Avamis
The drug is used intranasally.
To achieve maximum therapeutic effect, it is necessary to adhere to a regular regimen of use. The onset of action can be observed within 8 hours after the first administration. It may take several days to achieve maximum effect. The reason for the lack of immediate effect should be carefully explained to the patient.
For the symptomatic treatment of seasonal and year-round allergic rhinitis in adults and adolescents aged 12 years and older, the recommended initial dose is 55 mcg (2 sprays) in each nostril 1 time / day (110 mcg / day).
Once adequate symptom control is achieved, dose reduction to 27.5 mcg (1 spray) in each nostril once a day (55 mcg/day) may be effective for maintenance treatment.
For children aged 2 to 11 years, the recommended initial dose is 27.5 mcg (1 spray) in each nostril 1 time / day (55 mcg / day).
If there is no desired effect at a dose of 27.5 mcg (1 spray) in each nostril 1 time/day, the dose can be increased to 55 mcg (2 sprays) in each nostril 1 time/day (110 mcg/day). When adequate control of symptoms is achieved, it is recommended to reduce the dose to 27.5 mcg (1 spray) in each nostril 1 time / day (55 mcg / day).
There is insufficient data to recommend the use of intranasal fluticasone furoate for the treatment of seasonal and perennial allergic rhinitis in children under 2 years of age.
Elderly patients do not require dose adjustment.
In patients with impaired renal function, no dose adjustment is required.
In patients with mild to moderate liver dysfunction, no dose adjustment is required. There are no data on use in patients with severe liver dysfunction.
Rules for use and handling of the drug
The indicator window in the plastic package allows you to control the level of the drug in the bottle. In 30- or 60-dose vials, the drug level will be visible immediately, and in 120-dose vials, the initial drug level is above the upper limit of the viewing window. The nasal spray is available in orange glass bottles, which are in plastic cases. To check the level of the drug in the bottle, you need to hold it up to the light. The level will be visible through the viewing window.
Preparation for use should be carried out when using the spray for the first time, as well as if the bottle was left open. Proper preparation for use will ensure that the required dose of the drug is injected.
1. Without removing the cap, shake the bottle well for 10 seconds. The drug is a rather thick suspension and becomes more liquid when shaken. Spraying is only possible after shaking.
2. Remove the cap by gently pulling it with your thumb and forefinger.
3. Hold the bottle vertically and point the tip away from you.
4. Press the button firmly and make several presses (minimum 6) until a small cloud appears from the tip (if you cannot press the button with one thumb, you should press it with the thumbs of both hands).
5. The spray is ready for use.
Using a nasal spray
1. Shake the bottle thoroughly.
2. Remove the cap.
3. Clear your nose and tilt your head slightly forward.
4. Insert the tip into one nostril, continuing to hold the bottle vertically.
5. Point the tip of the sprayer at the outer wall of the nose, not at the nasal septum. This will ensure proper injection of the drug.
6. Start inhaling through your nose and press once with your fingers to spray the drug.
7. Remove the atomizer from your nostril and exhale through your mouth.
8. If it is necessary to make two injections into each nostril (as prescribed by a doctor), you should repeat steps 4-6.
9. Repeat the procedure for the other nostril.
10. Close the bottle with a cap.
11. Avoid getting the spray in your eyes. If the drug gets into your eyes, rinse them thoroughly with water.
Sprayer care
After each use:
1. Blot the tip and the inner surface of the cap with a dry, clean cloth. Avoid contact with water.
2. Do not try to clean the tip hole with a pin or other sharp objects.
3. Always cap the bottle and keep it closed. The cap protects the sprayer from dust and clogging, seals the bottle, and prevents accidental pressing of the button.
If the sprayer does not work:
1. Check the level of the remaining drug in the bottle through the viewing window. If there is only a small amount of liquid left, it may not be enough to operate the sprayer.
2. Check the bottle for damage.
3. Check if the tip hole is clogged. Do not attempt to clean the tip hole with a pin or other sharp object.
4. Try to activate the device by repeating the procedure for preparing the nasal spray for use.
Overdose
Symptoms: In a bioavailability study, doses 24 times higher than the recommended adult dose were used intranasally for more than 3 days, and no adverse systemic reactions were observed.
Treatment: Acute overdose is unlikely to require treatment other than medical supervision.
New possibilities of fluticasone furoate (Avamys) in the treatment of allergic rhinitis
The review examines the properties of fluticasone furoate, an intranasal glucocorticoid for the treatment of allergic rhinitis in adults and children over 2 years of age. Distinctive features of FF are high and long-lasting anti-inflammatory activity along with low bioavailability. Clinical studies have shown that, along with nasal medications, the drug consistently reduces the severity of ocular symptoms of allergic rhinitis and has a favorable safety profile. The improved FF delivery system allows for increased patient adherence to therapy. Therapy of allergic rhinitis with the drug "Avamys" significantly improves the quality of life of patients, restores daytime activity, night sleep, performance, reduces the medical and social burden of the disease and the costs of patients for its treatment by reducing the need for other medications.
Fluticasone furoate (Avamys): new opportunities in treatment of allergic rhinitis
This article is a review of the efficacy and safety of the novel intranasal glucocorticoid - fluticasone furoate in the treatment of allergic rhinitis in adults and children (from 2nd year of life). High anti-inflammatory ability and low systemic bioavailability differentiate fluticasone furoate from another intranasal glucocorticoids. Clinical studies have demonstrated that fluticasone furoate is effective against both intranasal and ocular symptoms of allergic rhinitis. Novel delivery system is designed to meet the needs of patients. Avamys allows to improve quality of life, daily activities and reduce allergic rhinitis burden.
Introduction
Allergic rhinitis (AR) is one of the most common diseases, affecting from 10 to 40% of the population in various countries of the world [1, 2]. The significance of the problem of allergic rhinitis is explained by its significant impact on the quality of life of patients, the development of other diseases of the ENT organs (sinusitis, otitis media, eustacheitis, etc.), and its connection with the development of bronchial asthma, which in turn explains the high costs associated with this disease. Only indirect costs caused by AR in the USA reach 9.7 billion dollars per year, in Sweden - 2.7 billion euros per year [3].
Clinical manifestations of AR include nasal (itching, sneezing, rhinorrhea, nasal congestion) and ocular (itching, redness, lacrimation, feeling of sand in the eyes) symptoms. A number of epidemiological studies have shown that signs of eye damage are present in more than 70% of patients with AR [4]. Ocular symptoms significantly reduce the quality of life and performance of patients, and also increase the cost of therapy [5, 6]. One of the reasons for their occurrence is the naso-ocular reflex, which occurs as a result of stimulation of the parasympathetic nerves by mediators of allergic inflammation of the nasal mucosa [7, 8].
Despite a wide arsenal of AR therapy methods, its results often remain unsatisfactory. A telephone survey of 2,500 AR patients in the United States showed that only 49% of them were completely satisfied with their treatment. The reason for refusal of therapy in 37% of cases was the lack of effect, in 35% - a decrease in effectiveness over time, in 32% - the lack of effect within 24 hours, and in 25% - adverse reactions [9]. These data indicate the need to improve pharmacotherapy of allergic rhinitis.
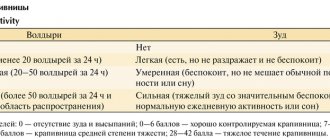
According to international and domestic clinical guidelines, intranasal glucocorticosteroids (InGCS) belong to the main class of drugs for the treatment of AR (Fig. 1). This article is devoted to the InGCS fluticasone furoate (Avamis) recently registered in Russia for the treatment of AR in adults and children over 2 years of age.
Pharmacological properties of fluticasone furoate (FF)
Fluticasone furoate (FF) is a synthetic trifluorinated glucocorticoid with the highest affinity and selectivity for the glucocorticoid receptor among all existing drugs in this group (Fig. 2). It is a combination of the fluticasone molecule and 17-α furoate ester, which provide its main properties (Fig. 3). Although FF is structurally similar to fluticasone propionate (FP), they differ in chemical and pharmacological properties. Neither drug is metabolized in the liver to fluticasone. They are inactivated by the enzyme CYP3A4 of the P450 system with the conversion of the 17b-fluoromethylthioether group and ultimately obtaining various inactive metabolites [10, 11].
Intense hepatic metabolism and high level of binding to plasma proteins (>99%) explain the low bioavailability of FF when administered intranasally (Fig. 3). Intranasal administration of fluticasone furoate at a dose of 110 mcg once daily does not usually result in measurable plasma concentrations (<10 pg/ml). In studies assessing bioavailability in healthy volunteers, the total daily dose of fluticasone furoate was 2640 mcg, which is 24 times the recommended dose, but even so, bioavailability was minimal and was less than 0.5% [15].
A special feature of FF is its high affinity for lung tissue and the epithelium of the nasal mucosa, as well as its good solubility in nasal secretions. It is characterized by high intracellular accumulation and low rate of exit from the cell [10].
Due to the presence of an ester group in fluticasone furoate, which interacts with the 17-α lipophilic site of the glucocorticoid receptor, the molecule is characterized by high affinity for the receptor, rapid association and slow dissociation. High affinity for the glucocorticoid receptor and long-term persistence in tissues explain the high anti-inflammatory potential of FF [10, 19].
Clinical studies of the effectiveness and safety of fluticasone furoate in allergic rhinitis.
Avamys is a well-studied drug with which a large number of preclinical and clinical studies have been conducted.
When choosing the optimal dose of FF (estimated at 55 mcg, 110 mcg, 220 mcg, 440 mcg/day) in patients with seasonal allergic rhinitis (SAR), the most effective and safe dose was 110 mcg once a day [20].
The testing program for SAD in the USA and European countries (including Russia) consisted of 4 double-blind placebo-controlled clinical studies in 1142 patients over 12 years of age, who were prescribed FF for 2 weeks at a dose of 110 mcg during the period of plant dusting. Once a day [21]. The total severity of 4 nasal (itching, sneezing, rhinorrhea, nasal congestion) and 3 ocular (itching/burning, lacrimation, flushing) symptoms was assessed in the morning, evening and immediately before taking the next dose of the drug.
All studies showed that FF, compared with placebo, reduced the severity of all nasal and ocular symptoms and increased the quality of life in patients with SAD. The drug began to act after 8 hours, and its effect persisted throughout the day. The profile of adverse events was the same in the active treatment and placebo groups, with the exception of nasal bleeding, which was slightly more common in FF treatment, but the frequency of its occurrence was the same as with other InGCS [21].
The results obtained in adults and adolescents were comparable to data from a double-blind, placebo-controlled clinical trial in children with SAD aged 2 to 11 years who received FF in doses of 55 mcg and 110 mcg once daily for 2 weeks [ 22].
It has been established that a decrease in the severity of ocular symptoms in patients with SAR is associated with the high local anti-inflammatory activity of FF and its ability to suppress the naso-ocular reflex caused by the activation of parasympathetic nerves by inflammatory mediators in the nasal mucosa [23]. A meta-analysis of 35 double-blind, placebo-controlled studies showed that among all InGCS, only FF reliably demonstrated stable effectiveness against ocular symptoms in SAD patients with sensitization to pollen from trees, grasses and weeds [24].
The efficacy and safety of FF for perennial allergic rhinitis (PAR) was evaluated in adults, adolescents (12 years and older), and children (2–11 years) over a period of 4–12 weeks in several multicenter, double-blind, placebo-controlled studies. Compared with placebo, the drug significantly reduced the severity of nasal and ocular symptoms and increased nasal inspiratory flow rate. The incidence of side effects in the FF group was the same as with placebo. There was no negative effect of FF on cortisol production, intraocular pressure and lens transparency [25-28].
The safety of FF in CAR was studied for 12 months in a double-blind, placebo-controlled study involving 806 patients (12 years and older) from 75 centers in 13 countries [29]. To assess safety, 24-hour cortisol excretion studies, ophthalmoscopy and intraocular pressure measurements, ECG recording, rhinoscopy, clinical laboratory tests, and determination of FF blood concentrations were performed. The efficacy study included a measure of overall nasal symptom severity.
The incidence of adverse events in the active treatment and placebo groups was comparable, with the exception of nasal discharge, which was slightly more common in patients receiving FF. There were no differences between other safety parameters in patients of groups 1 and 2. The concentration of FF in the blood could not be determined. The severity of nasal symptoms in the active treatment group was significantly less than in patients receiving placebo.
The effect of some InGCS (beclomethasone and budesonide) on growth rate in children dictates the inclusion in the research program of new steroid drugs to assess their effects on the musculoskeletal system. Studies conducted with fluticasone furoate (110 mcg once a day) did not reveal its effect on the growth rate of children with SAR and CAP [30].
Pharmacoepidemiological studies of fluticasone furoate
The high cost of treating AR causes a significant economic burden of this disease on the budget of the healthcare system and the patient.
A large pharmacoepidemiological study (data from 793,349 patients was analyzed) showed that the cost of treatment for FF compared to other InGCS was significantly lower (~$5-6 per patient per 60 days). This is due to a decrease (by 21%) in patients’ need for other drugs due to a decrease in the severity of not only nasal but ocular symptoms of AR [31].
Delivery systems for inhaled glucocorticosteroids
Improving InGCS delivery systems is one of the ways to increase patient adherence to treatment and, ultimately, improve the treatment of AR.
A survey of 7000 patients with moderate to severe AR in the United States found that less than 50% found current delivery systems easy to use [32]. Their main disadvantages were named:
1. Unpleasant taste and smell.
2. Lack of information about the remaining drug in the tank.
3. Difficulty pressing the balloon, especially for the elderly and children.
4. The tip is long and rigid, which causes pain and bleeding when inhaled.
5. Spraying the drug in the form of a stream, causing discomfort, nasal congestion and flow of the drug into the throat.
6. Large sizes.
7. Need to activate before regular use.
The new device developed consists of a reservoir with a dosing pump placed in an external container. The innovative delivery system ensures stability and physiological distribution of the drug in the nasal cavity, ease of use and significantly increases patient adherence to therapy. She received a gold Medical Design Excellence Award in 2008 for her outstanding design of a patient-centered device. The main advantages of this innovative system are summarized in Fig. 4.
The development of a device for intranasal administration of FF took place over 2 years. Five systems were tested, followed by interviews with patients and doctors about the advantages and disadvantages of each of them.
Patients noted the ease of use of the Avamys drug delivery system, convenient applicator, and reliability compared to previous intranasal drug administration systems [31]. According to the results of a randomized, double-blind, multicenter study, it turned out that the majority of patients with SAR and CAR prefer the new Avamys nasal spray compared to fluticasone propionate [33].
Conclusion
Thus, the InGCS of fluticasone furoate (Avamys), recently registered in Russia, has pronounced anti-inflammatory activity, as well as the ability, along with nasal ones, to stably reduce the severity of ocular symptoms of AR. A favorable safety profile and an improved delivery system improve patient adherence to therapy. Therapy of allergic rhinitis with the drug "Avamys" significantly improves the quality of life of patients, restores daytime activity, night sleep, performance, reduces the medical and social burden of the disease and the costs of patients for its treatment by reducing the need for other medications. The introduction of InGCS, which are highly effective with an optimal safety profile, into clinical practice will help improve the quality of treatment and quality of life of patients with AR.
A.V. Emelyanov, I.V. Tsukanova
St. Petersburg Medical Academy of Postgraduate Education
Emelyanov Alexander Viktorovich - head of the department of pulmonology with a course in allergology
This article was prepared with the financial support of GlaxoSmithKline.
Fluticasone furoate (Avamis) is a new intranasal glucocorticoid for the treatment of allergic rhinitis.
Literature:
1. Bousquet J., van Cavuwenberge P., Khaltaev N. et al. Allergic rhinitis and its impact on asthma (ARIA). Pocket Guide-WHO, 2001. - 23 p.
2. Bousquet J., Khaltaev N., Cruz A. et al. Allergic rhinitis and its impact on asthma (ARIA) update 2008 (in collaboration with World Health Organization, GA2LEN and AllerGen). Allergy, 2008, v. 63, suppl. 86. - R. 8-160.
3. Hellgren J., Cervin A., Nordling S., Bergman A., Cardell LO Allergic rhinitis and the common cold - high cost to society. Allergy, 2009, epub DOI: 10.1111/j.1398-9995.2009.02269.x.
4. Canonica GW, Bousquet J., Mullol J., Scadding GK, Virchow JC A survey of the burden of allergic rhinitis in Europe. Allergy, 2007, v. 62, suppl 85. - R. 17-25.
5. Gueron B., Demoly P., Mullol J. et al. Quality of life and work productivity in allergic rhinitis patients suffering from both nasal and ocular symptoms—an observational, cross sectional study in four countries in Europe. Allergy, 2009, v. 64, suppl 90, N 866.
6. Gueron B.1., Demoly P., Mullol J. et al. Impact of ocular symptoms on resource utilization and work productivity in management of AR—an observational, cross sectional study in four countries in Europe. Allergy, 2009, v. 64, suppl 90, N 867.
7. Baroody FM, Foster KA, Markaryan A. et al. Nasal ocular reflexes and eye symptoms in patients with allergic rhinitis. Ann Allergy Asthma Immunol., 2008, v 100. - P. 194-199.
8. Naclerio R., Pinto J., de Tineo M., Baroody FM Elucidating the mechanism underlying the ocular symptoms associated with allergic rhinitis. Allergy Asthma Proc., 2008, v. 29. - P. 24-28.
9. Naclerio RM, Hadley JA, Stoloff S., Nelson HS Patient and physician perspectives on the attributes of nasal allergy medications // Allergy Asthma Proc. - 2007. - Vol. 28. - P. S11-S17.
10. Salter M., Biggadike K., Matthews JL et al. Pharmacological propeties of the enhanced-affinity glucocorticoid fluticasone furoate in vitro and in vivo model of respiratory inflammatory disease. Am J Physiol Lung Cell Mol Physiol., 2007, v. 293. P. L660-L667.
11. Hughes S, Shatdlow PC, Hollis FJ et al. Metabolism and disposition of fluticasone furoate, an enhanced-affinity glucocorticoid, in humans. Drug Metabolism and Disposition, 2008, v. 36. - P. 2337-2344.
12. Valotis A., Högger P. Respir Res 2007; 8:54.
13. Salter M. et al. Am J Physiol Lung Cell Mol Physiol 2007; 293:L660-L667.
14. Biggadike K et al. Ann Allergy Asthma Immunol 2007; 98(Suppl 1):A91-A92.
15. Allen A., Down G., Newland A. et al. Absolute bioavailability of intranasal fluticasone furoate in healthy subjects. Clin Ther., 2007, v. 29. - P. 1415-1420.
16. Bryson HM, Faulds D. Drugs 1992; 43: 760-75.
17. Daley-Yates PT, Baker RC Br J Clin Pharmacol 2001; 51: 103-5.
18. Daley-Yates PT et al. Eur J Clin Pharmacol 2004; 60: 265-8.
19. Baumann D., Bachert C., Hogger P. Dissolution in nasal fluid, retention and anti-inflammatory activity of fluticasone furoate in human nasal tissue ex vivo. Clin Exp Allergy, 2009, v. 39. - P. 1540-1550.
20. Martin BG, Rathner PH, Hampbel FC et al. Optimal dose selection of fluticasone furoate nasal spray for the treatment of seasonal allergic rhinitis in adults and adolescents. Allergy Asthma Proc., 2007, v. 28. - P. 216-225.
21. Scadding G., Keith PK Fluticasone furoate nasal spray consistently and significantly improves both the nasal and ocular symptoms of seasonal allergic rhinitis: a review of the clinical data. Expert Opin Pharmacother., 2008, v. 9. - P. 2707-2715.
22. Meltzer EO, Lee J., Tripathy I. et al. Efficacy and safety of once-daily fluticasone furoate nasal spray in children with seasonal allergic rhinitis treated for 2 wk. Pediatr Allergy Immunol., 2009, v. 20. - P. 279-286.
23. Baroody FM, Shenaq D, DeThieno M et al. Fluticasone furoate nasal spray reduces the naso-ocular reflex: a mechanism for the efficacy of topical steroids in controlling allergic eye symptoms. J Allergy Clin Immunol., 2009, v. 123. - P. 1342-1348.
24. Keith P., Scadding G. Are intranasal corticosteroids all equally consistent in managing ocular symptoms of seasonal allergic rhinitis? Curr Med Res Opinion, 2009, v. 25. - P. 2021-2041.
25. Máspero JF, Rosenblut A., Finn A. Jr. et al. Safety and efficacy of fluticasone furoate in pediatric patients with perennial allergic rhinitis. Otorhingol Head Neck Surg., 2008, v. 138. - P. 30-33.
26. Nathan RA, Berger W, Yang W et al. Effect of once-daily fluticasone furoate nasal spray on nasal symptoms in adults and adolescents with perennial allergic rhinitis. Ann Asthma Immunol, 2008, v. 100. - P. 497-505.
27. Vasar M, Houle PA, Douglass JA et al. Fluticasone furoate nasal spray: effective monotherapy for symptoms of perennial allergic rhinitis in adults/adolescents // Allergy Asthma Proc 2008. - Vol. 29. - N 3. - P. 313-321.
28. Meltzer EO, Tripathy I, Máspero JF et al. Safety and tolerability of fluticasone furoate nasal spray once daily in pediatric patients aged 6-11 years with allergic rhinitis: subanalysis of three randomized, double-blind, placebo-controlled, multicentre studies. Clin Drug Investig., 2009, v. 29. - P. 79-86.
29. Rosenblut A., Bardin PG, Muller B. et al. Long term safety of fluticasone furoate nasal spray in adults and adolescents with perennial rhinitis. Allergy, 2007, v. 62. - P. 1071-1077.
30. Gradman J., Caldwell MF, Wolthers OD A 2-week, crossover study to investigate the effect of fluticasone furoate nasal spray on short-term growth in children with allergic rhinitis. Clin Ther., 2007, v. 29. - P. 1738-1747.
31. Garris C., Shan M., D`Souza A., Stanford R. Comparison of corticosteroid nasal sprays in relation to concomitant use and cost of other prescription medications to treat allergic rhinitis symptoms. Retrospective cohort analysis of pharmacy claim data. Clin Drug Invest., 2009, v. 29. - P. 515-526.
32. Berger W., Godfrey JW, Slater A. Intranasal corticosteroids: the development of a drug delivery divice for fluricasone furoate as a potential step toward improved compliance. Expert Opin Drug Deliv., 2007, v. 4. - P. 689-701.
33. Meltzer EO, Stahlman JE, Leflein J. et al. Preferences of adult patients with allergic rhinitis for the sensory attributes of fluticasone furoate versus fluticasone propionate nasal sprays: a randomized, multicenter, double-blind, single-dose, crossover study. Clin Ther., 2008., v. 30. - P. 271-279.
Avamys Spray, 120 d, 27.5 mcg/dose, nasal
Directions for use and doses
Avamis is intended for intranasal use only. To achieve maximum therapeutic effect, it is necessary to adhere to a regular regimen of use. The onset of action can be observed within 8 hours after the first administration. It may take several days to achieve maximum effect. The reason for the lack of immediate effect should be carefully explained to the patient. Treatment of nasal and ocular symptoms of seasonal allergic rhinitis, nasal symptoms of perennial allergic rhinitis in adults and adolescents (aged 12 years and older) The recommended initial dose is 2 sprays (27.5 mcg of fluticasone furoate per spray) in each nostril 1 time / day (110 mcg/day). Once adequate symptom control is achieved, dose reduction to 1 spray in each nostril once a day (55 mcg/day) may be effective for maintenance treatment. Treatment of nasal symptoms of seasonal and year-round allergic rhinitis in children aged 2 to 11 years. The recommended initial dose is 27.5 mcg (1 spray) in each nostril 1 time / day (55 mcg / day). If there is no desired effect at a dose of 27.5 mcg (1 spray) in each nostril 1 time/day, the dose can be increased to 55 mcg (2 sprays) in each nostril 1 time/day (110 mcg/day). When adequate control of symptoms is achieved, it is recommended to reduce the dose to 27.5 mcg (1 spray) in each nostril 1 time / day (55 mcg / day). Children under 2 years of age There are no data to recommend the use of intranasal fluticasone furoate as a treatment for seasonal and perennial allergic rhinitis in children under 2 years of age. Elderly patients No dose adjustment is required (see Pharmacokinetics section). Patients with impaired renal function No dose adjustment is required (see Pharmacokinetics section). Patients with impaired liver function No dose adjustment is required in patients with mild to moderate hepatic impairment (Child-Pugh class A and B). There are no data in patients with severe liver dysfunction (Child-Pugh class C). Caution should be exercised when determining the dose for patients with severe liver dysfunction, because such patients may be more at risk of systemic adverse reactions associated with the use of GCS (see Pharmacokinetics section and Special instructions section). Rules for use and handling of the drug An indicator window in a plastic package allows you to control the level of the drug in the bottle. In 30- or 60-dose vials, the drug level will be visible immediately, and in 120-dose vials, the initial drug level is above the upper limit of the viewing window. The nasal spray is available in orange glass bottles, which are in plastic cases. To check the level of the drug in the bottle, you need to hold it up to the light. The level will be visible through the viewing window. Preparation for use should be carried out when using the spray for the first time, as well as if the bottle was left open. Proper preparation for use will ensure that the required dose of the drug is injected.1. Without removing the cap, shake the bottle well for 10 seconds. The drug is a rather thick suspension and becomes more liquid when shaken. Spraying is possible only after shaking.2. Remove the cap by gently pulling it with your thumb and forefinger.3. Hold the bottle vertically and point the tip away from you.4. Press the button firmly and press several times (minimum 6) until a small cloud appears from the tip (if you cannot press the button with one thumb, you should press it with the thumbs of both hands).5. The spray is ready for use. Using nasal spray1. Shake the bottle thoroughly.2. Remove the cap.3. Clear your nose and tilt your head slightly forward.4. Insert the tip into one nostril, continuing to hold the bottle vertically.5. Point the tip of the sprayer at the outer wall of the nose, not at the nasal septum. This will ensure proper injection of the drug.6. Start inhaling through your nose and press once with your fingers to spray the drug.7. Remove the atomizer from the nostril and exhale through the mouth.8. If it is necessary to make two injections into each nostril (as prescribed by a doctor), you should repeat steps 4-6.9. Repeat the procedure for the other nostril.10. Close the bottle with the cap.11. Avoid getting the spray in your eyes. If the drug gets into your eyes, rinse them thoroughly with water. Caring for the sprayer After each use: 1. Blot the tip and the inner surface of the cap with a dry, clean cloth. Avoid contact with water.2. Do not attempt to clean the tip hole with a pin or other sharp object.3. Always cap the bottle and keep it closed. The cap protects the sprayer from dust and clogging, seals the bottle, and prevents accidental pressing of the button. If the sprayer does not work: 1. Check the level of the remaining drug in the bottle through the inspection window. If only a small amount of liquid remains, it may not be enough to operate the sprayer.2. Check the bottle for damage.3. Check to see if the tip hole is clogged. Do not attempt to clean the tip hole with a pin or other sharp object.4. Try to activate the device by repeating the procedure for preparing the nasal spray for use.