Pneumonia in children is a fairly common disease, especially at a young age when the immune system is not yet fully developed. This is a lung infection caused by bacteria, fungi or viruses. It is important to carry out proper infection prevention and be attentive to the first symptoms of the disease that occur in young children. Currently, there is a highly effective treatment for pneumonia, but despite this, serious and dangerous complications are possible.
Bacterial pneumonia is characterized by a sudden onset with fever, respiratory distress, chest pain and deterioration in general condition. Symptoms vary depending on the patient's age. Among respiratory diseases, pneumonia is the leading single cause of childhood mortality worldwide, killing approximately 1.1 million patients before the age of 5 years.
Classification of pneumonia
Types of pneumonia are classified according to the cause. The type of microorganism involved, the location where the child was infected, and how the infection occurred are taken into account. According to the conditions of infection, hospital-acquired (nosocomial), intrauterine and community-acquired pneumonia in children is distinguished. The most common type of disease is the latter, which develops at home mainly against the background of ARVI.
Types of pneumonia in children according to the classification used in clinical practice:
· Focal.
The focus of infiltration has a diameter of 0.5 to 1 cm. Individual areas of infiltration can merge, which leads to the formation of a large focus.
· Segmental.
An entire segment of the lung may be involved in the inflammatory process. It is protracted and often complicated by fibrosis or deforming bronchitis.
· Croupous.
It is characterized by a hyperergic inflammatory process that affects the pleural area.
· Interstitial.
Accompanied by proliferation and infiltration of connective tissue. Develops when affected by fungi, viruses and pneumocystis.
According to the severity of the disease, complicated and uncomplicated pneumonia are distinguished. When complications develop, pulmonary edema, pulmonary insufficiency, pleurisy or abscess are observed. Cardiovascular disorders cannot be excluded.
Along the way, protracted and acute pneumonia in children are distinguished. In the second case, the disease resolves within 4-6 weeks. In a prolonged form, the inflammatory process persists for more than one and a half months. According to etiology, fungal, bacterial, viral and parasitic pneumonia are distinguished.
The clinical classification of childhood pneumonia is important for doctors, because, knowing the place and time of infection of the child, it is possible to determine the form of the pathogen that caused the pneumonia and, accordingly, prescribe effective treatment.
Pneumonia among all pulmonary pathologies in young children is almost 80%. Even with the introduction of progressive technologies in medicine - the discovery of antibiotics, improved diagnostic and treatment methods - this disease is still one of the ten most common causes of death. According to statistical data in various regions of our country, the incidence of pneumonia in children is 0.4-1.7%.
- Improper treatment of influenza and ARVI can lead to pneumonia in a child
- Pneumonia in children - differential diagnosis of ARVI, acute bronchitis and bronchiolitis
- Signs of pneumonia in a child. Symptoms of pneumonia in infants, children under one year old
- Chlamydial, mycoplasma pneumonia in a child
- Indications for hospitalization
- Treatment of pneumonia in a child
When and why can pneumonia occur in a child?
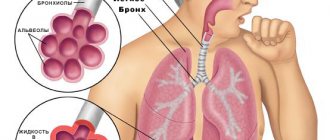
The lungs perform several important functions in the human body. The main function of the lungs is gas exchange between the alveoli and the capillaries that envelop them.
Simply put, oxygen from the air in the alveoli is transported into the blood, and carbon dioxide from the blood enters the alveoli.
They also regulate body temperature, regulate blood clotting, are one of the filters in the body, promote cleansing, the removal of toxins, breakdown products that occur during various injuries, and infectious inflammatory processes. And in the event of food poisoning, burns, fractures, surgical interventions, or any serious injury or illness, a general decrease in immunity occurs, and it is more difficult for the lungs to cope with the load of filtering toxins.
That is why very often a child develops pneumonia after suffering or against the background of injuries or poisoning.
Most often, the causative agent of the disease is pathogenic bacteria - pneumococci, streptococci and staphylococci, and recently cases of the development of pneumonia from pathogens such as pathogenic fungi, legionella (usually after staying in airports with artificial ventilation), mycoplasma, chlamydia, which are not They are rarely mixed or associated.
Pneumonia in a child, as an independent disease that occurs after serious, severe, prolonged hypothermia, is extremely rare, since parents try to prevent such situations.
As a rule, in most children, pneumonia does not occur as a primary disease, but as a complication after ARVI or influenza, less often than other diseases.
Why is this happening?
Many of us believe that acute viral respiratory diseases have become more aggressive and dangerous due to their complications in recent decades. This may be due to the fact that both viruses and infections have become more resistant to antibiotics and antiviral drugs, which is why they are so severe in children and cause complications.
One of the factors in the increase in the incidence of pneumonia in children in recent years has been the general poor health of the younger generation - how many children today are born with congenital pathologies, developmental defects, and lesions of the central nervous system.
A particularly severe course of pneumonia occurs in premature or newborn babies, when the disease develops against the background of an intrauterine infection with an insufficiently formed, immature respiratory system.
In congenital pneumonia, the causative agents are often herpes simplex virus, cytomegalovirus, mycoplasma, and when infected during childbirth - chlamydia, group B streptococci, opportunistic fungi, Escherichia coli, Klebsiella, anaerobic flora; when infected with hospital infections, pneumonia begins on the 6th day or 2 weeks after birth.
Naturally, pneumonia most often occurs in cold times, when the body already undergoes a seasonal adjustment from heat to cold and vice versa, overloads occur for the immune system, at this time there is a lack of natural vitamins in foods, temperature changes, damp, frosty, windy weather contribute to hypothermia of children and their infection.
In addition, if a child suffers from any chronic diseases - tonsillitis, adenoids in children, sinusitis, dystrophy, rickets (see rickets in an infant), cardiovascular disease, any severe chronic pathologies, such as congenital lesions of the central nervous system, developmental defects, immunodeficiency states - significantly increase the risk of developing pneumonia and aggravate its course.
The severity of the disease depends on:
- Extensiveness of the process (focal, focal-confluent, segmental, lobar, interstitial pneumonia).
- The age of the child, the younger the baby, the narrower and thinner the airways, the less intense gas exchange in the child’s body and the more severe the course of pneumonia.
- Places where and for what reason pneumonia occurred:
— community-acquired: most often have a milder course
— hospital: more severe, since infection with bacteria resistant to antibiotics is possible
- aspiration: when foreign objects, mixture or milk enter the respiratory tract.
The most important role is played by the general health of the child, that is, his immunity.
Improper treatment of influenza and ARVI can lead to pneumonia in a child
When a child gets sick with a common cold, acute respiratory viral infection, or influenza, the inflammatory process is localized only in the nasopharynx, trachea and larynx.
If the immune response is weak, and also if the pathogen is very active and aggressive, and the child is treated incorrectly, the process of bacterial reproduction descends from the upper respiratory tract to the bronchi, then bronchitis may occur. Further, inflammation can also affect lung tissue, causing pneumonia.
What happens in a child’s body during a viral disease?
In most adults and children, various opportunistic microorganisms - streptococci, staphylococci - are always present in the nasopharynx, without causing harm to health, since local immunity inhibits their growth.
However, any acute respiratory disease leads to their active reproduction, and if the parents act correctly during the child’s illness, the immune system does not allow their intensive growth.
What should not be done during ARVI in a child to avoid complications:
Antitussives should not be used.
Coughing is a natural reflex that helps the body clear the trachea, bronchi and lungs of mucus, bacteria, and toxins. If, to treat a child, in order to reduce the intensity of a dry cough, you use antitussives that affect the cough center in the brain, such as Stoptusin, Bronholitin, Libexin, Paxeladin, then an accumulation of sputum and bacteria in the lower respiratory tract may occur, which ultimately leads to pneumonia.
You cannot carry out any preventive antibiotic therapy for colds or viral infections.
Antibiotics are powerless against the virus, but the immune system must cope with opportunistic bacteria, and their use is indicated only if complications arise as prescribed by a doctor.
The same applies to the use of various nasal vasoconstrictors; their use promotes faster penetration of the virus into the lower respiratory tract, therefore Galazolin, Naphthyzin, Sanorin are not safe to use for a viral infection.
Drinking plenty of fluids - one of the most effective methods of relieving intoxication, thinning mucus and quickly clearing the airways is drinking plenty of fluids, even if the child refuses to drink, parents should be very persistent.
If you do not insist that the child drinks a sufficiently large amount of liquid, there will also be dry air in the room - this will help dry out the mucous membrane, which can lead to a longer course of the disease or a complication - bronchitis or pneumonia.
Constant ventilation, the absence of carpets and rugs, daily wet cleaning of the room in which the child is located, humidification and purification of the air using a humidifier and air purifier will help to quickly cope with the virus and prevent pneumonia from developing. Because clean, cool, moist air helps to thin sputum, quickly eliminate toxins through sweat, cough, and wet breath, which allows the child to recover faster.
Acute bronchitis and bronchiolitis - differences from pneumonia
ARVI usually has the following symptoms:
- High temperature in the first 2-3 days of illness (see antipyretics for children)
- Headache, chills, intoxication, weakness
- Qatar of the upper respiratory tract, runny nose, cough, sneezing, sore throat (not always the case).
In case of acute bronchitis against the background of acute respiratory viral infection, the following symptoms may occur:
- Slight increase in body temperature, usually up to 38C.
- At first the cough is dry, then it becomes wet, there is no shortness of breath, unlike pneumonia.
- Breathing becomes harsh, various scattered wheezes appear on both sides, which change or disappear after coughing.
- The radiograph shows an increase in the pulmonary pattern, and the structure of the roots of the lungs decreases.
- There are no local changes in the lungs.
Bronchiolitis occurs most often in children under one year of age:
- The difference between bronchiolitis and pneumonia can only be determined by X-ray examination, based on the absence of local changes in the lungs. According to the clinical picture, acute symptoms of intoxication and an increase in respiratory failure, the appearance of shortness of breath - are very similar to pneumonia.
- With bronchiolitis, the child’s breathing is weakened, shortness of breath with the participation of auxiliary muscles, the nasolabial triangle becomes bluish, general cyanosis and severe pulmonary heart failure are possible. When listening, a boxy sound and a mass of scattered fine-bubble rales are detected.
Signs of pneumonia in a child
When the infectious agent is highly active, or when the body’s immune response to it is weak, when even the most effective preventive treatment measures do not stop the inflammatory process and the child’s condition worsens, parents can guess from some symptoms that the child needs more serious treatment and urgent medical examination.
At the same time, under no circumstances should you start treatment with any traditional method. If it really is pneumonia, not only will this not help, but the condition may worsen and time will be lost for adequate examination and treatment.
Symptoms of pneumonia in a child 2 - 3 years old and older
How can attentive parents determine if they have a cold or viral illness that they should urgently call a doctor and suspect pneumonia in their child?
Symptoms that require x-ray diagnostics:
- After an acute respiratory infection or flu, there is no improvement in the condition for 3-5 days, or after a slight improvement, a jump in temperature and increased intoxication and cough reappear.
- Lack of appetite, lethargy of the child, sleep disturbances, and moodiness persist for a week after the onset of the illness.
- The main symptom of the disease remains a severe cough.
- The body temperature is not high, but the child has shortness of breath. At the same time, the number of breaths per minute in a child increases, the norm of breaths per minute in children aged 1-3 years is 25-30 breaths, in children 4-6 years old - the norm is 25 breaths per minute, if the child is in a relaxed, calm state. With pneumonia, the number of breaths becomes greater than these numbers.
- With other symptoms of a viral infection - cough, fever, runny nose - pronounced pallor of the skin is observed.
- If the temperature is high for more than 4 days and antipyretics such as Paracetamol, Efferalgan, Panadol, Tylenol are not effective.
Symptoms of pneumonia in infants, children under one year old
The mother can notice the onset of the disease by changes in the baby’s behavior. If a child constantly wants to sleep, becomes lethargic, apathetic, or vice versa, is capricious a lot, cries, refuses to eat, and the temperature may rise slightly, the mother should immediately consult a pediatrician.
Body temperature
In the first year of life, pneumonia in a child, the symptom of which is considered to be a high, unbroken temperature, is distinguished by the fact that at this age it is not high, does not reach 37.5 or even 37.1-37.3.
However, temperature is not an indicator of the severity of the condition.
The first symptoms of pneumonia in an infant
This is causeless anxiety, lethargy, loss of appetite, the baby refuses to breastfeed, sleep becomes restless, short, loose stools appear, there may be vomiting or regurgitation, runny nose and paroxysmal cough, which intensifies while the baby is crying or feeding.
Baby's breathing
Chest pain when breathing and coughing.
Sputum - with a wet cough, purulent or mucopurulent sputum (yellow or green) is released.
Shortness of breath or an increase in the number of breathing movements in young children is a clear sign of pneumonia in a child. Shortness of breath in infants may be accompanied by nodding of the head in time with breathing, and the baby also puffs out his cheeks and stretches out his lips, sometimes foamy discharge appears from the mouth and nose.
A symptom of pneumonia is considered to be exceeding the normal number of breaths per minute:
- In children under 2 months, the norm is up to 50 breaths per minute; over 60 is considered a high frequency.
- In children from 2 months to a year, the norm is 25-40 breaths, if 50 or more, then this is exceeding the norm.
- In children older than one year, the number of breaths exceeding 40 is considered shortness of breath.
Skin texture changes when breathing
Attentive parents may also notice retraction of the skin when breathing, usually on one side of the diseased lung.
To notice this, you should undress the baby and observe the skin between the ribs; it retracts when breathing. With extensive lesions, one side of the lung may lag behind during deep breathing.
Sometimes you can notice periodic stops in breathing, disturbances in the rhythm, depth, frequency of breathing, and the child’s desire to lie on one side.
Cyanosis of the nasolabial triangle
This is the most important symptom of pneumonia, when blue skin appears between the baby’s lips and nose. This sign is especially pronounced when the baby is breastfeeding.
With severe respiratory failure, slight blue discoloration may appear not only on the face, but also on the body.
Chlamydial, mycoplasma pneumonia in a child
Among pneumonias, the causative agents of which are not common bacteria, but various atypical representatives, mycoplasma and chlamydial pneumonia are distinguished.
In children, the symptoms of such pneumonia are somewhat different from the course of ordinary pneumonia. Sometimes they are characterized by a hidden, sluggish course.
Signs of atypical pneumonia in a child may be as follows:
- The onset of the disease is characterized by a sharp rise in body temperature to 39.5 C, then a persistent low-grade fever forms -37.2-37.5 or even normalization of temperature occurs.
- It is also possible that the disease begins with the usual signs of ARVI - sneezing, sore throat, severe runny nose.
- Persistent dry debilitating cough, shortness of breath may not be constant. This cough usually occurs with acute bronchitis, not pneumonia, which complicates the diagnosis.
- When listening, the doctor is most often presented with scant data: rare wheezing of various sizes, pulmonary percussion sound. Therefore, it is difficult for a doctor to determine atypical pneumonia based on the nature of wheezing, since there are no traditional signs, which greatly complicates the diagnosis.
- There may be no significant changes in the blood test for SARS. But usually there is an increased ESR, neutrophilic leukocytosis, combination with anemia, leukopenia, eosinophilia.
- A chest x-ray reveals a pronounced increase in the pulmonary pattern and heterogeneous focal infiltration of the pulmonary fields.
- Both chlamydia and mycoplasma have the ability to exist for a long time in the epithelial cells of the bronchi and lungs, so most often pneumonia is of a protracted, recurrent nature.
- Treatment of atypical pneumonia in a child is carried out with macrolides (azithromycin, josamycin, clarithromycin), since the pathogens are most sensitive to them (to tetracyclines and fluoroquinolones, too, but they are contraindicated for children).
Indications for hospitalization
The decision about where to treat a child with pneumonia - in a hospital or at home - is made by the doctor, and he takes into account several factors:
The severity of the condition and the presence of complications - respiratory failure, pleurisy, acute disturbances of consciousness, heart failure, drop in blood pressure, lung abscess, pleural empyema, infectious-toxic shock, sepsis.
Damage to several lobes of the lung. Treatment of focal pneumonia in a child at home is quite possible, but for lobar pneumonia it is better to treat it in a hospital setting.
Social indications are poor living conditions, inability to carry out care and doctor’s orders.
Age of the child - if an infant falls ill, this is grounds for hospitalization, since pneumonia in an infant poses a serious threat to life. If pneumonia develops in a child under 3 years of age, treatment depends on the severity of the condition and most often doctors insist on hospitalization. Older children can be treated at home, provided that the pneumonia is not severe.
General health - in the presence of chronic diseases, weakened general health of the child, regardless of age, the doctor may insist on hospitalization.
Treatment of pneumonia in a child
Antibiotics are the mainstay of treatment for pneumonia. At a time when doctors did not have antibiotics in their arsenal for bronchitis and pneumonia, pneumonia was a very common cause of death in adults and children, so in no case should you refuse to use them; no folk remedies are effective for pneumonia.
Parents are required to strictly follow all the doctor’s recommendations, provide proper care for the child, adhere to the drinking regime, nutrition:
Taking antibiotics must be carried out strictly on time; if the drug is prescribed 2 times a day, this means that there should be a break of 12 hours between doses, if 3 times a day, then a break of 8 hours. Antibiotics are prescribed - penicillins, cephalosporins for 7 days, macrolides (azithromycin, josamycin, clarithromycin) - 5 days. The effectiveness of the drug is assessed within 72 hours - improvement in appetite, decrease in temperature, shortness of breath.
Antipyretics are used if the temperature is above 39C , in infants above 38C. At first, antipyretic antibiotics are not prescribed, since it is difficult to assess the effectiveness of therapy. It should be remembered that during high temperatures the body produces the maximum amount of antibodies against the pathogen, so if a child can tolerate a temperature of 38C, it is better not to knock it down. This way the body can quickly cope with the microbe that caused pneumonia in the baby. If a child has had at least one episode of febrile convulsions, the temperature should be brought down already at 37.5C.
Feeding a child with pneumonia - lack of appetite in children during illness is considered natural and the child’s refusal to eat is explained by the increased load on the liver when fighting the infection, so you cannot force feed the child. If possible, you should prepare light food for the patient, exclude any ready-made chemicalized foods, fried and fatty, try to feed the child simple, easily digestible food - porridge, soups with a weak broth, steamed cutlets from lean meat, boiled potatoes, various vegetables, fruits.
Oral hydration - in water, natural freshly squeezed diluted juices - carrot, apple, weakly brewed tea with raspberries, rosehip infusion, water-electrolyte solutions are added (Rehydron, etc.).
Ventilation, daily wet cleaning, and the use of air humidifiers alleviate the baby’s condition, and the love and care of parents works wonders.
No general tonic (synthetic vitamins), antihistamines, or immunomodulators are used, since they often lead to side effects and do not improve the course and outcome of pneumonia.
Taking antibiotics for pneumonia in a child (uncomplicated) usually does not exceed 7 days (macrolides 5 days), and if you follow bed rest, follow all the doctor’s recommendations, in the absence of complications, the child will quickly recover, but within a month there will still be residual effects in the form cough, slight weakness.
With atypical pneumonia, treatment may take longer. P
When treated with antibiotics, the intestinal microflora in the body is disrupted, so the doctor prescribes probiotics - RioFlora Immuno, Acipol, Bifiform, Bifidumbacterin, Normobact, Lactobacterin.
To remove toxins after completion of therapy, the doctor may prescribe sorbents such as Polysorb, Enterosgel, Filtrum.
If the treatment is effective, the child can be transferred to a general regimen and walks from the 6-10th day of illness, and hardening can be resumed after 2-3 weeks.
In case of mild pneumonia, heavy physical activity (sports) is allowed after 6 weeks, in case of complicated pneumonia after 12 weeks.
Source: https://zdravotvet.ru/
Treatment of pneumonia in children
There are several treatment methods for pneumonia that are aimed at relieving symptoms and neutralizing the existing infection. In case of bilateral pneumonia in children, urgent hospitalization in a hospital is recommended, and in severe cases - in the intensive care unit.
To treat pneumonia in children, the following is carried out:
· elimination of infectious and inflammatory process in the lungs;
· detoxification of the body;
· elimination of respiratory failure.
Etiological treatment is carried out immediately after admission to the hospital, after taking samples of biomaterial for bacteriological examination.
Today, for the treatment of pneumonia in children, it has been decided to use step-by-step antibacterial therapy:
To improve the condition, antibiotics are prescribed parenterally (intravenously, intramuscularly), then orally;
· detoxification is carried out by drip parenteral crystalloids, glucose-physiological solution, diuretics;
· if necessary, oxygen therapy is prescribed to correct the composition of gas in the blood (in case of respiratory alkalosis), and in severe cases, it is connected to a mechanical ventilation device;
· to improve the outflow of mucus from the lungs, bronchodilators are prescribed;
· For persistent dry cough, antitussives are prescribed.
After normalizing body temperature, it is recommended to conduct a course of massage, physiotherapeutic procedures, and therapeutic exercises.
Even when the likelihood of a bacterial infection is high, it takes time to identify the bacteria involved and choose the best antibiotic to eliminate it. For viral pneumonia, specific antiviral drugs can be used. If the causative agent is a fungus, then the doctor prescribes antifungal drugs. To increase the effectiveness of treatment, your doctor may recommend using a nebulizer.
General information about the disease
When a child gets sick with ARVI, a lot of mucus is produced in his bronchi. It tends to accumulate, especially in preschoolers, because their chest muscles are not yet developed enough for effective coughing. As a result, some areas of the lungs are deprived of ventilation and become vulnerable to pathogens. Viruses and bacteria settle in them, causing inflammation. In the viral form, the disease goes away in about 5-6 days without treatment, and if it is caused by bacteria, then special therapy is required.
Attention! Treatment must be precisely targeted to the pathogen; individual selection of the drug and dosage is necessary. Self-medication can lead to irreversible consequences.
Pneumonia can occur even in a newborn; it is of aspiration origin in this case, that is, the cause is the baby swallowing amniotic fluid during childbirth.
The disease has an excellent prognosis if treatment is started on time. Complicated cases requiring hospital treatment with intravenous drugs are only 8-10%.
Causes of pneumonia in childhood
- improper therapy for ARVI, self-medication;
- complication of other respiratory diseases;
- infections (in exceptional and very rare cases, a bacterial disease can be contagious);
- weak immunity as a factor that expands the number of causes of pneumonia - even injury.
The nature of the disease may even be toxicological. The mechanism of our body’s work is such that with a huge number of ailments, harmful, toxic – “garbage” – substances filtered by the circulatory system settle in the lungs. Due to this, “weak” areas and local blockages are formed. Infections, viruses, and inflammation then develop in them. Even ailments not directly related to the respiratory system often lead to pneumonia.
Prognosis and prevention
The best treatment for pneumonia is prevention. Vaccines are available for children from two months of age. It is important to take care of the diet of a patient with pneumonia. During treatment, rest, bed rest and plenty of fluids are recommended to prevent dehydration of the baby's body after the formation of a large amount of mucus and due to increased sweating.
Typically, at the onset of the disease, children experience loss of appetite, but as they recover, it returns to normal. A healthy and nutritious diet is recommended to avoid nutritional deficiencies that can lead to other disorders in the body.
It is necessary to control the environment in which the patient is located, whether in a medical facility or at home. Avoid the presence of smoke (such as tobacco) or other lung irritants that may aggravate the condition.
After discharge from the hospital, children require clinical observation and rehabilitation measures. It is also recommended to strictly follow the doctor’s recommendations after recovery, correct daily routine, and moderate intake of vitamins as a preventive measure. Dosed physical activity contributes to the overall recovery of children and can prevent recurrence of pneumonia.
Pneumonia in children - treatment at the RebenOK clinic in Moscow
Our medical center employs pediatricians who have extensive practical experience. Treatment of pneumonia in children is carried out after confirming the diagnosis and determining the type of pathogen, which allows you to get a quick result. Competent specialists determine the symptoms of latent pneumonia in children, which occurs without fever and wheezing.
If signs of a cold appear, it is recommended to consult a pediatrician to rule out the presence of pneumonia or prevent the development of the disease. We use modern diagnostic equipment and prescribe treatment in accordance with international protocols, taking into account the individual characteristics of the patient.
Literature:
1. Erzhanova G.E. Pneumonia in children // Bulletin of the Kazakh National Medical Institute, 2014. URL: https://cyberleninka.ru/article/n/pnevmonii-u-detey (access date: 09/02/2021)
2. Sergeeva E.V., Petrova S.I. Community-acquired pneumonia in children. Modern features // Pediatrician Magazine, 2021. URL: https://cyberleninka.ru/article/n/vnebolnichnaya-pnevmoniya-u-detey-sovremennye-osobennosti (access date: 09/02/2021)
3. Geppe N.A., Kozlova L.V., Kondurina E.G. Community-acquired pneumonia in children // Clinical manual "Moscow Society of Children's Doctors", 2021. URL: https://pulmodeti.ru/wp-content/uploads/Vnebolnichnaya.pdf (access date: 09/02/2021)
4. Petchenko A.I., Luchaninova V.N., Knysh S.V.
Age-related features of the course of community-acquired pneumonia in children // Journal “Fundamental Research” No. 2, 2014. URL: https://fundamental-research.ru/ru/article/view?id=33563 (access date: 09/02/2021) 5. Kakeeva A.A., Bokonbaeva S.D., Dzhanabilova G.A. Etiological structure of community-acquired pneumonia in young children // Journal “Modern Problems of Science and Education” No. 3, 2021. URL: https://science-education.ru/ru/article/view?id=30897 (access date: 02.09. 2021)
Types of disease
There are several classification signs of pneumonia in an infant:
- the causative agents of the disease are viral, fungal and bacterial pneumonia, which requires treatment with antibiotics;
- according to the degree of tissue damage in the lungs, they are divided into focal (small areas), total (one whole lung) and bilateral (both lungs at once), while the process from focal to bilateral develops very quickly;
- According to the method of infection, they distinguish intrauterine, acquired, aspiration (entry of amniotic fluid into the child’s respiratory system) and birth (passage of the infected birth canal).
The type of disease is determined in order to select the appropriate treatment.