When treating with any medications, you must carefully study the description of the drug and strictly follow the recommendations in the annotation; exceeding the dosage can result in poisoning or death. To rid animals of tuberculosis, Isoniazid is often prescribed - the instructions for use for dogs contain all the necessary information about the rules of safe and effective therapy. But knackers use this product to bait animals, so owners need to know how to help their pet in such cases.
pharmachologic effect
Antituberculosis drug; acts bacteriostatically. It is a prodrug - mycobacterial catalase-peroxidase metabolizes isoniazid to an active metabolite, which, by binding to enoyl (acyl-transfer protein) reductase fatty acid synthase II, disrupts the conversion of delta 2 - unsaturated fatty acids to mycolic acid. The latter is a branched-chain fatty acid that, when combined with arabinogalactan (a polysaccharide), participates in the formation of cell wall components of Mycobacterium tuberculosis. Isoniazid is also an inhibitor of mycobacterial catalase-peroxidase, which reduces the microorganism's defense against reactive oxygen species and hydrogen peroxide. Isoniazid is also active against a small number of strains of Mycobacterium kansasii (for infections caused by this pathogen, sensitivity to isoniazid must be determined before starting treatment).
Composition and what it helps with
Isoniazid (Tubazid) is an effective but very toxic antimicrobial drug that helps with various forms of tuberculosis and is used in the treatment of humans and animals. Produced in light-colored tablets, the drug has a low cost, it can be purchased at a pharmacy without a prescription, the average price is 30–50 rubles.
The medicine contains 0.1, 0.2, 0.3 g of isoniazid, according to the instructions for use, this substance quickly destroys intracellular and extracellular types of mycobacteria - the causative agent of tuberculosis, but is ineffective against other pathogenic microorganisms.
If the Isoniazid tablet gets wet, red or pink stains will form around it - this feature will help the owner quickly determine the type of poison.
Pharmacokinetics
Isoniazid is rapidly and completely absorbed when taken orally; food reduces absorption and bioavailability. The bioavailability indicator is greatly influenced by the “first pass” effect through the liver. The period of maximum concentration is 1 - 2 hours, the maximum concentration after taking a single dose of 300 mg is 3 - 7 mcg/ml. The connection with proteins is insignificant - up to 10%. Volume of distribution - 0.57 - 0.76 l/kg. It is well distributed throughout the body, penetrating into all tissues and fluids, including cerebrospinal, pleural, ascitic; high concentrations are created in lung tissue, kidneys, liver, muscles, saliva and sputum. Penetrates through the placental barrier and into breast milk.
Metabolized in the liver by acetylation to form inactive products. In the liver, it is acetylated by N-acetyltransferase to form N-acetylisoniazid, which is then converted to isonicotinic acid and monoacetylhydrazine, which has a hepatotoxic effect through the formation of an active intermediate metabolite by the cytochrome P450 system during N-hydroxylation. The rate of acetylation is genetically determined; People with “slow” acetylation have little N-acetyltransferase. It is an inducer of the CYP2E1 isoenzyme. The half-life for “fast” acetylators is 0.5 - 1.6 hours; for “slow” ones - 2 - 5 hours. In renal failure, the half-life may increase to 6.7 hours. The half-life for children aged 1.5 to 15 years is 2.3 - 4.9 hours, and for newborns - 7, 8 - 19.8 hours (which is explained by the imperfection of acetylation processes in newborns). Although the half-life varies significantly depending on the individual intensity of acetylation processes, the average half-life is 3 hours (600 mg orally) and 5.1 hours (900 mg). With repeated appointments, the half-life is shortened to 2 - 3 hours.
It is excreted mainly by the kidneys: within 24 hours, 75-95% of the drug is excreted, mainly in the form of inactive metabolites - N-acetylisoniazid and isonicotinic acid. At the same time, in “fast” acetylators the N-acetylisoniazid content is 93%, and in “slow” acetylators it is no more than 63%. Small amounts are excreted in feces. The drug is removed from the blood during hemodialysis; 5-hour hemodialysis allows you to remove up to 73% of the drug from the blood.
Every owner should read and remember this!World has gone mad. Dog-hating is on the rise. The population poisons our dogs with impunity. On the dog hunter forums, recipes and methods on how to kill a dog are described in detail. They poison dogs with various nasty things, but two drugs are 100% lethal if adequate measures are not taken. These are isoniazid and rat poison (rodenticide).
I myself lost a gorgeous young dog who died because he stuck his nose into a rat hole treated with poison and then simply licked his lips. From the moment of the first symptoms to death, only 20 hours passed and all this time the dog was in the clinic... And then 10 years later, her great-niece died according to the same scenario in 22 hours and she spent almost all of this time in the clinic.
Treatment is possible and time is short, but there is. But there is no antidote, and the necessary drug is not certified in Russia. I know what to do with it and I want to share with you. But that’s not all, now there are also targeted baits in the form of meat balls or pieces of sausage stuffed with tablets used in the treatment of tuberculosis and sold in pharmacies without a prescription. When overdosed, these drugs rapidly cause seizures and death. And here there is a way out - there is even an antidote (antidote), but there is very little time!!! But! If you know what to do and have the necessary medications on hand, everything is not so hopeless!
So:
- How to manage to avoid poisoned traps?
- What to do if a dog swallows something on the street?
- What to do if your dog becomes ill and you suspect poisoning?
- Where to look for the necessary drugs. What you should have in your first aid kit.
The first is the most important!
You should always be able to see what your dog is doing at any time of the day while walking. You must teach your dog never to pick up anything from the ground, never to take anything from the hands of strangers! This is the basis of safety! This, no matter how nightmare it sounds, is the basis for the survival of our dogs in the city.
Second most important!
If you see that your dog ate something from the ground or took it and ate it from the hands of a stranger and you can assume that it is poison, then run home and urgently induce vomiting. If you rinsed the dog’s stomach within 15-30 minutes, then further therapy can only be preventive for self-soothing.
How to induce vomiting (gastric lavage).
Hydrogen peroxide is perhaps the best remedy. Mix hydrogen peroxide and water in equal parts and forcefully pour this mixture in the amount of one and a half tablespoons for every 4.5 kg of weight into the dog’s mouth. Vomiting will begin within a few minutes. This is what veterinarians advise. From actual practice, in some cases this amount may not be enough. That's why! We pour in enough so that vomiting begins immediately.
As an example, I can cite a 4.5-month-old Dalmatian puppy who, during a break in class, found and swallowed the whole body of a rat. We immediately poured diluted peroxide into it in the indicated dosage - the puppy slobbered, but did not give up the rat. After some time, they began to pour the solution into him without restriction, about 250 ml of the solution was poured in, and only then did he literally burp this rat like a fountain.
Third.
If your dog suddenly starts bleeding from the anus and vomiting blood and you assume that the dog might have eaten something on the street, run to the clinic. We assume the worst - we tell the doctor that it is possible poisoning with rodenticides (rat poison, coumarins). Urgently! We are looking for the drug vitamin K-1 (phytomenadione, konakion).
If your dog suddenly starts vomiting foam, excessive salivation, loss of coordination, convulsions, and you assume that he ate something on the street, then we assume the worst and begin measures as in the case of isoniazid poisoning. (see below.)
Fourth.
K-1 can be found in online pharmacies, but only injectable. There are no tablets in Russia! You can search on the PesiQ forum in the veterinary section. There are attached topics about this drug. For those who visit Europe, the easiest way is to bring K-1 from there; it is freely sold without a prescription in pharmacies, but also injections, tablets are available in Sweden and the Czech Republic - look for information on the forum.
The antidote to isoniazid is
(pyridoxine) is freely available at any pharmacy. We need ampoules. They cost pennies - just keep it in your first aid kit as a spare. Also, you should always have hydrogen peroxide in your first aid kit to induce vomiting.
And now about the details.
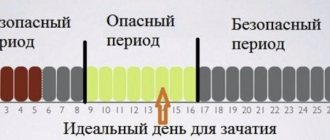
Isoniazid poisoning (the anti-tuberculosis drug is extremely toxic in large doses, it must be swallowed, it is scattered in the form of pieces of minced meat or sausage, if the dog only sniffs or even licks it, it will not be poisoned). Isoniazid is rapidly absorbed, mainly in the small intestine. Its serum concentration reaches a maximum 1-2 hours after administration.
Symptoms:
- Drowsiness, confusion - appear after 30-60 minutes.
- The dog begins to lose coordination, its legs give way, it skids to the sides
- Vomit
- Excessive salivation, foam at the mouth
- In severe poisoning, coma, respiratory depression, convulsions, and lactic acidosis are possible. Seizures are usually prolonged and are not controlled by anticonvulsants. If there are no seizures, then lactic acidosis does not occur. (Acidosis is the accumulation of negatively charged particles (anions) of acids in the blood and other tissues of the body; lactic acidosis is the accumulation of lactate).
Treatment:
1. First of all, immediately introduce vitamin B6! (It is an antidote! Sold freely in any pharmacy!) Intramuscularly, for small dogs, up to approximately 20 kg, about 4-5 ml. More than 20 kg approximately 6-7 ml. There is no need to worry about an overdose of this vitamin. In this situation, in the indicated dosages, it will not harm or kill the animal. It will be worse if you administer lower dosages than indicated, the animal may die.
2. Urgent measures are taken to remove the toxic substance from the gastrointestinal tract, i.e. induce vomiting (see above)
3. After vomiting, adsorbents (activated carbon, enteros gel, or 20 ml diluted Atoxil sorbent with a syringe - it is very powerful and relatively inexpensive compared to enterosgel (and more powerful in action than enterosgel). Isoniazid is well adsorbed.
After all this, urgently go to the clinic for further therapy and be sure to tell the vet what you did at what time in what quantity and what initially happened to the dog.
My comments.
The forums are teeming with descriptions of cases of isoniazid poisoning; almost none of the dogs were saved. Some felt sick while walking and in the conditions of the park there was simply nothing to induce vomiting, and there was no B6 at home. By the time we figured out what was what, by the time we got to the vet, there was no one to help. A close colleague’s dog died from poisoning within an hour and a half. I came back from a walk and started vomiting, so far this and that. It was too late. Don’t waste time - inject the antidote, and then you’ll figure out whether it was necessary or not!
Poisoning with rat poison (rodenticides) - only go to the clinic, urgently!!! If the symptoms are already obvious, if you only assume that the dog has swallowed/licked the poison, urgently lavage the stomach (induce vomiting).
ETIOLOGY
Most rodenticides are anticoagulants. There are 1st generation rodenticides (warfarin (zoocoumarin)) and 2nd generation rodenticides created to get rid of warfarin-resistant rodents (dicumarol, coumafuril, difenacoum, brodifacoum, coumatetralil, bromadiolone, etc.). As a rule, 2nd generation rodeticides have more pronounced toxicity and a longer elimination time (4-6 days versus 14 hours for warfarin).
The mechanism of action of most rodenticides is the inhibition of vitamin K, which is involved in the synthesis of coagulation factors. After entering the body, it takes some time until the body’s own reserves of vitamin K are exhausted, after which, when the synthesis of one’s own vitamin K ceases, a deficiency of coagulation factors gradually develops with all the ensuing consequences.
The typical time for the onset of clinical symptoms varies from 3 to 5 days after rodenticide enters the body.
CLINICAL PICTURE
The most common symptoms in descending order are (in descending order):
- Dyspnea
- Anemia
- Weakness
- Cough/hemoptysis
- Pallor
- Anorexia
- Nose bleed
- Bloody stool
- Vomit
- Lameness
- Subcutaneous hemorrhages
- Hematuria
- Syncope
- Abdominal pain
- Shiver
Diagnosis is based on anamnesis, the clinical symptoms described above, blood tests (anemia (regenerative and non-regenerative), thrombocytopenia, hypoproteinemia, increased alkaline phosphatase (due to hypoxia), possibly a slight increase in liver enzymes, a specific increase in prothrombin time and activated coagulation time and changes in other coagulogram parameters ).
DIFFERENTIAL DIAGNOSIS
Anticoagulant poisoning in dogs and cats should be differentiated from other possible causes of bleeding:
- DIC syndrome
- Hereditary deficiency of clotting factors
- Willerbrand's disease
- Thrombocytopenia or their functional disorders
- Liver diseases
- Canine ehrlichiosis
The response to trial therapy with vitamin K1 allows us to differentiate most of the pathologies listed above.
TREATMENT
It largely depends on the stage at which the patient is delivered to the clinic. In case the poison was eaten a few minutes/hours ago, the necessary actions include a standard decontamination procedure.
Those. induce vomiting and then prescribe sorbents (activated carbon 1 tablet per kg 4 times a day for 2-3 days) followed by laxatives. At this stage, most doctors have a dilemma regarding the use of preventive vitamin K. There is no clear opinion on this matter. The solution to this dilemma should be based on an analysis of the possible dose of poison, the timing of its consumption, and the success of decontamination procedures. If vitamin K therapy is not initiated, coagulation tests should be performed after 24-36 hours and again after 96 hours. If clotting time is prolonged, aggressive vitamin K therapy and plasma transfusion should be initiated.
Treatment of patients admitted to the clinic with bleeding disorders due to the use of rodenticides is based on three principles:
Restore the missing components of the coagulation system (transfusion of plasma or whole blood depending on the number of red blood cells) in order to stop possible bleeding.
Ensure the supply of vitamin K1 so that the liver can begin producing its own clotting factors.
Provide supportive symptomatic therapy and rest (hospitalization in a hospital for at least 24 hours is advisable).
1. With regard to blood transfusion, it is important to remember that in case of severe anemia this is a mandatory component of therapy. In case of mild anemia, plasma transfusion can be given. Plasma is transfused at the rate of 6-10 ml/kg (if necessary, up to 20 ml per day per kg), whole blood depending on the hematocrit (12-20 ml/kg). In extreme cases, autotransfusion of blood from the abdominal/thoracic cavity is possible, not forgetting that we do not replenish clotting factors.
2. Specific therapy involves the introduction of the first loading dose of K1 subcutaneously or orally at the rate of 2.5 mg/kg for first-generation rodenticides and 5.0 mg/kg for second-generation rodenticides; in cases where the generation of the rodenticide is not known, 2.5- 5.0 mg/kg. After administration of the first dose of the antidote, they switch to maintenance therapy with the oral form of the drug at an average rate of 2.5 mg/kg per dose (0.25-2.5 for warfarin poisoning and 2.5-5 mg/kg for poisoning with rodeticides of the 2nd generation), dividing the dose into 2-3 doses.
It is important to give the drug with food, for example canned food, since in this case its effectiveness increases 4-5 times. Side effects with this drug, even at high doses, are extremely rare, so don't be afraid to be aggressive.
The duration of maintenance therapy is 15 days for warfarin, and an average of 1 month for 2nd generation or unknown rodenticides.
The decision to discontinue therapy should be comprehensive and based on a trial withdrawal of the drug after 2-4 weeks and control tests of the blood coagulation system (for example, prothrombin time) 36-48 and 96 hours after discontinuation.
It is important to remember that the drug of choice is K1 (phytomenadione), and not K3 (vicasol).
Vikasol is not able to compensate for the necessary deficiency of vitamin K, while in high doses of 25 mg/kg it can cause liver damage, methemoglobinuria and some other negative consequences, which is why in the states it has been banned for use in veterinary medicine since 1985. If there is no way to get K1 , then you can, of course, try Vikasol (1 amp/kg), but it is important to remember that its effectiveness is questionable and such therapy should be considered more like a therapy of despair.
The onset of clotting factor synthesis after administration of phytamenadione varies from 6 to 12 hours, so you should not forget about plasma transfusion as a source of clotting factor. 3. In addition, depending on the symptoms and results of a blood test, symptomatic therapy is necessary, which usually involves proteolysis inhibitors in high doses (aprotionin - gordox, contrical), antibiotic therapy, oxygen therapy, with the development of disseminated intravascular coagulation syndrome (mini (10 units/kg) or low doses (50-100 units/kg) of heparin, such doses in most cases are not able to significantly worsen coagulopathy).
FORECAST
Patient survival is 83%. Patients suffering from hepatopathy have a much worse prognosis (since vitamin K must be metabolized in the liver). After recovery, patients who have suffered poisoning with 2nd generation rodenticides tend to become more sensitive to subsequent poisonings with rodenticides; it is important to explain this to the owner - next time his pet may have less chance.
And my personal comments.
In my kennel, twice in 2001 and 2011, dogs died from jet bleeding after licking rodenticide. The trouble is that the drug is sold freely in any Sadovod store, and although the packaging says that the antidote (antidote) is vitamin K (vicasol), this is a lie. Antidote - i.e. there is no antidote, and vikasol (K3) is not effective for poisoning.
Our domestic veterinarians in most cases do not know about the existence of K1, they persist and puff out their cheeks, and only the persistence of the owner can encourage them to use this drug, even if you bring it and give it to the veterinarian. It is possible to find K1, at least in large cities, although not easy. Many nurseries have already purchased the drug and keep it in reserve, there are veterinarians who know the scheme of resuscitation measures and subsequent treatment, there are blood and plasma banks. Everything is possible, you just need to act and not fall into a stupor. Even if your dog is lucky and the bleeding is not due to rodenticide poisoning, then K1 will not be superfluous, it copes well with any bleeding and has practically no contraindications. So, its use in case of any bleeding will be justified, and in case of poisoning - the only correct one. But! You should not rely only on K1 alone to solve the problem of poisoning! A set of measures is needed, which are prescribed by the attending physician, based on the dog’s condition. And be prepared for long-term treatment, because any poison completely leaves the body on its own no earlier than after 21 days.
Contraindications
Sensitivity, drug-induced hepatitis and liver failure (due to previous treatment with isoniazid), liver disease in the acute stage, children under 3 years of age (for this dosage form).
With caution
Alcoholism, liver failure, renal failure, seizures, age over 35 years, long-term use of other medications, history of discontinuation of isoniazid therapy, peripheral neuropathy, HIV infection, decompensated diseases of the cardiovascular system (chronic heart failure, angina pectoris, arterial hypertension ), hypothyroidism, pregnancy (do not prescribe at a dose higher than 10 mg/kg).
special instructions
In some cases, fatal drug-induced hepatitis develops during treatment, which can occur even after several months of cessation of use. The risk increases with age (highest incidence in the age group 35 - 64 years), especially with daily ethanol consumption. Therefore, it is necessary to monitor liver function monthly; for persons over 35 years of age, liver function is additionally examined before starting treatment. In addition to ethanol consumption, additional risk factors include chronic liver disease, parenteral drug use, and the postpartum period; under these circumstances, monitoring of liver function (laboratory and clinical) should be carried out more often. Patients should be informed to report any manifestations of liver damage (unexplained anorexia, nausea, vomiting, dark urine, jaundice, rash, paresthesia of the hands and feet, weakness, fatigue or fever lasting more than 3 days, abdominal pain, especially in the right hypochondrium ). In these cases, isoniazid is immediately discontinued.
Patients who have previously suffered isoniazid hepatitis are prescribed alternative anti-tuberculosis drugs. If it is necessary to resume therapy, it is started after complete resolution of clinical and laboratory signs of hepatitis, followed by constant monitoring of liver function. If there are any signs of relapse, isoniazid is immediately discontinued. In patients with acute liver disease, prophylactic isoniazid should be postponed.
To slow down the development of microbial resistance, it is prescribed together with other anti-tuberculosis drugs.
Due to the different metabolic rates, before using isoniazid, it is advisable to determine the rate of its inactivation (based on the dynamics of content in the blood and urine). For “fast” acetylators, isoniazid is used in higher doses.
If there is a risk of developing peripheral neuritis (patients over 65 years of age, concomitant diabetes mellitus, pregnancy, chronic renal failure, alcoholism, hypovitaminosis B6 due to malnutrition, concomitant anticonvulsant therapy), it is recommended to prescribe 10 - 25 mg/day of pyridoxine.
During treatment, you should avoid eating cheese (especially Swiss or Cheshire), fish (especially tuna, sardinella, skipjack), since when they are consumed simultaneously with isoniazid, reactions may occur (skin flushing, itching, sensations of heat or cold, palpitations, increased sweating , chills, headache, dizziness) associated with suppression of the activity of monoamine oxidase and diamine oxidase and leading to disruption of the metabolism of tyramine and histamine contained in fish and cheese.
It should be borne in mind that isoniazid can cause hyperglycemia with secondary glycosuria; copper reduction tests may be false positive; The drug does not affect enzyme tests for glucose.
Taking into account possible side effects, during the treatment period it is necessary to exercise caution when driving vehicles and engaging in other potentially hazardous activities that require increased concentration and speed of psychomotor reactions.
Poisoning a dog with other poisons
Since isoniazid is not the only drug that can cause seizures, it is important to be aware of other toxins. They can also lead to similar poisonings in dogs: bromethalin, metaldehyde, methylxanthines, lead, amphetamines, organophosphates and carbamates, selective serotonin reuptake inhibitors, xylitol, ethylene glycol, strychnine, fluorouracil, ivermectin, fluoroquinolones, lamotrigine, ibuprofen, metronidazole, butadione, vilazodone, diphenhydramine, phenylpropanolamine, 5-hydroxytryptophan, zinc phosphide, Brunfelsia pauciflora and cycas plants.
It is also necessary to distinguish dog poisoning from idiopathic epilepsy. For inflammatory diseases (for example, granulomatous meningoencephalitis). Infectious diseases (for example, rabies). Anatomical abnormalities (eg, hydrocephalus). Neoplasia, hypoglycemia, hypernatremia.
Therefore, it is very important that if your dog experiences seizures, immediately take it to a veterinary clinic. Doctors will be able to perform general clinical and biochemical blood tests and blood gas analysis. Often, when these tests are performed, other signs are discovered. This is metabolic acidosis, hypoglycemia, blood thickening. There may be increased activity of liver enzymes (eg, alkaline phosphatase, alanine aminotransferase, aspartate aminotransferase) and, less commonly, azotemia.
Directions for use and doses
Orally, after meals, 600 - 900 mg/day in 1 - 3 divided doses, maximum single dose - 600 mg, daily dose - 900 mg.
Children - 5 - 15 mg/kg/day, frequency of administration - 1 - 2 times a day, maximum dose - 500 mg/day.
For the purpose of prevention - 5 - 10 mg/kg/day in 2 doses for 2 months.
During pregnancy and in severe cases of pulmonary heart failure, severe atherosclerosis, coronary heart disease and arterial hypertension, dosages of more than 10 mg/kg should not be prescribed.
Side effect
From the nervous system: headache, dizziness, paresthesia, numbness of the extremities, peripheral neuropathy; excessive fatigue or weakness, irritability, euphoria, insomnia, optic neuritis, polyneuritis, toxic psychosis, emotional lability, depression, convulsions, toxic neuropathy, memory impairment.
From the cardiovascular system: palpitations, angina pectoris, increased blood pressure.
From the digestive system: nausea, vomiting, gastralgia; increased activity of alanine aminotransferase, aspartic aminotransferase, hyperbilirubinemia, bilirubinuria, jaundice; rarely - toxic hepatitis, including death.
From the hematopoietic organs: agranulocytosis, hemolytic, sideroblastic or aplastic anemia, thrombocytopenia, eosinophilia.
Allergic reactions: skin rash (measles, maculopapular, exfoliative, purpura), itching, fever, arthralgia, lymphadenopathy, vasculitis.
Metabolism: hypovitaminosis B6, pellagra, hyperglycemia, metabolic acidosis, gynecomastia.
Other: very rarely - menorrhagia, tendency to bleeding and hemorrhage.
If any of the side effects indicated in the instructions worsen, or any other side effects not listed in the instructions are noted, you should immediately inform your doctor.
Overdose
Symptoms appear within 0.5 - 3 hours after administration: nausea, vomiting, dizziness, slurred speech, blurred vision, visual hallucinations. In case of severe overdose: respiratory distress syndrome, depression of the central nervous system quickly moving from stupor to coma, severe intractable convulsions, severe metabolic acidosis, acetonuria, hyperglycemia.
Treatment: in case of severe overdose (80-150 mg/kg), insufficient therapy leads to neurotoxicity with a fatal outcome. With adequate therapy, the prognosis is favorable.
In case of asymptomatic overdose: activated carbon, gastric lavage. When taken at a dose of more than 80 mg/kg, pyridoxine is administered intravenously at the same dose; if the dose of isoniazid taken is unknown, then 5 g of pyridoxine is administered intravenously to adults, and 80 mg/kg to children over 30 to 60 minutes.
For clinical manifestations: adequate ventilation, maintaining the activity of the cardiovascular system, preventing aspiration of gastric contents. If the dose of isoniazid taken is known, the same amount of pyridoxine is administered intravenously over 3 to 5 minutes. If the dose of isoniazid taken is unknown, then 5 g of pyridoxine is administered intravenously to adults, and 80 mg/kg to children. If the cramps do not stop, the dose can be repeated. It is rarely necessary to prescribe a dose of more than 10 g. The maximum safe dose of pyridoxine for an overdose of isoniazid is unknown. If pyridoxine is ineffective, diazepam is prescribed.
It is necessary to monitor the content of electrolytes, urea, glucose and partial pressure of gases in the blood. With the development of metabolic acidosis, sodium bicarbonate may increase hypercapnia (continuous monitoring is required).
Dialysis is prescribed if convulsions and acidosis are not relieved by pyridoxine, diazepam and sodium bicarbonate.
Dangerous dosage
The lethal dose of Isoniazid for dogs is 0.05 g/kg; for small dogs and puppies it is enough to swallow 1 tablet. For poisoning to occur in an adult large dog - more than 5 pieces. An animal cannot swallow such a dose by accident; the poison is mixed into tasty baits by dog hunters who position themselves as fighters against stray animals; they use various methods and techniques to bait dogs.
In addition to Isoniazid, analogues of the drug - Fthisopyram, Hixoside - are also deadly for dogs.
The drug Isoniazid does not have a pronounced taste or smell, so dogs eat the poison without fear. Dog hunters often mix anti-tuberculosis drugs with antiemetic drugs, which significantly increases the likelihood of developing severe consequences.
Signs of poisoning
The main danger of the drug is its immediate effect; signs of intoxication appear in the dog within 20–40 minutes; in case of severe poisoning, death occurs after 3–4 hours.
Symptoms of poisoning:
- increased salivation, lacrimation, foam at the mouth;
- lack of coordination, unsteady gait, weakness in the limbs, the dog begins to fall to one side when walking - deviations are caused by the destructive effect of the drug on the cerebellum;
- convulsions, muscle twitching, epileptic attack, the animal’s head is thrown back and its paws are stretched out - the seizure lasts no more than 20 seconds, involuntary urination and fecal incontinence are often observed;
- confusion, drowsiness, sometimes panic or stupor is observed in the animal - signs indicate serious disturbances in the functioning of the central nervous system;
- vomiting, the masses contain blood, mucus, particles of undigested food;
- rapid breathing, shortness of breath.
If you do not provide timely assistance to your pet, it falls into a coma, and death soon occurs; the mortality rate from this poison among dogs is 100%. Upon autopsy, a large amount of the drug is found in the animal’s liver.
In addition to Isoniazid, dog hunters poison dogs with Digitalis, the antiemetic drug Metoclopramide, Atropine, and arsenic-based drugs. Death in animals occurs after a few hours, but sometimes the suffering of the animal continues for 3-10 days.
Interaction with other drugs
When combined with paracetamol, hepatotoxicity and nephrotoxicity increases; isoniazid induces the cytochrome P450 system, resulting in increased metabolism of paracetamol to toxic products.
Ethanol increases the hepatotoxicity of isoniazid and accelerates its metabolism.
Reduces the metabolism of theophylline, which can lead to an increase in its concentration in the blood.
Reduces metabolic transformations and increases the concentration of alfentanil in the blood.
Cycloserine and disulfiram enhance the adverse central effects of isoniazid.
Increases the hepatotoxicity of rifampicin.
Combination with pyridoxine reduces the risk of developing peripheral neuritis.
Caution should be used in combination with potentially neuro-, hepato- and nephrotoxic drugs due to the risk of increased side effects.
It enhances the effect of coumarin and indanedione derivatives, benzodiazepines, carbamazepine, theophylline, since it reduces their metabolism due to the activation of cytochrome P450 isoenzymes.
Glucocorticosteroids accelerate metabolism in the liver and reduce active concentrations in the blood.
Suppresses the metabolism of phenytoin, which leads to an increase in its concentration in the blood and an increase in the toxic effect (adjustment of the phenytoin dosage regimen may be required, especially in patients with slow acetylation of isoniazid); should be taken into account when prescribing as an anticonvulsant in case of isoniazid overdose.
Antacid drugs (especially aluminum-containing ones) slow down absorption and reduce the concentration of isoniazid in the blood (antacids should be taken no earlier than 1 hour after taking isoniazid).
When used concomitantly with enflurane, isoniazid may increase the formation of an inorganic fluoride metabolite, which has a nephrotoxic effect.
When taken together with rifampicin, it reduces the concentration of ketoconazole in the blood.
Increases the concentration of valproic acid in the blood (control of the concentration of valproic acid is necessary; adjustment of the dosage regimen may be required).
Signs and symptoms of isoniazid poisoning in a dog
Poisoning a dog with isoniazid poison can lead to neurological symptoms. For example, seizures and coma. Gastroenterological symptoms are possible, such as drooling, vomiting, diarrhea. Acid-base imbalances such as metabolic acidosis and hyperthermia (secondary to seizures) occur. Organ damage is also possible - myocardial damage, secondary acute kidney injury, hepatopathy.
Clinical signs of isoniazid poisoning: ataxia, disorientation, dysphoria or euphoria, hypersalivation, vomiting, diarrhea, tachypnea, tachycardia or bradycardia, muscle weakness, hyperesthesia, seizures, hyperthermia, pigmenturia, coma, death.
Seizures are one of the most common symptoms that accompany dog poisoning.
In simple terms, the symptoms of dog poisoning with isoniazid poison are as follows:
- Loss of coordination and weakness, the dog is unable to stand firmly on its feet
- The dog constantly gets sleepy
- Severe vomiting, possibly with blood
- Heavy salivation, possible foam at the mouth
- Convulsive muscle contractions