November 15, 2021
43 132
20 minutes
Author, editor and medical expert – Klimovich Elina Valerievna.
Acute infections of the upper respiratory tract include inflammation of the nasal cavity, nasopharynx, pharynx and larynx (above the vocal cords) caused by various microorganisms. They all have similar symptoms (despite the variety of pathogens), so in everyday life they are often called “colds,” and doctors use the general term “acute respiratory diseases,” or acute respiratory infections, to refer to them.
Acute respiratory infections are observed all year round. On average, adults get colds 2 to 4 times a year, children get sick more often, 6-9 times - this is normal and necessary for the formation of a healthy immune system2. The peak incidence of acute respiratory tract infections occurs in the autumn-winter-spring period1. The likelihood of colds increases with the first cold snap, in September-October1, when we begin to go out less often and have longer contact with other people, among whom there may be carriers of pathogenic microbes or patients with acute respiratory infections. High humidity and cold outside often cause hypothermia and decreased immunity. Low air humidity in heated rooms leads to drying out of the nasal mucosa, increasing its permeability and susceptibility to infectious agents. Only in May, when the weather improves, does the incidence decline1.
Up to contents
EXacERBATION OF CHRONIC BRONCHITIS
Chronical bronchitis
- a disease associated with prolonged exposure to nonspecific irritants (tobacco smoke, etc.) on the respiratory tract, accompanied by hypersecretion of mucus and inflammatory and degenerative changes in the bronchi and lung tissue. The key symptom of the disease is a chronic productive cough observed for at least 3 months over 2 consecutive years, with the exclusion of other diseases/pathological conditions (tuberculosis, congestive heart failure, etc.).
Exacerbation of chronic bronchitis
is accompanied by increased cough, shortness of breath, an increase in the volume of sputum produced, its purulent nature and/or an increase in body temperature. Bacterial and viral infections are responsible for exacerbations of chronic bronchitis in 1/2-2/3 of cases. Other causes of exacerbation of the disease may be allergens, air pollutants, etc.
Main pathogens
Among the bacterial pathogens of exacerbations of chronic bronchitis
H.influenzae, S.pneumoniae
and
occupy a key position .
In special clinical situations (age over 65 years, concomitant diseases, severe bronchial obstruction - FEV1 less than 50% of the required values, constant separation of purulent sputum),
P.aeruginosa, S.aureus
, and enterobacteria acquire a certain etiological significance. About 30% of infectious exacerbations of the disease are caused by influenza/parainfluenza viruses, RSV, rhinoviruses, and coronaviruses.
Choice of antimicrobials
When choosing AMPs, it is necessary to take into account the patient’s age, the severity of bronchial obstruction syndrome, the frequency of exacerbations, the presence of concomitant diseases, the use of glucocorticoids and AMPs (Table 1).
Table 1. Selection of antimicrobial drugs for exacerbation of chronic bronchitis
| Amoxicillin Doxycycline | Amoxicillin/clavulanate Azithromycin Clarithromycin Levofloxacin Moxifloxacin | ||
| Increased shortness of breath, increased volume and purulence of sputum. Age 65 years and older and/or severe bronchial obstruction (FEV1 < 50%), frequent exacerbations (from 4 times a year), concomitant diseases, exhaustion, long-term glucocorticoid therapy, disease duration more than 10 years | H.influenzae (the proportion of β-lactamase-positive strains increases) S.pneumoniae M.catarrhalis Sometimes Enterobacteriaceae | Amoxicillin/clavulanate Levofloxacin Moxifloxacin | |
| Constant separation of purulent sputum, frequent exacerbations | H.influenzae S.pneumoniae M.catarrhalis Enterobacteriaceae P.aeruginosa | Ciprofloxacin | Antipseudomonal β-lactams Aztreonam |
Due to the fact that exacerbation of chronic bronchitis in most cases is not severe, preference should be given to AMPs for oral administration. In cases of severe exacerbation in debilitated patients or those in hospital, parenteral administration of antimicrobial agents may be required. The duration of antibiotic therapy is 7-14 days.
Symptoms of acute respiratory infections
The clinical picture of all colds consists of the same general and local manifestations in varying degrees of severity and combinations.
General symptoms
Their severity depends on the type of pathogen and can vary from mild malaise to severe intoxication, accompanied by disruption of the functioning of internal organs and clouding of consciousness.
| Fever | It can be especially pronounced in young children, in whom the symptoms of intoxication prevail over the local manifestations of a cold5. Fever may be absent in mild cases of the disease, as well as in weakened patients and elderly people1. |
| Aches and pains in muscles and joints | In some patients, these sensations are limited to the appearance of a feeling of weakness; in others, the body aches are so strong that they do not allow them to sleep and force them to take painkillers. |
| Headache | It is more typical for influenza, but can also appear with other viral diseases, especially when they are severe1 and the temperature rises to 40 0C or higher. In these cases, the headache may be accompanied by nausea and unrelieved vomiting associated with irritation of the meninges1. |
| Gastrointestinal discomfort | Decreased appetite, nausea and vomiting, intestinal colic and diarrhea, as manifestations of a viral infection of the upper respiratory tract, are more common in children5. Sometimes they accompany streptococcal lesions5. |
Local manifestations of acute respiratory infections
Their diversity is determined by the level of damage to the respiratory tract.
| Runny nose | It begins with the appearance of itching, burning, nasal congestion, sneezing and copious mucous discharge from the nasal passages. As the process develops and bacterial microflora joins, the nasal mucus acquires a yellowish-greenish tint, there is less of it, and it begins to dry out, forming crusts in the nose. This reduces nasal congestion. |
| Sore and sore throat | They are associated with inflammation and dryness of the pharyngeal mucosa, intensify during swallowing and decrease slightly after warm drinking. The mucous membrane of the pharynx, palatine arches, uvula and tonsils look red and swollen. Enlarged lymphoid follicles are visible on the posterior wall of the pharynx. |
| Cough | One of the causes of cough during acute respiratory infection is the flow of mucus from the nose and nasopharynx into the respiratory tract. The second reason is associated with irritation of the receptors of the inflamed pharynx - in this case, the cough appears approximately on the 2-3rd day of the disease, more often it is dry, hacking, and even vomiting. A barking cough and hoarseness on the 4-5th day of illness indicate involvement of the larynx in the pathological process and the development of laryngitis. Children may develop false croup, in which attacks of convulsive coughing are accompanied by difficult, noisy breaths, and sometimes even periods of cessation of breathing5. The condition worsens at night, which is associated with an increase in mucus production and impaired sputum discharge at this time of day5. |
| Sputum | In the first days of the disease, the cough is always dry and painful. The appearance of sputum in the following days alleviates the suffering somewhat. When the upper parts of the respiratory tract are affected, it is not abundant. Its mucous nature indicates the viral nature of the disease; bacterial infections of the respiratory tract are accompanied by the release of purulent sputum. |
Additional symptoms
Along with the general manifestations typical of all diseases of the upper respiratory tract, in some cases specific symptoms are observed.
Thus, when infected with adenoviruses, signs of conjunctivitis appear; children often have abdominal pain associated with inflammation of the intra-abdominal lymph nodes5.
Respiratory syncytial virus tends to affect not only the upper, but also the lower parts of the respiratory tract, quickly causing the development of bronchitis and bronchiolitis1.
Bad breath is often a symptom of a bacterial respiratory tract infection. It is associated with the appearance of pus in the oropharynx - a product of inflammation and the activity of pathogenic microorganisms.
Up to contents
PNEUMONIA
Pneumonia
- an acute infectious disease characterized by focal damage to the respiratory parts of the lungs with intra-alveolar exudation, detected by objective and x-ray examination, expressed in varying degrees by a febrile reaction and intoxication.
Clinically significant is the division of pneumonia into community-acquired
and
nosocomial (hospital, in-hospital)
. This division of pneumonia has nothing to do with the severity of their course. The main and only criterion for differentiation is the environment in which pneumonia developed.
Nosocomial pneumonia
- pneumonia that develops in a patient no earlier than 48 hours after hospitalization and was not in the incubation period.
Main pathogens
Community-acquired pneumonia
Pneumococcus remains the most common causative agent of community-acquired pneumonia (Table 2). Two other microorganisms are M.pneumoniae
and
C.pneumoniae
- often occur in young and middle-aged people (up to 20-30%), and their etiological role in patients of older age groups is less significant (1-3%).
L.pneumophila
is a rare causative agent of community-acquired pneumonia, but legionella pneumonia ranks second (after pneumococcal) in terms of mortality.
H.influenzae more often causes pneumonia in smokers, as well as against the background of chronic bronchitis. E.coli
and
K.pneumoniae
(less commonly other representatives of the
Enterobacteriaceae
) are found, as a rule, in patients with risk factors (diabetes mellitus, congestive heart failure, etc.).
The likelihood of staph pneumonia ( S. aureus
) increases in older people or in people who have had the flu.
Table 2. Etiology of community-acquired pneumonia
| Pathogen | Detection rate, % |
| S. pneumoniae | 30,5 |
| M. pneumoniae | 12,5 |
| C. pneumoniae | 12,5 |
| L.pneumophila | 4,8 |
| H.influenzae | 4,5 |
| Family Enterobacteriaceae | 3,0 |
| S. aureus | 0,5 |
| Other pathogens | 2,0 |
| Pathogen not detected | 39,5 |
Nosocomial pneumonia
The etiology of nosocomial pneumonia is dominated by gram-negative microflora of the Enterobacteriaceae family, P.aeruginosa
(Table 3).
Table 3. Etiology of nosocomial pneumonia
| Pathogen | Detection rate, % |
| P. aeruginosa | 25-35 |
| Family Enterobacteriaceae | 25-35 |
| S. aureus | 15-35 |
| Anaerobes (usually in combination with gram-negative bacteria) | 10-30 |
| H.influenzae | 10-20 |
| S. pneumoniae | 10-20 |
There is a special type of nosocomial pneumonia - ventilator-associated pneumonia, the etiology of which depends on the length of the patient's stay on mechanical ventilation. With the so-called early VAP (development in the first 4 days of being on a ventilator), the most likely pathogens are S.pneumoniae, H.influenzae, S.aureus
(MSSA) and other representatives of the normal microflora of the oral cavity.
The development of late VAP (more than 4 days on mechanical ventilation) is associated with P.aeruginosa, Acinetobacter
spp., members of the
Enterobacteriaceae
, and less commonly MRSA.
Choice of antimicrobials
When treating patients with community-acquired pneumonia, a differentiated approach should be taken to the choice of antimicrobial agents, taking into account age, severity of the condition, the presence of concomitant diseases, location of the patient (at home, in the general ward of a hospital, in the ICU), previous antimicrobial therapy, use of glucocorticoids, etc. (Table . 4).
Table 4. Choice of antibiotics for community-acquired pneumonia
| Features of the nosological form | Main pathogens | Drugs of choice | Alternative drugs |
| Non-severe course, age up to 50 years without concomitant diseases. Treatment at home | S.pneumoniae M.pneumoniae H.influenzae C.pneumoniae | Amoxicillin Modern macrolides | Doxycycline Levofloxacin Moxifloxacin |
| Non-severe course in patients with risk factors for ARP or gram-negative microflora (age 65 years and older, cardiovascular or bronchopulmonary diseases, AMP therapy within the previous 3 months, etc.). Treatment at home | Cefuroxime axetil, amoxicillin/clavulanate + macrolide, doxycycline or monotherapy with a third-fourth generation fluoroquinolone (levofloxacin, moxifloxacin) | Ceftriaxone IM | |
| Non-severe course, age under 60 years and/or with concomitant diseases. Treatment in the general department | S.pneumoniae M.pneumoniae H.influenzae Enterobacteriaceae Legionella spp. C. pneumoniae | Benzylpenicillin, ampicillin + macrolide | II-III generation cephalosporins + macrolide Amoxicillin/clavulanate, ampicillin/sulbactam + macrolide Levofloxacin Moxifloxacin |
| Severe course regardless of age. Treatment in the ICU | S. pneumoniae Legionella spp. Enterobacteriaceae S.aureus C.pneumoniae | Amoxicillin/clavulanate, ampicillin/sulbactam + macrolide III-IV generation cephalosporins + macrolide Levofloxacin + cefotaxime or ceftriaxone | Fluoroquinolones (iv) Carbapenems |
Prognostically, the rapid initiation of antimicrobial therapy, no later than 4 hours after diagnosis, is very important.
When choosing AMPs in a patient with nosocomial pneumonia
the nature of the department in which he is located (general profile or ICU), the use of mechanical ventilation and the time of development of VAP are taken into account (Table 5). Empirical therapy is planned based on local data on the sensitivity of likely pathogens. Sputum examination is mandatory, and it is desirable to obtain material by invasive methods with quantitative assessment of the results, and blood culture.
Table 5. Choice of antibiotics for nosocomial pneumonia
| Features of the nosological form | Most common pathogens | Drugs of choice | Alternative drugs |
| Pneumonia that occurred in general wards, without risk factors or early VAP | S.pneumoniae Enterobacteriaceae H.influenzae Less common: Pseudomonas spp., S.aureus | Amoxicillin/clavulanate Ampicillin/sulbactam Cephalosporins II-III generation (except ceftazidime) | Fluoroquinolones Cefepime Cefoperazone/sulbactam |
| Late ventilation pneumonia or pneumonia that occurred in general departments, in the presence of risk factors | Enterobacteriaceae Pseudomonas spp. S. aureus (including MRSA) | Cefepime Ceftazidime, cefoperazone + aminoglycoside Imipenem + aminoglycoside | Fluoroquinolones Cefoperazone/sulbactam, ticarcillin/clavulanate or piperacillin/tazobactam + aminoglycoside Vancomycin |
Risk factors: recent abdominal surgery, aspiration - anaerobes; coma, head injury, diabetes, chronic renal failure, influenza, “IV drug addicts” - S.aureus
;
large doses of glucocorticoids, cytostatics, neutropenia - Legionella
spp.,
P.aeruginosa, Aspergillus
spp.;
long stay in the ICU, treatment with corticosteroids, antibiotics, bronchiectasis, cystic fibrosis - P.aeruginosa
,
Enterobacter
spp.,
Acinetobacter
spp.
Routes of administration of antimicrobial drugs
In the treatment of outpatient forms of community-acquired pneumonia, preference should be given to oral antibiotics. However, in severe infections, AMPs must be administered intravenously. In the latter case, stepwise therapy is also highly effective, which involves switching from parenteral to oral administration. The transition should be made when the course of the disease stabilizes or the clinical picture improves (on average 2-3 days from the start of treatment).
Duration of therapy
For uncomplicated community-acquired pneumonia, antibiotic therapy can be completed once stable normalization of body temperature is achieved. The duration of treatment is usually 7-10 days.
If there are clinical and/or epidemiological data on mycoplasma, chlamydial or legionella pneumonia, the duration of antibacterial therapy should be longer due to the risk of relapse of infection - 2-3 weeks.
Duration of AMP use for complicated community-acquired pneumonia
and
nosocomial pneumonia
are determined individually.
In any case, the persistence of individual clinical, laboratory and/or radiological signs is not an absolute indication for continuation of antibacterial therapy or its modification. In most cases, these signs resolve spontaneously over time.
Prevention of respiratory diseases
Prevention of ARVI is aimed at increasing immunity. There are many known folk ways to increase the body's defenses: hardening, a diet rich in vitamins, and the use of natural phytoncides, for example, garlic.
In order not to become infected, it is necessary to take precautions: maintain a safe distance, reduce contact during periods of epidemics, wash your hands more often, ventilate the premises, dress according to the weather, avoiding hypothermia.
Vaccination provides the most effective protection against viruses. It is necessary to get vaccinated against influenza every year. You can get a pneumococcal vaccine to prevent severe pneumonia.
ABSCESS OF THE LUNG
Lung abscess
- a pathological process characterized by the formation of a limited cavity in the lung tissue as a result of its necrosis and purulent melting.
Main pathogens
Development of a lung abscess
binds primarily to anaerobic flora -
Bacteroides
spp.,
F. nucleatum, Peptostreptococcus
spp.,
P. niger
- often in combination with enterobacteria (due to aspiration of oropharyngeal contents).
Choice of antimicrobials
Drugs of choice
: amoxicillin/clavulanate, ampicillin/sulbactam or cefoperazone/sulbactam IV; benzylpenicillin intravenously, then amoxicillin orally (step therapy); benzylpenicillin + metronidazole IV, then amoxicillin + metronidazole orally (stepped therapy).
Alternative drugs
: lincosamides + aminoglycosides of II-III generation; fluoroquinolones + metronidazole; carbapenems.
Duration of therapy
determined individually.
PLEURAL EMPYEMA
Empyema of the pleura
(purulent pleurisy, pyothorax) is a pathological process characterized by the accumulation of pus in the pleural cavity and is an unfavorable variant of the course of exudative pleural effusion (pleurisy) of various origins.
Main pathogens
The composition of pathogens that are isolated during pleural empyema (Table 6) largely depends on the characteristics of pathogenesis. Thus, the main microorganisms in empyema associated with pneumonia (with or without lung abscess) are anaerobes. In contrast, the spectrum of pathogens after surgery is predominantly aerobic gram-negative bacteria or S. aureus
. In 5-20% of cases, the exudate turns out to be sterile.
Table 6. Etiology of pleural empyema
| Pathogen | Detection rate, % |
| Anaerobes | 19 |
| Gram-negative aerobes | 15 |
| S. aureus | 15 |
| S. pneumoniae | 7 |
| S.pyogenes | 1 |
| Mixed infection | 25 |
| Pathogen not detected | 28 |
Choice of antimicrobials
In most cases, it is possible to carry out targeted antibacterial therapy taking into account data from microbiological examination of the contents of the pleural cavity.
If the purulent effusion turns out to be sterile, AMPs or their combinations that are active against anaerobes and aerobic gram-negative enterobacteria should be used: inhibitor-protected penicillins; III-IV generation cephalosporins or fluoroquinolones + metronidazole; lincosamides + aminoglycosides of the II-III generation, cefoperazone/sulbactam.
The development of pleural empyema as a complication after surgery is often associated with S.aureus
. Depending on sensitivity, ghbvtytys may be oxacillin, vancomycin, cefazolin, linezolid.
The main route of administration of AMPs for pleural empyema is intravenous. The duration of antibiotic therapy is determined individually.
Diagnosis of respiratory viral infections
If after a few days you cannot cope with the cold on your own, you should consult a doctor. Modern diagnostic methods make it possible to identify the type of virus at an early stage and prevent complications.
At the Anapa Diagnostic Center you can undergo examinations, undergo fluorography, and take sputum, blood and urine tests. If a bacterial infection is suspected, a bacteriological culture will be performed. Having identified the causative agent of the disease, effective treatment will be prescribed. Call and make an appointment; the earlier treatment is started, the lower the risk of complications.
FEATURES OF TREATMENT OF NPD INFECTIONS IN CHILDREN
In children, such a nosological form as exacerbation of chronic bronchitis practically does not occur. Acute bronchitis, which in adults usually has a viral etiology and does not require the use of antimicrobial agents, in childhood can be associated with a layer of bacterial flora (pneumococcus, mycoplasma, chlamydia). Therefore, in rare cases, acute bronchitis in children may require antibiotic therapy. The drugs of choice are amoxicillin or modern macrolides.
In newborns
Intrauterine
and
nosocomial
(including those associated with mechanical ventilation) infection predominates Community-acquired pneumonia is observed in full-term infants mainly after 3-6 weeks of life, in premature infants - after 1.5-3 months.
Intrauterine pneumonia
more often caused by group B streptococci and gram-negative bacteria (
E.coli, K.Pneumoniae
), less often -
S.aureus, L.monocytogenes, T.pallidum
.
Possible associations with CMV, HSV and fungi of the genus Candida
.
In rare cases, pneumonia can be caused by P. carinii
.
For intrauterine pneumonia
The drugs of choice are ampicillin or ampicillin/sulbactam in combination with aminoglycosides. For listeriosis, the drug of choice is ampicillin in combination with gentamicin. It should be emphasized that Listeria is resistant to cephalosporins, so the latter should be combined with ampicillin.
Treatment of pneumonia in newborns is almost always carried out in a hospital. AMPs are administered parenterally.
In the treatment of nosocomial pneumonia
, especially late ventilation, a combination of inhibitor-protected penicillins or third-generation cephalosporins with aminoglycosides or monotherapy with imipenem is preferable.
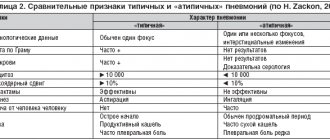
Pneumonia in children aged 1 to 6 months
can be divided into two groups:
typical
- focal (focal, confluent), developing against the background of high fever, and
atypical
- with predominantly diffuse changes in the lungs, at low or normal body temperature.
The most common causative agents of typical pneumonia
are viruses (RSV, parainfluenza, etc.),
E. coli
and other enterobacteria, staphylococci.
Pneumococci and H.influenzae
are rarely isolated at this age (about 10%).
For typical pneumonia
Amoxicillin/clavulanate, ampicillin/sulbactam, parenteral ampicillin are used. Alternative AMPs are II-III generation cephalosporins.
With chlamydia ( C. trachomatis
) for pneumonia, modern macrolides are the drugs of choice.
For anaerobic infections, inhibitor-protected penicillins, lincosamides, metronidazole, and carbapenems are effective; for Pneumocystis infection, co-trimoxazole is effective.
Among the causative agents of pneumonia in children from 6 months to 6 years
S.pneumoniae
predominates .
H.influenzae
is less common (up to 10%).
Pneumonia caused by M.pneumoniae
is observed in this age group in less than 10% of cases;
C.pneumoniae
.
Treatment of mild, uncomplicated pneumonia in children living in good social conditions is carried out on an outpatient basis using oral medications. AMPs of choice are amoxicillin and macrolides, alternatives are inhibitor-protected penicillins (amoxicillin/clavulanate), cefuroxime axetil.
In children with a tendency to allergic reactions or the development of antibiotic-associated diarrhea, macrolides are preferred.
In children over 7 years old
the main bacterial causative agent
of typical pneumonia
is
S. pneumoniae
(35-40%).
The frequency of atypical
pathogens -
M.pneumoniae
and
C.pneumoniae - is increasing.
Mild pneumonia is treated mainly at home using oral antimicrobial agents. The drugs of choice are amoxicillin or modern macrolides (clarithromycin, roxithromycin, azithromycin).
Severe forms of pneumonia
in children of all ages are an indication for hospitalization. In a hospital setting, it is advisable to carry out stepwise therapy. III-IV generation cephalosporins and inhibitor-protected penicillins are preferred. You can combine β-lactams with modern macrolides, less often with aminoglycosides (netilmicin, amikacin).
Nosocomial pneumonia
In children, the etiology is practically no different from pneumonia in adults. Treatment tactics are developed accordingly.
The use of fluoroquinolones is contraindicated in children. For health reasons, in the absence of a safer alternative, ciprofloxacin may be prescribed. Doxycycline is contraindicated in children under 8 years of age; Co-trimoxazole is not advisable to use in the first 2 months of life.
Complications of ARVI and their danger
In a person with good immunity, acute respiratory diseases go away within a few days, especially if the body is helped to cope with viruses. It is recommended to drink more water, rinse your nose, and gargle. Symptoms can be stopped - bringing down the temperature above 38 degrees, fighting a runny nose, treating the throat with emollients.
However, in some cases, severe viral intoxication or the addition of a bacterial infection can cause complications. Most often, complications arise in the respiratory system and lead to other diseases: tonsillitis, sinusitis, rhinitis, pharyngitis, laryngitis. Often, ARVI develops into bronchitis, otitis media, sinusitis, and pneumonia.
More serious consequences of ARVI threaten people with weakened immune systems. A respiratory infection may not be limited to the respiratory tract and spread to other organs. Severe complications include: pyelonephritis, nephritis, rheumatoid arthritis, neuroinfection.
FEATURES OF TREATMENT OF NPD INFECTIONS IN ELDERLY PEOPLE
In older people, the frequency of PD infections increases, which is associated with such predisposing factors as partial atrophy (especially in smokers) and low activity of the ciliated epithelium of PD, decreased general immunity, and the presence of concomitant diseases. Therefore, antibiotic therapy should be based on the possible influence of these unfavorable factors.
Due to age-related changes in kidney function, it may be necessary to adjust the AMP dosage regimen. This primarily concerns aminoglycosides and co-trimoxazole.
With existing pathology of the liver and gallbladder, it is possible to change the kinetics of a number of AMPs that are metabolized in the liver or excreted in the bile (lincosamides, metronidazole, macrolides). In patients with gallbladder pathology, ceftriaxone should be used with caution due to the increased risk of developing pseudocholelithiasis.
Table 7. Doses of antibiotics for the treatment of urinary tract infections in adults
| A drug | Dose (adults) |
| Benzylpenicillin | 1-3 million units IV every 4-6 hours |
| Oxacillin | 2.0 g IV every 4-6 hours |
| Ampicillin | 0.5-1.0 g orally, 1.0-2.0 g IV or IM every 6 hours |
| Amoxicillin | 0.5 g orally every 8 hours |
| Amoxicillin/clavulanate | 0.625 g orally every 6-8 hours 1.2 g IV every 6-8 hours |
| Ampicillin/sulbactam | 1.5-3.0 g IV, IM every 8-12 hours |
| Ticarcillin/clavulanate | 3.1 g IV every 4-6 hours |
| Piperacillin/tazobactam | 3.375 g IV every 6 hours |
| Cefazolin | 1.0-2.0 g IV, IM every 8-12 hours |
| Cefuroxime | 0.75-1.5 g IV, IM every 8 hours |
| Cefuroxime axetil | 0.5 g orally every 12 hours |
| Cefotaxime | 1.0-2.0 g IV, IM every 4-8 hours |
| Ceftriaxone | 1.0-2.0 g IV, IM every 24 hours |
| Ceftazidime | 2.0 g IV, IM every 8-12 hours |
| Cefoperazone | 1.0-2.0 g IV, IM every 8-12 hours |
| Cefoperazone/sulbactam | 2-4 g IV, IM every 8-12 hours |
| Cefaclor | 0.5 g orally every 8 hours |
| Cefepime | 2.0 g IV every 12 hours |
| Imipenem | 0.5 g IV every 6-8 hours |
| Meropenem | 0.5 g IV every 6-8 hours |
| Aztreons | 2.0 g IV, IM every 8 hours |
| Erythromycin | 0.5 g orally every 6 hours 1.0 g IV every 6 hours |
| Clarithromycin | 0.5 g orally every 12 hours 0.5 g IV every 12 hours |
| Azithromycin | 3-day course: 0.5 g orally every 24 hours 5-day course: 0.5 g on the first day, then 0.25 g every 24 hours |
| Spiramycin | 3 million IU orally every 12 hours 1.5-3.0 million IU IV every 8-12 hours |
| Midecamycin | 0.4 g orally every 8 hours |
| Gentamicin | 4-5 mg/kg/day IV, IM every 24 hours |
| Tobramycin | 5 mg/kg/day IV, IM every 24 hours |
| Netilmicin | 4-6 mg/kg/day IV, IM every 24 hours |
| Amikacin | 15 mg/kg/day IV, IM every 24 hours |
| Ciprofloxacin | 0.5-0.75 g orally every 12 hours 0.4 g IV every 12 hours |
| Ofloxacin | 0.4 g orally and intravenously every 12 hours |
| Levofloxacin | 0.5 g orally every 24 hours 0.5 g IV every 24 hours |
| Moxifloxacin | 0.4 g orally every 24 hours |
| Lincomycin | 0.5 g orally every 6-8 hours 0.6-1.2 g IV, IM every 12 hours |
| Clindamycin | 0.6-0.9 g IV every 8 hours 0.15-0.6 g orally every 6-8 hours |
| Vancomycin | 1.0 g IV every 12 hours |
| Rifampicin | 0.5 g IV every 12 hours |
| Doxycycline | 0.2 g orally or IV every 24 hours |
| Metronidazole | 0.5 g orally every 8 hours 0.5-1.0 g IV every 8-12 hours |
Table 8. Typical errors in antibiotic therapy for NPD infections
| Purpose | A comment |
| By choice of drug | |
| Gentamicin for community-acquired pneumonia | Aminoglycosides are inactive against pneumococcus and atypical microorganisms |
| Ampicillin orally for community-acquired pneumonia | Low bioavailability when taken orally |
| Co-trimoxazole for community-acquired pneumonia | S.pneumoniae and H.influenzae in Russia , frequent allergic skin reactions, availability of safer drugs |
| Routine administration of nystatin | Lack of evidence of the clinical effectiveness of nystatin for candidiasis in patients without immunodeficiency, unreasonable economic costs |
| By timing of initiation of antibiotic therapy | |
| Late initiation of antibiotic therapy | Prescribing AMPs later than 4 hours after the diagnosis of community-acquired pneumonia leads to an increase in mortality |
| By duration of therapy | |
| Frequent changes in AMPs during treatment, “explained” by the danger of developing resistance | Indications for replacing AMPs: a) clinical ineffectiveness, which can be judged after 48-72 hours of therapy; b) development of serious adverse reactions requiring discontinuation of antimicrobial agents; c) high potential toxicity of AMPs (for example, aminoglycosides), limiting the duration of their use |
| Continuation of antibiotic therapy while maintaining individual radiological and/or laboratory changes until their complete disappearance | The main criterion for discontinuing antibiotics is regression of clinical symptoms. The persistence of individual laboratory and/or radiological changes is not an absolute indication for continued antibiotic therapy |



![Table 3. Pharmacokinetic and pharmacodynamic parameters of fluoroquinolones with a single standard dose taken orally [7, 13]](https://irknotary.ru/wp-content/uploads/tablica-3-farmakokineticheskie-i-farmakodinamicheskie-parametry-ftorhinolonov-pri-odnokratnom-prieme-330x140.jpg)