For the body to function normally, blood circulation must occur continuously. The blood supply to organs and systems is ensured by the pumping function of the heart muscle, which pushes out 70 - 80 ml of blood (cardiac output) with each systole. In a minute, in an adult with a heart rate of 70 beats, the heart pumps about 5 liters of blood (and in a day - more than 7 tons!).
- Anatomical and functional features of the cardiovascular system
- Acute cardiovascular failure
- Urgent measures
- Drug therapy
- Shock
- Collapse
The main reasons for the progression of the disease under study
If collapse occurs, emergency care is indicated in the following situations:
- acute bleeding, resulting in the loss of a large amount of blood,
- serious burns,
- viral diseases,
- intoxication with certain medications,
- stressful situations; depressive mood
- acute cardiovascular failure,
- diseases in the nervous system,
- endocrine pathology.
Urgent measures
- Provide the patient with a semi-sitting position with legs down (orthopnea)
- Provide inhalation of humidified oxygen through a nasal catheter. This catheter is lubricated with glycerin and inserted through the nasal passage to a depth of 10-12 cm (the distance from the wing of the nose to the auricle), fixing it to the skin with a bandage. It is forbidden to use Vaseline, which can catch fire in the presence of oxygen!
- It should be noted that when oxygen supply is 6-7 l/min. its concentration in the nasopharynx cavity will be 35-40%. When a catheter is inserted superficially (a common mistake), the oxygen content in the respiratory mixture decreases, and drying out of the nasal mucosa causes discomfort in patients.
- Apply venous tourniquets to the patient's arms and legs (to reduce blood flow to the heart). During such events, up to 1-1.5 liters of blood are deposited in his limbs.
- Assess the state of cardiac activity and diuresis. The nurse, without waiting for the doctor's instructions, must attach a cardiac monitor to the patient, measure blood pressure and pulse rate, and perform bladder catheterization.
- Catheterize the vein. All medications and, especially, infusion therapy should be carried out under the control of central venous pressure.
- Apply defoamers. To do this, use a solution of antifomsilan or ethyl alcohol (40-96 °), through which oxygen is passed.
Drug therapy
Cardiac glycosides are prescribed, which improve myocardial contractility:
- strophanthin solution (0.05%);
- solution of corglycone (0.06%);
- digoxin solution (0.025%).
To improve coronary blood flow, the patient is given nitroglycerin: a tablet (0.0005 g) under the tongue with an interval of 10-20 minutes. Morphine solution (1% - 1 ml) reduces the excitability of the respiratory center, shortness of breath, has a calming effect, and reduces pressure in the pulmonary circulation. Sometimes it is advisable to administer thalamonal (1-2 ml of 0.005% fentanyl solution and 1-2 ml of 0.25% droperidol solution), which, in addition, has a vasodilating effect.
In the presence of high blood pressure (systemic blood pressure > 150 mm Hg), ganglion blockers :
- pentamine (1 ml of 5% solution, dissolved in 100-150 ml of isotonic sodium chloride solution, administered dropwise);
- arfonade (250 mg, dissolved and administered similarly) under blood pressure control, not allowing it to decrease by more than a third.
These drugs reduce blood flow to the right side of the heart.
Osmotic diuretics (mannitol, urea) are contraindicated because they cause an increase in circulating blood volume, worsening heart function.
In a terminal condition, a patient with acute heart failure should be intubated and mechanically ventilated with a high oxygen content in the respiratory mixture and positive expiratory pressure (about 5 cm Hg).
Acute right ventricular failure is the inability of the right ventricle to pump blood from the systemic circulation to the pulmonary circulation due to its weakness or the presence of an obstruction to blood flow. It occurs with pulmonary embolism, myocardial infarction of the right ventricle, excessive infusion-transfusion therapy (especially with citrated blood transfusions) in patients with heart failure, with lung diseases (bronchial asthma, emphysema, pneumosclerosis), resulting in an increased load on the right ventricle
Patients experience severe acrocyanosis, tachycardia, suffocation, bloating and pulsation of the saphenous veins, especially in the neck. Swelling occurs in the lower extremities. The liver enlarges and ascites appears. Central venous pressure increases sharply (reaches 200-250 mm Hg), which, however, is not accompanied by pulmonary edema.
Intensive therapy is pathogenetic. If infusion therapy is necessary, the volume and rate of transfusions should be limited. When transfusions of blood preserved with a citrate solution, to prevent hypocalcemia, 10 ml of a 10% calcium gluconate solution should be administered for every 500 ml of preserved blood.
If bronchospasm is present, administer bronchodilators. Excess fluid is removed from the body using diuretics (furosemide solution). Metabolic acidosis is corrected with 4% sodium bicarbonate solution (drip under the control of CBS). For pulmonary embolism, anticoagulants are used (fraxiparin solution 0.6 mg subcutaneously; heparin solution 5000 IU every 4 hours), fibrinolytics (fibrinolysin, urokinase, streptodecase, cabikinase, etc. according to the instructions ).
How does collapse occur?
The progression of the disease is quite acute. The condition is dangerous, and in the absence of timely emergency assistance in case of collapse, we can talk about serious and terrible consequences.
The main symptoms of the disease are:
- general weakness of the body and fatigue,
- dizziness,
- decrease in blood pressure,
- the skin becomes significantly lighter,
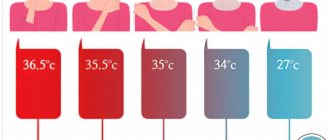
- decrease in temperature indicators,
- chills,
- facial features become sharper,
- dry mouth,
- loss of consciousness.
Help with collapse is urgently needed!
Symptoms
The disease occurs completely unexpectedly. Initially, weakness and dizziness occur, and the patient is thirsty. The skin becomes lighter than its normal state, profuse cold sweating appears on it, characterized by chills. The pulse becomes slower, the pressure decreases significantly, and shortness of breath is also observed. Among other things, you may notice deterioration in vision, the appearance of extraneous sounds in the ears, and the person may be worried about something. As the disease progresses, a person's thoughts become confused, his pupils dilate, and his heart beats much faster.
symptoms of collapse
Prevention and treatment
If you are wondering what is the sequence of first aid for collapse , then we offer you the following recommendations:
- The pathology in question implies a phenomenon that requires immediate intervention by specialists. People who happen to be nearby when the disease progresses should change the position of the patient during collapse and put him on the bed, raise his legs and cover him with a warm blanket to prevent him from freezing.
- In a short period of time, you need to find the cause of the decrease in pressure and get rid of it: stop heavy bleeding, give the person the necessary medications, and so on.
- At this time, it is also necessary to provide for parenteral infusion of blood components or mixtures that serve as a replacement for blood.
- In some particularly dangerous situations, it is necessary to carry out resuscitation measures to help save the patient’s life.
Prevention of this disease is reflected in properly selected treatment of those pathologies that can cause the development of collapse, in systematically undergoing a medical examination and taking into account the side effects of medications taken. Now you know the difference between collapse and fainting , and how to provide first aid.
Anatomical and functional features of the cardiovascular system
From the left ventricle, blood enters the arterial system of the systemic circulation. Arteries contain 15% of the total circulating blood volume. These vessels carry blood to the tissues. The terminal sections of the arteries end in arterioles (resistance vessels). They perform the function of distributing blood in tissues. Thus, an increase in the tone of the arterioles (their spasm) prevents the flow of blood into the capillary pool. Tissue ischemia occurs, and blood flows into the venous system through arteriovenous anastomoses. A decrease in arteriolar tone, on the contrary, increases their lumen and enhances blood supply to tissues.
Natural vasoconstrictors (vasoconstrictors) are:
- adrenalin,
- norepinephrine,
- serotonin,
- angiotensin-2.
Under stress, the concentration of catecholamines (adrenaline, norepinephrine) in the blood increases sharply. They cause spasm of arterioles; a phenomenon of centralization of blood circulation occurs with a decrease in peripheral blood flow. The vasodilating effect is exerted by “acidic” metabolites (lactates, pyruvate, adenylic and inosinic acids), bradykinin, histamine, acetylcholine, a number of medications (neuroleptics, alpha-adrenolytics, peripheral vasodilators, ganglion blockers, etc.), some exogenous poisons, etc. Their action causes the phenomenon of decentralization of blood circulation (opening of the lumen of arterioles and redistribution of blood from the central vessels to the periphery, into the capillary bed).
Capillaries are an extensive network of the smallest vessels in the body, with a total length of 90,100,000 kilometers. About 20-25% of the capillaries function simultaneously, in which the transition of oxygen and nutrients from the blood to the tissues and the removal of “waste” metabolic products from them occurs. Periodically, with an interval of several tens of seconds, other capillaries open, where the blood is redistributed (vasomotion effect). Capillaries contain 12% of all circulating blood. However, in some pathological conditions this volume can increase several times.
The waste blood flows from the capillaries into the venous system. Veins play the role of a blood reservoir, since they contain the bulk of it (70%). They, unlike arteries, are able to change their volume, affecting the flow of blood to the heart.
The most important hemodynamic indicator of the venous system is central venous pressure (CVP). This is the pressure that blood exerts on the walls of the vena cava and the right atrium. It is an integral indicator of circulating blood volume, vascular tone and pumping function of the heart. CVP is measured with a phlebotonometer. Normally it is 60-120 mm of water column.
Central venous pressure decreases when:
- blood loss;
- excessive loss of water (hypohydration);
- decreased tone of arterioles and veins.
This reduces the volume of blood flowing to the heart and, accordingly, reduces cardiac output. With negative CVP values, there is a danger of circulatory arrest. Venous pressure increases when:
• heart failure (left and right ventricular);
• excessive infusion of blood and other fluids;
• obstruction of blood flow from the right ventricle of the heart (pulmonary embolism).
When the CVP is more than 150-160 mm Hg. against the background of left ventricular failure, patients may develop pulmonary edema. An integral indicator of the hemodynamics of the arterial part of the vascular system is blood pressure (systolic, diastolic, pulse and average). Systolic and diastolic blood pressure are measured with a tonometer using the Korotkoff method. Pulse blood pressure is the difference between systolic and diastolic.
The value of blood pressure is influenced by the volume of cardiac output and the resistance of peripheral vessels (arterioles). This dependence is directly proportional. Therefore, you can increase a patient’s blood pressure in the following ways:
- introduce vasoconstrictor agents (adrenaline solution, mezaton, etc.);
- increase the volume of circulating blood (by transfusion of polyglucin, refortan, etc.);
- improve the functional ability of the myocardium (by introducing cardiac glycosides, etc.).
The total blood volume in humans is about 7% of body weight: in men 70 ml/kg, in women - 65 ml/kg. The circulating blood volume (CBV) is somewhat smaller, since part of the blood does not participate in the circulation, being in the vascular depot. BCC can be measured by injecting a known concentration of a substance into the bloodstream, for example, Evans blue or polyglucin, and determining the degree of its dilution. So, measurements of central venous pressure, blood pressure, cardiac output and blood volume in patients make it possible to identify the characteristics of circulatory disorders and carry out adequate corrective therapy.