gradient is used to generate ATP. These complexes play vital roles in cells.[3]
Reviews about Cytochrome C
There are no reviews about this drug, since it is used in the complex treatment of hypoxic conditions or to prevent them. Therefore, it is not possible to draw a conclusion about the effectiveness of this drug. You can only trust experimental and clinical studies. For example, this drug was included in intensive therapy of the postoperative period for patients who underwent heart valve replacement. Infusion of the drug at a dose of 0.5 g/kg was carried out before surgery and again immediately after surgery. It was concluded that it has antihypoxic and anti-ischemic effectiveness. It increases the capabilities of the heart muscle in conditions of ischemia , improves coronary blood flow and contractile function. It has proven to be an effective cardioprotector in open heart surgery.
The experience of using this drug in the acute period of myocardial infarction . Good results are available with intravenous administration of this drug (even a single dose) in a dose of 50-100 mg for carbon monoxide .
The antioxidant properties of the drug are used in the complex treatment of diabetic neuropathy , to normalize gas exchange in the mother-fetus system in case of fetoplacental insufficiency.