Coprogram is a comprehensive analysis of feces, which allows you to evaluate the functioning of the digestive system as a whole, and the functionality of each organ separately. In order for the research results to be accurate, it is necessary to adhere to certain rules for the preparation, collection and storage of material.
What is a coprogram?
Coprogram is a method of laboratory examination of feces, which is prescribed to identify pathologies of the digestive system. The specialist conducts macroscopic, microscopic, chemical and physical analysis of feces, after which he makes a detailed description of the composition of feces.
What a general stool analysis shows:
- dysfunction of the pancreas, intestines, stomach;
- the presence of foci of inflammation in the gastrointestinal tract and their localization;
- disruptions in the process of digestion, movement of feces, and absorption of nutrients;
- dysbacteriosis;
- presence of parasites;
- colitis.
You can make a stool coprogram in a regular clinic for free, but to get a more accurate and detailed result, it is better to contact private laboratories, the average price is 370–420 rubles.
Norms
Macroscopic examination
| Parameter | Norm |
| Quantity | A healthy person produces an average of 100-200 g of feces per day. Normally, feces contain about 80% water and 20% dry matter. With a vegetarian diet, the amount of feces can reach 400-500 g per day; when using easily digestible food, the amount of feces decreases. |
| Consistency | Normally, formed feces have a dense consistency. Pasty feces can occur normally and are caused by the intake of predominantly plant foods. |
| Form | Normally cylindrical. |
| Smell | Normally, stool has a mild odor, which is called fecal (ordinary). It may intensify with the predominance of meat products in the diet, with putrefactive dyspepsia and weaken with a dairy-vegetable diet, constipation. |
| Color | Normally, stool is brown in color. When eating dairy foods, stool turns yellowish-brown, and meat stool turns dark brown. Ingestion of plant foods and some medications can change the color of stool (beets - reddish; blueberries, blackcurrants, blackberries, coffee, cocoa - dark brown; bismuth, iron color stool black). |
| Slime | Normally absent (or in scanty quantities). |
| Blood | Normally absent. |
| Pus | Normally absent. |
| Leftover undigested food (lientorrhea) | Normally none. |
Chemical research
| Parameter | Norm |
| Fecal reaction | Normally neutral, less often slightly alkaline or slightly acidic. Protein nutrition causes a shift in the reaction towards the alkaline side, while carbohydrate nutrition causes the reaction to shift towards the acidic side. |
| Reaction to blood (Gregersen reaction) | Normally negative |
| Reaction to stercobilin | Normally positive. |
| Reaction to bilirubin | Normally negative. |
| Vishnyakov-Triboulet reaction (for soluble protein) | Normally negative. |
Microscopic examination
| Parameter | Norm |
| Muscle fibers | Normally absent or single in the field of view. |
| Connective tissue (remnants of undigested vessels, ligaments, fascia, cartilage) | Normally absent. |
| Fat is neutral. Fatty acid. Salts of fatty acids (soaps). | Normally there are no or scanty amounts of fatty acid salts. |
| Plant fiber | Normally, there are single cells in the p/z. |
| Starch | Normally absent (or single starch cells). |
| Iodophilic microflora (clostridia) | Normally, single in rare areas (normally, iodophilic flora lives in the ileocecal region of the large intestine). |
| Epithelium | Normally, there are no or single columnar epithelial cells in the p/z. |
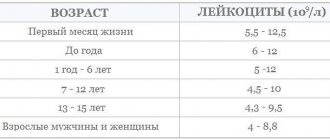
| Leukocytes | Normally, there are no or single neutrophils in the p/z. |
| Red blood cells | Normally none. |
| Worm eggs | Normally none. |
| Pathogenic protozoa | Normally none. |
| Yeast cells | Normally none. |
| Calcium oxalate (oxalic lime crystals) | Normally none. |
| Triple phosphate crystals (ammonium phosphate-magnesia) | Normally none. |
Indications for taking a coprogram
A stool test should be taken as part of an annual preventive examination in order to recognize problems with the digestive tract in time and begin treatment.
When is scatology prescribed:
- inflammation of the digestive system in acute and chronic form;
- hemorrhoids, fissures in the anus, chronic constipation;
- cirrhosis of the liver;
- irritable bowel syndrome;
- neoplasms in the gastrointestinal tract;
- poisoning;
- suspicion of helminthic infestation, amoebic dysentery;
- assessment of the effectiveness of drug treatment;
- before conducting instrumental diagnostics of the gastrointestinal tract and surgical interventions.
Children are prescribed a stool test for colic, if there is a suspicion of intestinal infections, inflammatory processes, cystic fibrosis, lactose intolerance, dysbacteriosis, or infection with worms.
Decoding indicators
Consistency Liquid feces may indicate overly active intestinal motility, colitis, or the presence of protozoal invasion.
Too tight stools indicate excessive absorption of fluid in the intestines, constipation, and dehydration.
Foamy stool occurs when the pancreas is insufficient or the secretory function of the stomach is impaired.
Pasty feces may indicate dyspepsia, colitis, or accelerated evacuation of feces from the large intestine.
Form
Pea-shaped feces occur with hemorrhoids, anal fissures, ulcers, fasting, myxedema (mucoedema).
Feces in the form of a thin ribbon are observed with stenosis of the small intestine, as well as in the presence of neoplasms in it.
Color
Black color (the color of tar) can be caused by eating certain foods (currants, chokeberries, cherries), taking medications with bismuth or iron, as well as bleeding in the stomach or duodenum, cirrhosis of the liver.
A red tint appears when there is bleeding in the large intestine.
Light brown stool color occurs due to liver failure or blockage of the bile ducts.
Light yellow stool occurs with pathologies of the pancreas and due to excessive consumption of dairy products.
Dark brown color indicates an excess of meat in the diet, as well as increased secretory function in the large intestine.
Green stool is a sign of typhoid fever.
Odor A putrid odor occurs due to the formation of hydrogen sulfide in the intestines and indicates the presence of ulcerative colitis or tissue breakdown, tuberculosis, putrefactive dyspepsia.
A sour smell indicates increased fermentation processes.
A foul odor indicates a malfunction of the pancreas, a lack of bile entering the intestines.
Acidity Increase pH
observed in formula-fed infants, in adults - with putrefactive dyspepsia, as well as with high activity of intestinal microflora.
Decrease in pH
occurs when the absorption process in the small intestine is disrupted, with excessive consumption of carbohydrates, or with increased fermentation processes.
Slime
Mucus can be found both on the surface of the stool and inside it; it is found in ulcerative colitis and constipation.
Blood Blood in the stool is detected during bleeding in the gastrointestinal tract caused by neoplasms, polyps, ulcers, hemorrhoids, and inflammatory processes.
Excessive amounts of bacteria and fungi can cause a false positive response.
Remains of undigested food Undigested food in the feces (lientorrhea) indicates a dysfunction of the pancreas, chronic gastritis, and accelerated peristalsis.
Undigested dietary fiber in stool analysis
Protein The presence of protein in stool indicates pathologies of the duodenum or stomach, colitis, enteritis, hemorrhoids and some other gastrointestinal diseases.
Stercobilin
The absence or significant decrease in stercobilin in the feces (the reaction to stercobilin is negative) indicates blockage of the bile duct or a sharp decrease in the functional activity of the liver. An increase in the amount of stercobilin in feces is observed with increased bile secretion and hemolytic jaundice.
Bilirubin The detection of bilirubin in the stool of an adult indicates a disruption in the process of its restoration in the intestine under the influence of microflora. This indicates intestinal dysbiosis, increased peristalsis, or taking antibacterial drugs during preparation for the test or shortly before.
Connective tissue and muscle fibers are undigested remains of meat and are found when there is a lack of pancreatic enzymes.
Fat Fat in the stool is one of the signs of insufficient pancreatic function or impaired bile secretion.
Excessive fat in stool (steatorrhea)
Plant fiber A large amount of digested plant fiber in the feces indicates the rapid passage of food through the stomach due to a decrease in its secretory function, the absence of hydrochloric acid in it, as well as an excess amount of bacteria in the large intestine and their penetration into the small intestine. Undigested fiber has no diagnostic value, since there are no enzymes in the gastrointestinal tract to break it down.
Starch An increased content of starch in feces, which appears when there is a lack of digestion processes in the stomach, small intestine and dysfunction of the pancreas, is called amilorrhea. Additionally, a lot of starch may be found during diarrhea.
Intracellular starch granules in stool analysis
Iodophilic flora (pathological) The presence of pathological microflora (staphylococci, enterococci, E. coli, etc.) indicates a decrease in the number of beneficial bacteria in the intestines and, accordingly, dysbacteriosis. When consuming large amounts of carbohydrates, clostridia begin to multiply intensively, causing fermentative dysbiosis.
Crystals
Calcium oxalate crystals in feces indicate insufficient stomach function, helminthic infestations, and allergies. Triple phosphate crystals indicate increased decay of proteins in the colon.
Epithelium
A significant amount of columnar epithelium in the stool is found in acute and chronic colitis. The presence of squamous epithelial cells has no diagnostic significance.
Leukocytes
Leukocytes in stool appear in cases of colitis and enteritis of the intestine, dysentery, and intestinal tuberculosis.
Red blood cells
Red blood cells appear in the feces during hemorrhoids, rectal fissures, ulcerative processes in the large intestine, and during the disintegration of tumors.
Protozoa
Non-pathogenic protozoa are present in healthy people. Pathogens can be detected in feces delivered to the laboratory no later than two hours after collection of the biomaterial. Their presence indicates an invasion.
Worm eggs
Helminth eggs in feces indicate helminthic infestation.
Larvae of roundworms of the genus Strongyloides in feces
Yeasts May be present in stool during corticosteroid or antibacterial therapy. The presence of the fungus Candida albicans indicates intestinal damage.
Sources
- Nomenclature of medical services (new edition). Approved by order of the Ministry of Health and Social Development of the Russian Federation dated October 13, 2021 No. 804n. Valid from 01/01/2018. As amended by Order of the Ministry of Health of Russia dated March 5, 2020 N 148n (including as amended, which came into force on April 18, 2020).
- Shakova H.H. Assessing the reliability of scatological research depending on the storage time of the material. Advances of modern natural science, magazine. 2003. No. 8. P. 131-131.
- Bugero N.V., Nemova I.S., Potaturkina-Nesterova I.I. Factors of persistence of protozoa in the fecal flora in intestinal dysbiosis. Bulletin of new medical technologies, magazine. T. XVIII. No. 3. pp. 28-31.
How to donate stool correctly
For diagnostic results to be reliable, several simple conditions must be met.
Rules for preparing for coprogram:
- 3-5 days before the examination, stop eating meat, tomatoes, beets, green vegetables, red fish - when testing for occult blood, they can become the culprits of a false positive result.
- The diet should include dairy products, mashed potatoes, lean meat, kazhi, boiled eggs, and porridge.
- A week before the test, you need to stop taking activated carbon, preparations based on bismuth, iron, antibacterial, anti-inflammatory drugs, antacids - they change the color of stool. You cannot take laxatives, use rectal suppositories, or do enemas.
- Sometimes the doctor prescribes a special diet, which details the daily amount of proteins, carbohydrates, and lipids - this is necessary in order to maximally load the digestive system, which will help detect even the slightest malfunction in its functioning.
- A coprogram can be performed no earlier than 5–6 days after an X-ray with barium, colonoscopy, or cleansing procedures.
- You cannot donate stool during menstruation or bleeding hemorrhoids.
Any deviation from the rules will distort the results of the coprogram.
What may affect the results
- Failure to follow nutritional recommendations, use of an enema, or performing a fluoroscopic or endoscopic examination shortly before the test.
- Violation of the rules for collecting stool, including the use of a non-sterile container for collecting biomaterial or collection directly from the toilet, as a result of which foreign microorganisms from urine, genital secretions, water from the toilet, etc. entered it.
- Failure to comply with the conditions for storing and transporting feces (biomaterial was delivered to the laboratory after the maximum established time from the moment of collection).
If the result of the coprogram seems incorrect to you, it is better to take the test again, adhering to all the recommendations for preparation and collection rules.
How to collect stool
It is better to collect stool from an adult and a child in the morning, immediately after the morning toilet, and try to deliver it to the laboratory as quickly as possible. You need to collect material from different parts of the feces, put them in sterile containers, or special disposable plastic containers, which can be purchased at the pharmacy. Evacuation should be natural; the use of laxatives, much less enemas, is prohibited.
In infants, it is not recommended to collect feces from the diaper; it is better to use a disposable diaper or medical oilcloth if the child has loose stools.
An older child needs to prepare a potty; first wash it with laundry soap or soda.
Important! When collecting material, you need to ensure that there is no urine in the stool.
How much feces do you need?
To carry out the analysis, you need to bring 15–20 g of material to the laboratory, which is approximately equal to 1 tsp. – this amount is quite enough to identify all the main indicators.
Is it possible to collect stool samples in the evening?
It is better to use a morning portion of feces for analysis, but if you are not sure that defecation will occur after waking up, you can collect the material in the evening; it should be stored in the refrigerator for no more than 10–12 hours, the container should be hermetically sealed.
Diseases for which a doctor may prescribe a general stool test (coprogram)
Anal fissure
With an anal fissure, feces may take the form of small lumps (“sheep feces” indicates a spastic condition of the intestines). Due to bleeding, scarlet blood and slightly changed red blood cells may be present in the stool.
Crohn's disease
With Crohn's disease, you may find blood in your stool. The Vishnyakov-Triboulet reaction reveals soluble protein in it. Crohn's disease affecting the colon is characterized by the presence in the feces of a large number of red blood cells in combination with leukocytes and columnar epithelium.
Colon diverticulosis
With diverticular disease, due to the long stay of stool in the colon, it takes the form of “large lumps”.
Duodenal ulcer
With a duodenal ulcer, the feces have the form of small lumps (“sheep feces” indicates a spastic condition of the intestines).
Stomach ulcer
With a stomach ulcer, the feces have the form of small lumps (“sheep feces” indicates a spastic condition of the intestines).
Chronic pancreatitis
In chronic pancreatitis with exocrine insufficiency, stool may have a pasty consistency.
Hemolytic anemia
With hemolytic jaundice (anemia), due to massive hemolysis of red blood cells, the amount of stercobilin in the feces increases.
Benign neoplasms of the colon
With a tumor accompanied by bleeding from the distal colon, the stool may have a pronounced red color. With disintegrating colon tumors, blood may be found in the stool. Pus on the surface of the stool occurs when there is severe inflammation and ulceration of the colon mucosa (disintegration of an intestinal tumor), often along with blood and mucus. When a colon tumor is in the stage of decay due to bleeding, the reaction to blood (Gregersen reaction) is positive.
Intestinal helminthiases
With helminthic infestation, the feces contain eggs of roundworms, tapeworms, etc.
Cirrhosis of the liver
In liver failure, including liver cirrhosis, the stool is grayish-white, clayey (acholic).
Ulcerative colitis
With colitis, there is mucus covering the outside of the stool in the form of thin lumps. With ulcerative colitis, blood may be found in the stool; pus on the surface of the stool, often along with blood and mucus; soluble protein in the Vishnyakov-Triboulet reaction; a large number of leukocytes (usually neutrophils); a large number of red blood cells in combination with leukocytes and columnar epithelium.
Constipation
With prolonged constipation caused by chronic colitis, peptic ulcers and other conditions associated with increased absorption of fluid in the intestine, the amount of feces decreases. With constant constipation due to excessive absorption of water, the consistency of stool is dense. With constipation, there may be mucus covering the outside of the stool in the form of thin lumps.
Malignant neoplasm of the colon
The form of feces in the form of “large lumps” - when feces remain in the colon for a long time - is noted in colon cancer. Pronounced red color of stool - with a tumor accompanied by bleeding from the distal parts of the colon and rectum. Blood in the stool can be found in disintegrating colon tumors. Pus on the surface of the stool occurs when there is severe inflammation and ulceration of the colon mucosa (disintegration of an intestinal tumor), often along with blood and mucus. A positive reaction to blood (Gregersen reaction) indicates bleeding with a tumor of the colon in the stage of decay. A large number of red blood cells in combination with leukocytes and columnar epithelium is characteristic of malignant neoplasms of the colon.
Irritable bowel syndrome, chronic colitis
With colitis with diarrhea, the amount of feces increases. The amount of feces decreases with prolonged constipation caused by chronic colitis. Mucus covering the outside of formed feces in the form of thin lumps is found in colitis. An alkaline reaction (pH 8.0-10.0) occurs in colitis with constipation. A large number of leukocytes (usually neutrophils) are observed in colitis of various etiologies.
Cholera
In cholera, stool looks like a gray inflammatory exudate with fibrin flakes and pieces of the colon mucosa (“rice water”).
Amoebiasis
With amebiasis, the stool is jelly-like, deep pink or red.
Typhoid fever
In typhoid fever, the stool looks like “pea soup.”
Decoding the results of scatological research
When the results are ready, the person will receive a form indicating normal indicators and the results obtained from the study of the material. It is better to consult a doctor for a decoding, since even a deviation from the norm of several indicators does not always indicate the presence of pathologies.
Normally, an adult's feces should be uniformly brown in color, dense, and have a characteristic odor.
The feces of a healthy person are free of foreign impurities, food debris, protozoa and parasite eggs. The presence of undigested fiber in the stool indicates low acidity of gastric juice, the presence of blood and pus indicates serious gastrointestinal pathologies.
Macroscopic examination
Quantity
In pathology, the amount of feces decreases with prolonged constipation caused by chronic colitis, peptic ulcers and other conditions associated with increased absorption of fluid in the intestines. With inflammatory processes in the intestines, colitis with diarrhea, and accelerated evacuation from the intestines, the amount of feces increases.
Consistency
Thick consistency - with constant constipation due to excessive absorption of water. Liquid or mushy consistency of stool - with increased peristalsis (due to insufficient absorption of water) or with abundant secretion of inflammatory exudate and mucus by the intestinal wall. Ointment-like consistency - in chronic pancreatitis with exocrine insufficiency. Foamy consistency - with enhanced fermentation processes in the large intestine and the formation of a large amount of carbon dioxide.
Form
The form of feces in the form of “large lumps” - when feces remain in the colon for a long time (hypomotor dysfunction of the colon in people with a sedentary lifestyle or who do not eat rough food, as well as in cases of colon cancer, diverticular disease). The form in the form of small lumps - “sheep feces” indicates a spastic state of the intestines, during fasting, stomach and duodenal ulcers, a reflex nature after appendectomy, with hemorrhoids, anal fissure. Ribbon or “pencil” shape - for diseases accompanied by stenosis or severe and prolonged spasm of the rectum, for rectal tumors. Unformed feces are a sign of maldigestion and malabsorption syndrome.
Color
If staining of stool by food or drugs is excluded, then color changes are most likely due to pathological changes. Grayish-white, clayey (acholic feces) occurs with obstruction of the biliary tract (stone, tumor, spasm or stenosis of the sphincter of Oddi) or with liver failure (acute hepatitis, cirrhosis of the liver). Black feces (tarry) - bleeding from the stomach, esophagus and small intestine. Pronounced red color - with bleeding from the distal parts of the colon and rectum (tumor, ulcers, hemorrhoids). Gray inflammatory exudate with fibrin flakes and pieces of the colon mucosa (“rice water”) - with cholera. The jelly-like character is deep pink or red in amoebiasis. In typhoid fever, the stool looks like “pea soup.” With putrefactive processes in the intestines, the feces are dark in color, with fermentative dyspepsia - light yellow.
Slime
When the distal colon (especially the rectum) is affected, the mucus occurs in the form of lumps, strands, ribbons, or a glassy mass. With enteritis, the mucus is soft, viscous, mixing with feces, giving it a jelly-like appearance. Mucus, covering the outside of formed feces in the form of thin lumps, occurs with constipation and inflammation of the large intestine (colitis).
Blood
When bleeding from the distal parts of the colon, the blood is located in the form of streaks, shreds and clots on formed stool. Scarlet blood occurs when bleeding from the lower parts of the sigmoid and rectum (hemorrhoids, fissures, ulcers, tumors). Black feces (melena) occur when there is bleeding from the upper digestive system (esophagus, stomach, duodenum). Blood in the stool can be found in infectious diseases (dysentery), ulcerative colitis, Crohn's disease, disintegrating colon tumors.
Pus
Pus on the surface of the stool occurs with severe inflammation and ulceration of the mucous membrane of the colon (ulcerative colitis, dysentery, disintegration of an intestinal tumor, intestinal tuberculosis), often together with blood and mucus. Large amounts of pus without mucus are observed when opening paraintestinal abscesses.
Leftover undigested food (lientorrhea)
The release of undigested food residues occurs with severe insufficiency of gastric and pancreatic digestion.
Patient preparation rules
feces
Standard preparation conditions (unless otherwise determined by the doctor):
3 days in advance Stop taking antimicrobial drugs, laxatives, enemas, suppositories.
Immediately before the examination Do not drink alcohol. Do not eat foods that increase fermentation in the intestines. Notes:
Collect a sufficient amount of stool (1/3 container) after involuntary bowel movement (more than 5 g or ml if the sample is liquid). Feces should not contain foreign impurities. Material for research collected after an enema, taking medications that affect peristalsis, taking castor or vaseline oil, after administering suppositories, or medications that affect the color of stool (iron, bismuth) is not accepted. You should not collect biomaterial during menstruation, in the presence of bleeding hemorrhoids, blood in the urine, or after significant effort during defecation.
You can add this study to your cart on this page
Diseases
The list of pathologies that are detected through fecal analysis is quite wide. Based on the results of the study, the following primary diagnoses can be established.
Table 1. Diseases that can be detected through fecal testing
| Disease | Symptoms |
| Cholelithiasis. | The stool takes on a beige tint, belching of bile appears, discomfort in the liver area and frequent attacks of nausea. |
| Ulcer of the stomach and duodenum. | Injury to the mucous membrane leads to the formation of rich black feces. |
| Dysentery, hemorrhoids and ulcerative colitis. | Splotches of bloody discharge. |
| Chronic pancreatitis. | Changes occurring in the intestinal microflora are fraught with the formation of a large amount of undigested food in the stool. Feces have a foul odor associated with rotting processes. |
| Dysbacteriosis. | The stool becomes liquid and smells unpleasant. |
| Inflammatory processes of the intestines and colitis. | These ailments are accompanied by the formation of mucus in the feces. |