Frostbite - causes, symptoms and first aid
Table of contents
- Causes of frostbite and their nature
- Symptoms of frostbite
- Degrees of frostbite
- First aid for frostbite
- What not to do if you have frostbite
- Treatment of frostbite
- Prevention of frostbite
With the onset of frost, the risk of frostbite increases - damage to body tissues caused by exposure to low temperatures. About 90% of frostbite cases occur on the extremities, sometimes leading to irreversible consequences: tissue necrosis and gangrene.
Causes of frostbite and their nature
Frostbite is a cold injury; its peculiarity is that it is likely to occur not only at sub-zero ambient temperatures, but also when a person spends a long time outdoors at a temperature of +4..+8°C.
Changes in tissues occur not only under the influence of low air temperature, but also under the local action of ice, snow, cold metal products or water.
The development of frostbite begins with pathological changes in the blood vessels. Then circulatory disorders occur, which entail degenerative changes in the cells of the body; secondary tissue necrosis develops. Most often the face, limbs (fingers), and ears are affected. Frostbite in other parts of the body is rare, usually with general freezing, when profound changes are observed in all tissues, blood circulation stops and anemia of the brain occurs.
The development of frostbite is promoted by:
• General exhaustion of the body, vitamin deficiency. • Elderly age. • Vascular diseases and circulatory disorders. • Strong wind. • High air humidity, damp clothes. • Alcohol intoxication. • Drowsiness. • Incorrectly selected clothes and shoes. • Limb injuries.
Symptoms of frostbite
Symptoms differ depending on the period of frostbite:
• Before warming up (pre-reactive period) – at this time, a tingling, burning sensation is felt in the affected areas of the body. The feeling of cold is gradually replaced by loss of sensitivity. The skin at the site of frostbite becomes pale, with a bluish tint. The limbs stop moving and “turn to stone.” • After warming up (reactive period) – the affected area becomes painful and swelling develops.
Subsequently, inflammation and signs of tissue death appear.
Immediately after warming the frostbitten area, it is impossible to determine the severity of the lesion; sometimes the picture becomes clear after a few days. There is a classification of frostbite based on the depth of penetration of cold damage into the tissue.
Degrees of frostbite
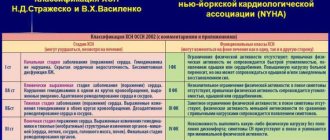
1st degree – there is a circulatory disorder without tissue death. All violations are reversible. Patients feel pain, a burning sensation in the affected area, then sensitivity to external stimuli disappears. After warming up, the skin turns red and swelling appears. These phenomena go away on their own after a few days, the skin peels off and then takes on its normal appearance.
2nd degree – tissue nutrition is disrupted, blisters with light contents appear inside, and an infection may develop. Tissue functions are restored within a week, sometimes it takes longer.
The 3rd degree of frostbite is characterized by the appearance of blisters filled with blood. The epithelium completely dies, patients experience severe pain. Gangrene develops - tissue death with the spread of infection to large areas of the body. Dead tissue is rejected within two to three weeks, healing occurs slowly, with the formation of scars and cicatrices.
With the 4th degree of frostbite, necrosis occurs not only of soft tissues, but also of bones. The limbs become covered with dark blisters, pain is not felt, the fingers become black and mummify. Starting from the ninth day after frostbite, a granulation shaft appears - a line separating living and dead tissue. Rejection of dead areas and scarring occurs slowly, over two months. This degree is characterized by the frequent addition of erysipelas, sepsis, and osteomyelitis.
First aid for frostbite
First aid to victims of frostbite occurs in the pre-reactive period, that is, before warming up. It includes the following activities:
• Warming the patient and his affected limbs. • Restoration of blood circulation in frostbitten areas of the body. • Artificial respiration or administration of drugs to restore breathing (if necessary). If necessary, call an ambulance. • Protection against infection through affected areas. • Inside – hot drinks (tea, coffee), cardiac medications. • Taking foot baths with a gradual increase in temperature from +18°C to +37°C. • Light massage of the limbs. • If signs of blood circulation appear (redness of the skin, increased body temperature), massage and warming are stopped, the affected areas are wiped with alcohol and an aseptic bandage is applied.
What not to do if you have frostbite
Do not rub frostbitten areas with snow, as it can cause infection through damaged skin; Rubbing in oils and fats is ineffective.
Also, avoid warming the extremities too quickly due to the risk of shock. This is explained by the fact that cold blood from a frostbitten limb, when suddenly warmed up, instantly enters the bloodstream; the temperature difference causes a drop in pressure and shock.
It would be a mistake to drink alcohol in the cold, since due to the dilation of blood vessels, heat is lost and the result is the opposite effect.
After providing first aid and warming the patient, you can begin to treat frostbite.
Treatment of frostbite
The choice of treatment method depends on the degree of frostbite; doctors recommend administering anti-tetanus serum for prophylactic purposes for frostbite of degrees 2–4. For frostbite of the 1st degree, the affected areas are wiped with a solution of tannin or boric alcohol.
Physiotherapy procedures are prescribed: darsonvalization, UHF therapy. It is possible to use ointments with antibiotics (levomekol, oflomelid).
For frostbite of the 2nd degree, the blisters that appear and the skin around them are treated with 70% ethyl alcohol. After opening the blisters, the epidermis is removed and an alcohol dressing is applied to the wound. For preventive purposes, the doctor may prescribe antibiotics.
Frostbite of the 3rd degree is accompanied by tissue necrosis, so surgical treatment is performed - removal of dead areas (necrectomy). Apply bandages with alcohol or hypertonic (10%) sodium chloride solution, and prescribe antibiotics.
For grade 4 frostbite, surgical methods such as necrectomy, necrotomy, and amputation are used.
General treatment for all types of frostbite includes:
• Use of sleeping pills and painkillers. • Vitamin therapy. • Enhanced nutrition. • Prescription of antibiotics locally or orally. • Taking angioprotectors, anticoagulants and vasodilators to improve blood circulation and prevent the formation of blood clots. • Administration of detoxification solutions to remove waste products from the blood. • During the recovery period – courses of magnetic therapy, UHF, electrophoresis
For mild frostbite, you can use the following recipes:
• Dilute a teaspoon of calendula tincture in 10 ml of water and apply as a compress. • Use a decoction of potato peels to make baths for frostbitten hands or feet. • Apply pieces of aloe leaf to the affected areas.
Advice: when warming up from frostbite, you need to drink a lot of hot, sweet liquid: a decoction of viburnum, chamomile, ginger; Regular tea will also work.
Injuries often occur in winter when curious children taste frozen metal objects: the tongue instantly freezes to the piece of iron. Confused, the parents literally tear the child’s tongue off the metal, although it is enough to pour warm water on the stuck area. If a shallow wound forms on the tongue, it should be washed with hydrogen peroxide and a sterile bandage applied until the bleeding stops. Usually small wounds on the tongue heal quickly; rinsing with chamomile or calendula decoctions will help speed up the process. If the child is severely injured, it is necessary to see a doctor.
Prevention of frostbite
In frosty weather, you need to carefully prepare for going outside, especially if you have to stand for a long time at a bus stop or somewhere else.
• Wearing layers of clothing is recommended. It would be good if the sweaters were wool, creating an air layer. • Shoes should be a size larger to accommodate warm insoles and thick wool socks. • You need to remove metal jewelry before going out into the cold. • It is also recommended to eat a hearty meal; food should be high in calories to provide the body with energy. • You should not lubricate your face and hands with regular moisturizing creams; there are special protective compounds for applying to the skin before going out into the cold. • In the cold you need to move all the time, turn away from the wind, and at the first opportunity go into warm rooms (cafes, shops).
By following simple frostbite prevention measures, you can protect yourself and your family from the unpleasant consequences of exposure to low temperatures. Knowing simple first aid techniques for frostbite will help reduce the likelihood of complications in the event of an emergency.
Source: nmedik.org
Frostbite: main risks
Most often, the feet suffer from cold, followed by the hands, followed by the nose, ears and cheeks. The body loses heat faster in cold water, or if a person is wearing wet clothes or shoes. The risk of frostbite is higher in strong winds and snowstorms, as well as in those who wear tight shoes or do not change body position for a long time. Vascular diseases, neuritis, previous frostbite, fatigue, exhaustion, hunger, and past infectious diseases also contribute to cold injury. People often get frostbite while intoxicated.
First aid
The victim must be moved from the cold to a warm, windless place, take off wet clothes, and wrap him in a blanket. You can warm a frostbitten area using heat-insulating materials, for example, cotton-gauze bandages with a layer of compress paper or plastic film; if this is not at hand, use foam rubber, blankets, and so on.
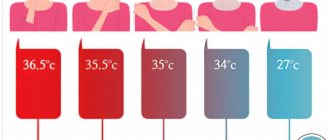
A hot drink and a warm bath will help you warm up. It is necessary to heat the water in it gradually. They start with a temperature of plus 17–18 degrees and within about an hour the water is heated to plus 36–37 degrees.
But you shouldn’t rub frostbitten skin with ice and snow. There is a high risk of further hypothermia and injury.
First aid for hypothermia
The victim needs to be helped to restore normal body temperature. The simplest and safest method is warm clothes, blankets and a warm room. It is very important to keep your head covered because it gives off 30 percent of the heat. Electrically heated blankets can be used. Only the chest needs to be warmed, otherwise complications may occur.
Hot drinks and a warm bath (heat gradually to a temperature no higher than plus 36 degrees) help. In the bath, you can gently rub your body with soft washcloths. With a mild degree of cooling, only warming is sufficient; with moderate and severe cooling, the victim needs medical attention.
What not to do if you have frostbite
Some things in the treatment of frostbite seem self-evident - for example, the need to warm the affected area. However, some common “first aid” methods can only aggravate the damage, and they should not be used under any circumstances: • in case of deep tissue damage, frostbitten areas of the skin should not be warmed by an open fire, or with heating pads and other heating devices; • do not rub frostbitten areas with alcohol or fat; • in the same way, you should not drink alcohol - it causes a short-term expansion of the capillaries and can warm you up for a while, but increased heat loss occurs through the dilated vessels - therefore, frostbite can worsen; • It is strictly forbidden to rub frostbitten areas of skin with snow!
Signs of hypothermia
Hypothermia is accompanied by a general depression of consciousness, up to coma; Muscle tremors may occur. A decrease in temperature below 30 degrees leads to the cessation of trembling and the appearance of muscle rigidity, reminiscent of rigor. There are three successive stages of development of general cold injury: mild, moderate and severe.
During the mild stage, the internal body temperature drops below 35 degrees. First, a person feels chills, breathing and pulse quicken, blood pressure rises slightly, and goose bumps appear. Then, due to a decrease in the temperature of the internal organs, their functions are inhibited: the frequency of breathing and heartbeat decreases, the person feels lethargy, apathy, drowsiness, and muscle weakness. Coordination of movement and vision may be impaired, and hallucinations may occur.
During the middle stage of frostbite, the temperature of the internal organs drops to about 30 degrees. The victim's skin turns pale (sometimes acquires a marble tint), the heart rate decreases, consciousness becomes confused, speech and movements are impaired, facial expressions are absent, reflexes are weakened, and stupor occurs.
In the severe stage, the temperature of the internal organs drops below 30 degrees, and all the basic vital functions of the body are inhibited. A person may experience cramps and increased muscle tone. It becomes difficult to straighten the arms and legs, the victim is unconscious, and reflexes weaken. A person’s heart rate and blood pressure decrease, breathing becomes less frequent; Possible urinary and fecal incontinence. With a further drop in temperature, imaginary death may occur, in which breathing, pulse and blood pressure are barely perceptible, and reflexes are not detected. If the core body temperature drops to 25–22 degrees, a person may die.
After the body warms up, a reactive period begins. As a rule, lethargy, fatigue, drowsiness, stiffness of movement, and headache are noted. In severe hypothermia, swelling of internal organs may develop: the brain, lungs and others. Thrombosis may occur, and cardiovascular activity may also be disrupted, acute renal failure and nervous system disorders may develop. Subsequently, inflammation of internal organs may appear: pneumonia, bronchitis, nephritis and others.
What are the signs of frostbite?
The first signs of frostbite are easy to miss. The skin temperature drops, it becomes pale, loses sensitivity, but a tingling or burning sensation may be felt. While a person is in the cold, it is very difficult to determine the extent of damage. It is determined after warming.
If the skin becomes warmer when warmed, and sensitivity is restored, this means that the cold injury is superficial. Pain and lack of sensitivity are characteristic of deep frostbite.
Based on the depth of injury, injuries are divided into four types. The first two are classified as superficial, the rest - deep. First degree frostbite affects the superficial layers of the skin. After warming up, pale skin may turn red or even become bluish, and after a while it may peel off. Within a week her condition returns to normal.
With a second-degree injury, blisters filled with fluid, most often light, form on the skin. After about a week they subside, and after another two to three weeks the skin is completely restored.
In the third degree, the blisters are often filled with pink or red liquid, and their bottom is blue-purple. After the dead tissue is sloughed off, wounds are formed. With the fourth degree of frostbite, the affected part of the body swells sharply, becomes dark, and gangrene may develop.