Left ventricular failure is a violation of myocardial contractility in the area of the specified chamber.
As a result of the course of the condition, blood is released into the aorta, and therefore the large circle, in insufficient quantities. All organs and systems suffer. Including the myocardium itself. Ischemia occurs (oxygen starvation).
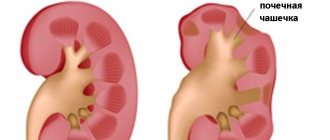
On the other hand, if the pathological process is associated with regurgitation (reverse flow of blood from the left ventricle into the left atrium), dilatation occurs (expansion of both chambers). Increased load leads to the development of cardiomyopathy (organic changes in the myocardium).
These two factors determine the relatively early onset of critical condition. Death is the most likely outcome.
Treatment is carried out under the supervision of a cardiologist or specialized surgeon, depending on the condition and underlying cause.
The mechanism of pathology development
Normally, blood moves from the right side of the heart to the left ventricle, then is released into the aorta and moves in a large circle, providing nutrition to all organs and systems, including the brain.
LVAD develops as a result of exposure to a negative factor, usually mitral or aortic valve insufficiency or pathology of the interventricular septum.
The result of the violation is, on the one hand, a decrease in myocardial contractility as a result of overload. Accordingly, not enough blood is released.
On the other hand, stagnation of liquid connective tissue, which leads to dilatation (expansion) of cardiac structures and an even greater decrease in the organ’s ability to function normally.
The heart cannot function like this for a long time. Therefore, within a few years, death occurs. The progression is rapid.
The condition needs to be treated from the very first months, or preferably weeks, in a hospital setting. The basis of therapy is eliminating the cause of the phenomenon.
What is heart failure?
Our heart is like a pump that pumps blood and supplies oxygen and nutrients to all parts of the body. Impaired ability of the heart to pump blood leads to stagnation and leads to the development of heart failure .
Poor blood supply puts other organs and tissues at risk. In terms of prevalence, heart failure rivals the most well-known infectious diseases.
According to statistics, around 28 million people suffer from heart failure throughout Europe. In our country, the number of patients with this disease exceeds 9 million (more than 25% of them are under 60 years of age)! At the same time, Russians die from it 10 times more often than from myocardial infarction.
1 Tests for heart failure
2 Tests for heart failure
3 Tests for heart failure
Classification
This is done for a number of reasons.
Based on the nature of the pathological process:
- Acute left ventricular failure. Develops in minutes. Accompanied by a critical drop in myocardial contractility and impaired circulation of all organs.
Associated with intense symptoms: chest pain, arrhythmia, fainting and others. Considered an emergency. Leads to cardiogenic shock, which is fatal in almost 100% of cases.
If you're lucky, the attack will be a signal, but not the cause of death. The acute process is stopped in the hospital, then long-term observation by a cardiologist is indicated.
- Chronic type. Develops in 80% of cases without a prior emergency condition. Determined by the minimal clinical picture.
For a long time, sometimes until death from cardiac shock and cardiac arrest, the patient is unaware of his own condition.
The prognosis is determined by the moment of detection and the root cause. It often turns out to be too late. Therefore, any discomfort should be grounds for urgent treatment at the hospital.
Left ventricular failure is almost always secondary in origin. That is, it is caused by other diseases. Usually cardiac.
Tests and diagnostics
Diagnosis of cardiogenic shock is based on data from a physical examination, instrumental and laboratory examinations. During an external examination, a cardiologist or resuscitator pays attention to external signs of the disease:
- sweating;
- pallor;
- marbling of the skin.
Objective diagnosis includes:
- Physical examination of the patient. A decrease in blood pressure to 90/50 mmHg is typical. Art. and below, the pulse rate can drop below 200 mm Hg. Hypotension may be absent in the initial stages of the disease, which is explained by the launch of the body’s compensatory capabilities. Heart sounds are muffled; when listening to the lungs, fine moist rales are noted.
- Electrocardiography. On an ECG in standard 12 leads, characteristic signs of myocardial infarction are recorded: ST segment displacement; decreased amplitude of the R wave; negative T wave. Additionally, atrioventricular blockades and extrasystole .
- Laboratory tests and examinations. The concentration of electrolytes, troponin, urea, creatinine, liver enzymes, and glucose is assessed. Already in the first hours after myocardial infarction, the level of troponins I and T increases. By increasing the concentration of urea, sodium and creatinine, renal failure is suspected. When the hepatobiliary system reacts, the activity of liver enzymes increases.
It is necessary to conduct a differential diagnosis of cardiogenic shock and vasovagal syncope, dissecting aortic aneurysm . With syncope, there are no specific characteristic changes on the ECG; the patient has a history of psychological stress or pain. With aortic dissection, pain is noted along the spinal column and persists for several days, and can be wavy in nature.
Stages of LVN
Pathological processes can also be classified according to severity. Based on this criterion, they call 4 stages, sometimes three.
First
Easy. Does not produce clinically significant symptoms. Organic defects are already present, but not yet critical. The likely manifestation of left ventricular failure at this stage is shortness of breath.
Tachycardia and increased heart rate may develop. Restoration is carried out after identification.
This is the best time to begin treatment for left ventricular failure. Rarely gives attacks. The prognosis is favorable.
Second
Can be divided into two phases.
- A. Pronounced organic changes. The clinical picture is quite clear. Left ventricular heart failure is accompanied by intense chest pain and shortness of breath with moderate physical exertion.
The patient can still perform daily activities, but mechanical work is no longer possible. There is a nonproductive cough and swelling of the lower extremities.
- B Complemented by right ventricular failure. Severe shortness of breath develops after minor physical activity, stable arrhythmia. Pressing pain in the chest. Cough.
The heart is unable to function normally, like other organs. Treatment of such a pathology is futile. The effectiveness is minimal; it is possible to partially alleviate the condition, but complete recovery cannot be achieved.
Third or terminal
Accompanied by total dysfunction of the entire body. There is no strength not only to work, but also to take care of oneself in everyday life, even to move. The patient lies down most of the time, death occurs within a few weeks or months.
Effective treatment is possible only at the first stage. This classification is used to quickly assess the patient’s health status and recovery prospects.
Examination and treatment
Heart failure (HF) is a symptom complex of various manifestations associated with decompensated work of the heart muscle.
In some patients it is combined with pathologies of the pumping function of the heart, while in others there is a disorder in the normal process of filling and emptying the chambers. The disease can be independent or be a complication of a number of serious pathological conditions - from anemia to congenital and acquired heart defects. For diagnosis, various research methods are used aimed at assessing the functions of the left ventricle and the entire cardiovascular system as a whole. After diagnosis, it is extremely important to undergo the treatment recommended by the doctor, since self-medication in such a case is clearly impossible.
Make an appointment with a specialist, without queues, at a convenient time
+7
Sign up
Causes
The development of left ventricular failure is caused by cardiac events. Possible diseases include:
Mitral valve defects
MV stenosis or MV prolapse. Developmental defects in one word. The anatomical structure covers the entrance to the left ventricle, preventing blood from returning to the atrium.
As a result of loose closure of the valves, regurgitation occurs - a reverse flow of liquid tissue. Hence the overload, impaired contractility and dilatation changes. Treatment is surgical, according to indications.
Attention:
At the first symptoms of LVN, the need for surgery is unconditional. Urgent therapy. The prospects for recovery depend on existing anatomical disorders. They are irreversible.
Aortic valve defects
Causes the onset of left ventricular failure even more often. The essence is approximately the same. A pathological narrowing of the valve of the body's largest artery occurs.
The blood comes back into the chamber, the volume of ejection into the large circle is insufficient. Hence the functional and then organic deviations.
Treatment is surgical. If possible, valve repair is performed. If ineffective or inappropriate, prosthetics are indicated.
The prognosis at an early stage is good. Maintenance therapy is required, but the dangers as such are minimal. Read more about aortic valve stenosis in this article.
Arterial hypertension
Patients with a stable increase in pressure suffer from LVH almost three times more often. Why are the statistics so unfavorable?
We are talking about an organic disorder of cardiac structures. During a prolonged increase in tonometer readings, the load on the left ventricle increases.
Myocardial muscle mass increases, but chamber volume and functionality decrease. Hence the decrease in blood output into the aorta.
The process moves further along the chain. A persistent disruption of the functioning of cardiac structures occurs. As the myopathy progresses, it worsens.
The disease develops relatively slowly, and severe left ventricular failure occurs several years later. Therefore, there is time for diagnosis and treatment.
Myocarditis
Inflammation of the muscle layer of the heart. The condition is provoked by an autoimmune or, more often, an infectious factor.
Outside of quality care, preferably in a hospital setting, the likelihood of tissue destruction and death is maximum. The outcome is disability.
Prosthetics may be a treatment option, but will not guarantee complete recovery.
Throughout the entire period of supervision, constant monitoring of the condition is required. Therefore, they try not to keep such patients at home. The risks of sudden death from cardiac arrest or other complications are too great.
Previous myocardial infarction
Acute malnutrition of the muscle layer. Even if the patient is lucky and survives, no one guarantees a favorable outcome in the future. It is necessary to evaluate the extent of the lesion, general health, and the quality of treatment.
In 100% of cases, a heart attack leaves scars; this is post-infarction cardiosclerosis. Hence the guaranteed failure, coronary artery disease, of varying severity.
Lifelong maintenance therapy under the supervision of a specialist is required. Complex cases are difficult to resolve.
Cardiomyopathy
The growth of the muscle layer of the organ (hypertrophic cardiomyopathy), or its stretching - dilatation.
These defects are almost impossible to radically correct. They often turn out to be the result of intoxication, viral and bacterial pathologies, and other processes.
With the help of medications, you can slow down the development of the condition, even to a complete stop. The prognosis in this case is much better.
Congenital and acquired heart defects
Genetic or spontaneously arising during life or intrauterine development. Treatment methods vary and depend on many factors.
The causes of the pathological process are excluded one by one. If defects and functional abnormalities are identified, urgent treatment is indicated. Delay reduces your chances of survival.
Acute left ventricular failure
Acute left ventricular failure is a serious condition caused by decompensation of heart pathology and requiring emergency medical care. In the structure of mortality of cardiac patients, this disease is the first cause of death. What are the main causes, symptoms, diagnostic methods, how is left ventricular failure treated - information about this is further in the article.
Risk factors
Acute cardiac left ventricular failure occurs as a result of complex pathogenetic mechanisms causing primary hypertension (increased pressure) in the pulmonary circulation. Risk factors for decompensation of severe cardiac pathology are physical or emotional stress, fluid overload of the vascular bed, infections, etc.
The development of heart failure is associated with impaired systolic or diastolic function, which is caused by various reasons. In order to understand the pathogenetic mechanism, one should recall some aspects of the anatomical and functional features of the heart.
The heart is a muscular “pump” that continuously pumps blood through 2 circles of blood circulation – large and small. Acute left ventricular failure occurs when there is difficulty in the functioning of the left sections (atrium and ventricle) of the heart and is caused by overload of the pulmonary circulation (PB).
8
24/7
In a simplified manner, the ICC diagram can be described by the following sequential stages of blood circulation through the cardiovascular system:
- Right ventricle.
- Pulmonary trunk.
- Right and left pulmonary arteries.
- Arteries, arterioles, capillaries of the bronchopulmonary system.
- Venules and veins.
- Left atrium.
Oxygen-enriched blood through the mitral valve, during diastole, enters the left ventricle, and from there in systole, it is pushed into the aorta.
Acute left ventricular failure develops under the influence of such unfavorable factors as:
- cardiac ischemia;
- long-term surgical intervention;
- infections;
- hypertonic disease;
- excess fluid in the body;
- bronchial asthma;
- severe kidney disease;
- taking certain medications;
- congenital and acquired pathology of the valve system;
- diseases of the endocrine system.
Under the adverse influence, backflow occurs, overflow and volume overload of the left atrium and pulmonary vascular bed. This causes swelling of the intercellular spaces, reactive narrowing of the bronchial lumen, and foaming of the protein contents of the alveoli. All this leads to the development of a clinical picture of cardiac asthma and pulmonary edema.
Causes
The causes of acute left ventricular failure are cardiac (heart) and non-cardiac in nature. The reasons causing the development of this pathology include:
- chronic heart failure in the decompensation phase;
- myocardial infarction;
- aortic dissection;
- cardiac tamponade;
- infection of arteries and valves;
- severe acute myocarditis;
- arrhythmia attack;
- hypertensive crisis.
Factors that do not affect the anatomical structures of the heart, but significantly affect its work with the development of failure, include:
- violation of treatment tactics (overdose of drugs, non-compliance with the rhythm and frequency of taking medications);
- fluid overload (especially with intravenous infusions);
- alcohol abuse;
- tumor of the adrenal cortex (pheochromocytoma);
- renal failure;
- severe lung pathology (bronchial asthma, COPD, pneumonia, tuberculosis);
- stroke;
- sepsis.
In addition, conditions such as severe anemia and thyrotoxic crisis cause increased cardiac output syndrome, which also negatively affects the condition of the left ventricle.
8
24/7
What happens
Acute left ventricular failure, according to the etiological factor or origin, can be primary and an exacerbation of chronic failure. Primary heart failure is caused by:
- acute nephritis (inflammation of kidney tissue);
- acute myocardial infarction;
- hypertensive crisis.
And among the acute manifestations of chronic left ventricular failure are:
- mitral heart defects;
- defects of aortic origin;
- blood stagnation in the ICC in chronic heart failure;
- left ventricular aneurysm.
According to the clinical course, according to the new recommendations of the Society of Cardiology, heart failure (HF) can be:
- acute decompensated (newly occurring, exacerbation of chronic HF);
- hypertensive – symptoms of heart failure are combined with arterial hypertension;
- pulmonary edema;
- cardiogenic shock;
- HF combined with high cardiac output (more often with infections).
When taking into account the clinical course together with radiographic data, acute HF is divided into 4 degrees of severity:
- There are no clinical signs of heart failure.
- The appearance of symptoms and radiological signs consistent with cardiac asthma.
- Detailed picture of pulmonary edema.
- Cardiogenic shock with a drop in blood pressure.
Based on systematic observation of the clinical course, depending on the volume of blood ejected by the left ventricle, left ventricular HF with high or low cardiac output is distinguished.
Symptoms
At the moment when acute left ventricular failure develops, assistance should be provided according to the clinical variant, each of which has its own characteristics.
Precursors and acute forms of left ventricular failure manifest themselves in the form of:
- increased or onset of shortness of breath;
- forced body position (orthopnea), which alleviates the condition;
- rawness behind the sternum during physical activity;
- cough when changing body position;
- the appearance of wheezing in the lower parts of the lungs.
With stagnation in the pulmonary vessels and their increased tension, fluid leaks from the bloodstream into the intercellular tissue (interstitium). It is interstitial pulmonary edema that underlies the development of cardiac asthma, which has the following clinical manifestations:
- nocturnal asthma attack;
- shortness of breath accompanied by chest pain;
- orthopnea;
- participation of auxiliary muscles in breathing;
- sticky, cold sweat on the face and chest;
- cyanosis (blue discoloration) of the nasolabial triangle, lips, neck, fingertips;
- dry and moist wheezing in the lungs;
- pulse is rapid and arrhythmic.
If help is not provided or treatment is ineffective, the following type of manifestation of left ventricular failure develops - pulmonary edema, which is characterized by symptoms such as:
- suddenness of occurrence;
- bubbling breathing;
- feeling of fear of death;
- moist rales heard at a distance;
- discharge of white-pink frothy sputum;
- Moist rales are heard over all the lungs.
If acute left ventricular failure develops, pulmonary edema must be stopped immediately, since severe respiratory failure leads to acute oxygen starvation of the entire body. This is a critical condition that leads to death in a short time.
8
24/7
Diagnostics
The basis of diagnostic measures aimed at confirming the diagnosis is the collection of objective data, especially auscultatory data (when listening to the lungs with a stethoscope).
The following additional laboratory and instrumental methods are used:
- electrocardiography;
- chest x-ray;
- ECHO-cardioscopy with Dopplerography;
- blood chemistry;
- study of blood gas composition;
- general blood and urine tests;
- study of the coagulation system and D-dimer.
When recording an ECG, a number of characteristic changes are revealed that confirm decompensation of the pathological condition. On the cardiogram, changes in the isoline are recorded in the leads corresponding to the damage.
X-ray allows you to assess the presence and extent of damage to the lung tissue, displacement of the cardiac border, enlargement or displacement of the borders of the heart and mediastinum.
ECHO cardioscopy is performed using an ultrasound sensor with the function of measuring the speed and volume of blood flow through the vessels (Doppler). This study helps to visualize the site of damage, the valve apparatus, measure the volumes of the heart chambers, the thickness of the heart walls, the speed and magnitude of blood flow, and ejection fractions.
A biochemical blood test involves the identification and quantitative assessment of substances that are markers of acute cardiac pathology. Among the biochemical indicators, total protein, ALT and AST, creatine phosphokinase, haptoglobin, creatinine, potassium, sodium, urea, and sugar are taken into account.
Blood gases allow you to determine the degree of decrease in oxygen in the blood and increase in carbon dioxide. The criteria for these indicators reflect the severity of hypoxia – oxygen starvation and help monitor the patient’s condition and the effectiveness of therapeutic measures.
Treatment at different stages
If acute left ventricular failure develops, emergency care should be provided even before the ambulance arrives. The algorithm of actions is as follows:
- Call an ambulance.
- Position the patient in a semi-sitting position.
- Provide access to fresh air.
- Unbutton your shirt collar and loosen your belt.
- If possible, calm down, give Valoserdin, Valocardin, Corvalol to drink.
- Measure and record blood pressure and pulse, do this every 10 minutes.
- When systolic (upper) pressure is above 100 mm Hg. suggest dissolving a Nitroglycerin tablet under the tongue.
- Apply tourniquets to the thighs (15-20 cm below the inguinal fold), loosen them every 15 minutes.
- If you lose consciousness, place yourself in a safe position on your side.
- Clear your mouth of foam.
- If there is no breathing or heartbeat, begin chest compressions and artificial respiration.
Acute left ventricular failure, the treatment of which must be carried out in an intensive care unit or resuscitation room, is an absolute indication for hospitalization in a cardiological or therapeutic hospital.
Therapeutic measures aimed at relieving this pathological condition include methods such as:
- oxygen therapy - inhalation of heated, humidified oxygen through a mask or nasal cannulas, for pulmonary edema, passed through an antifoam agent - ethyl alcohol;
- administration of narcotic analgesics (Morphine), which provide a sedative (calming) and analgesic effect;
- intravenous administration of Nitroglycerin;
- use of diuretics (Lasix, Furosemide, Ethacrynic acid);
- prescription of cardiac glycosides (Strophanthin, Korglykon, Digoxin);
- cardioversion – used for atrial flutter or fibrillation.
For successful treatment of acute HF caused by non-cardiac pathology, it is important to establish and eliminate the cause that causes it. With continued exposure to a negative factor, therapeutic measures turn out to be ineffective, which leads to rapid death.
Forecast
The prognosis for this disease is rarely favorable, and despite the achievements of modern resuscitation, pulmonary edema is very often the cause of death. The forecast largely depends on the following factors:
- etiology of the development of heart failure (acutely occurring or decompensation of chronic heart failure);
- the extent of damage to the cardiac structure due to cardiogenic causes;
- possibilities for rapid relief of non-cardiac causes of heart failure (pneumonia, sepsis, thyrotoxic crisis);
- age;
- the presence of concomitant pathology.
Left ventricular failure, which occurs as a transient condition, has a more favorable prognosis, which depends on the volume and timeliness of medical intervention. Often acute heart failure is accompanied by massive damage to the heart and becomes chronic.
Disease prevention
The basis for preventing the development of acute left ventricular failure is a commitment to strict adherence to doctor’s prescriptions. It is important to exclude all provoking factors that contribute to damage to the cardiovascular system.
Measures to prevent heart disease include the following:
- to give up smoking;
- avoiding the consumption of alcoholic beverages;
- compliance with diet therapy (limiting cholesterol-rich foods, fatty, fried, canned foods, coffee, confectionery, animal fats);
- performing feasible physical exercises daily (jogging, yoga, Nordic walking, swimming);
- exclusion of stressful situations and neuro-emotional experiences;
- limiting physical overexertion.
8
24/7
Acute left ventricular failure is based on cardiac and non-cardiac causes, which cause hypertension in the pulmonary circulation. The main manifestations of the pathology are cardiac asthma and its complication – pulmonary edema. Timely provision of emergency and specialized care for acute heart failure affects the prognosis of the disease.
Symptoms
Signs of left ventricular failure appear from the very first stages of the pathological process.
However, at the initial stages they are nonspecific, and they are almost impossible to detect. In most cases, detection of changes is accidental.
An approximate list of manifestations, without reference to stage:
- Chest pain. They have a burning or pressing character, which directly indicates organ ischemia. The duration is minimal, from 2 to 30 minutes. The occurrence of such a symptom is not necessary.
- Dyspnea. Classic manifestation. Indicates the beginning of problems with gas exchange. At the first stage, the defect after which the symptom develops is high, so the common person does not notice changes in well-being. At stages 2-3, the intensity of the symptom is so great that the patient is unable to move normally, work, or even take care of himself at home.
- Dry non-productive cough. Against the background of developing respiratory failure.
- Impaired consciousness as a result of a decrease in the intensity of blood circulation in the brain.
- Edema of the lower extremities.
- Pale skin.
- Cyanosis of the nasolabial triangle.
- Periodic panic attacks.
Symptoms of left ventricular failure are cardiac, respiratory and neurogenic. The more developed the pathological process, the more significant the clinical picture.
Main symptoms of the disease
Depending on the location of the affected area and the direction of blood flow, acute heart failure can be:
- left ventricular;
- right ventricular
Left ventricular AHF can manifest itself as a result of: hypertensive crisis, myocardial overload due to cerebrovascular accidents, interruptions in cardiac function. Symptoms of left ventricular AHF:
- dry cough, which produces foamy sputum;
- difficult, noisy and frequent breathing (more than 24/min.);
- shortness of breath and cough in a horizontal position, which is why the patient can only sleep reclining;
- shortness of breath, sometimes reaching the level of suffocation;
- increased sweating (hyperhidrosis);
- heart rhythm disturbance;
- excitement, fear of death;
- bluish or pale skin.
With exacerbation of heart failure in the lower parts of the lungs, fine rales can be heard. With the development of AHF, the patient's bronchi swell and cause prolonged exhalation due to impaired air flow. The patient's breathing becomes bubbling, there is a murmur in the upper part of the heart, pulmonary edema and expansion of the myocardial boundaries to the left are possible.
Right ventricular AHF can be caused by: infarction, pericardial tamponade, or pulmonary thromboembolism. With this pathology, venous stagnation of blood circulation in the systemic circle is observed. Symptoms of right ventricular AHF:
- swelling of the internal jugular veins in the patient’s neck;
- bluish tint on the tip of the nose, fingers and ears;
- noticeable enlargement of the liver and dull pain in the right hypochondrium, which intensifies with palpation;
- myocardial expansion to the right;
- sticky cold sweat and chest pain;
- a change in heart rhythm, in which a thread-like pulse is barely palpable;
- accumulation of fluid in the peritoneum, swelling of the legs;
- arterial hypotension, in which blood pressure is below normal.
The medical doctor offers to make an appointment with a cardiologist. A full range of diagnostics and treatment of heart diseases in Tula. Tel. for appointment +7 (4872) 39-30-33.
First aid for an attack
There is little you can do on your own. The goal is to stabilize the patient's condition. There is no chance of elimination without special intervention. The main thing to do is to call a team of doctors.
Before the ambulance arrives, the emergency algorithm is as follows:
- Sit the patient down and place a cushion made from available materials under his back. A blanket or clothing will do.
- Be sure to lower your arms and legs. There should be no intense peripheral circulation, as this will negatively affect the state of the cardiovascular system.
- Open a vent or window to provide fresh air into the room.
- Against the background of pain, give a Nitroglycerin tablet. One.
- Measure blood pressure.
- If symptoms of cardiogenic shock develop (loss of consciousness, indifference to what is happening, a sharp drop in blood pressure and heart rate), the patient must be taken to the hospital as quickly as possible. If possible, it is better to do this on your own, without waiting for an ambulance.
Make an appointment with a cardiologist
The best cardiologists at the private Multidisciplinary Medical Center in Moscow invite patients with any type of cardiac dysfunction to diagnose and treat them. If signs of heart failure are detected, the patient is prescribed a comprehensive examination, after which experienced specialists will monitor the disease through medication and other effective therapy.
You can make an appointment with a cardiologist for a fee by phone or using the feedback form. Check the price of initial and repeat appointments on the clinic’s website. If the patient’s condition is acute, cardiologists will see him without an appointment at any time of arrival at our center.
Moscow, st. Krasnodarskaya, house. 52, bldg. 2
+7
We work on weekdays and weekends from 8.00 to 21.00
Diagnostics
The examination is carried out under the supervision of a cardiologist. An acute attack requires immediate action. Therefore, specialized actions are taken immediately, and then the results of instrumental methods are evaluated.
After restoration of basic vital signs, the following examination methods are indicated:
- Oral interview with a person. Complaints play a big role.
- Anamnesis collection.
- Measurement of blood pressure, heart rate.
- Auscultation. Listening to sound. Against the background of current defects, systolic murmur develops. The tones are dull, chaotic behavior is possible due to arrhythmias.
- Electrocardiography. Assessment of the functional state of the heart. Depression of the ST segment and deformation of the R, P, and S teeth occur.
- Echocardiography. Used to detect organic defects. Deviations are clearly visible during imaging.
- MRI or CT if indicated.
- Scintigraphy.
- Coronography.
This is enough in the system. It is possible to prescribe 24-hour monitoring to determine heart rate and blood pressure over a 24-hour period.
The examination takes place in an inpatient or outpatient setting. The first option is faster.
Diagnosis of heart failure
When diagnosing a disease, it is extremely important to identify the true cause of its development - only then can treatment be as successful as possible.
After collecting an anamnesis and physical examination, a cardiologist may prescribe:
- general clinical, biochemical blood and urine tests;
- electrocardiography (at rest);
- Ultrasound of the heart (Echocardiography);
- chest x-ray;
- coronary angiography;
- Holter ECG monitoring and other studies.
Treatment
{banner_banstat9}
Urgent. The directions of influence are as follows: elimination of the root cause of the condition, removal of threatening symptoms, prevention of complications. All three problems are solved simultaneously, but in different ways.
Etiotropic therapy requires surgical intervention in most cases. Mitral and aortic valve replacement, stenting or ballooning (dilation of the affected vessel).
For myocarditis, immunosuppressants (autoimmune type) or antibiotics, antivirals, fungicides under the guise of cardioprotectors are indicated.
Symptomatic effects require the use of antiarrhythmic, organic nitrates, and sedatives.
Additionally, glycosides (Digoxin, tincture of lily of the valley), beta blockers (Anaprilin, Carvedilol), and diuretics to evacuate excess fluid (Veroshpiron) are prescribed. It is also possible to prescribe ACE inhibitors (Perindopril in different variations).
Prevention is carried out using the same pharmaceutical agents in small dosages.
Additionally, lifestyle changes are indicated. Refusal of smoking, alcohol, drugs, fatty foods, salt intake in the amount of 7 grams per day. Fortification of the diet, refusal of significant physical activity. The recommendations are strict, you cannot deviate from them if you want to be cured.
LVAD is such a complex and complex process that there is no and cannot be an unambiguous answer about the treatment regimen.
Forecast
{banner_banstat10}
Left ventricular failure causes death in 70% of cases. The outcome directly depends on many factors:
- General health.
- Presence of somatic pathologies.
- Working blood pressure level.
- Family history.
- Time course of pulmonary hypertension and other diseases.
- The quality of the treatment provided.
- Age.
- Floor.
- Body type, weight, overweight and obesity.
- Nature of nutrition.
- Bad habits, lifestyle.
- Emotional condition.
- Hormonal background.
- Type of professional activity.
In combination, these factors give a unique, unique picture. Accordingly, the forecast depends on the mass of moments.
To roughly formalize the numbers: the probability of survival at the first stage is 95% with proper treatment. The process is stopped completely.
Starting from the second, the values decrease proportionally:
| Stage | Survival percentage |
| 2A | 75% |
| 2B | 30% |
| 3 | 5% |
Possible complications
Among the likely consequences of a long-term or, especially, acute course of the pathological process, the following are distinguished:
- Cardiogenic shock. Emergency condition. Accompanied by a critical drop in blood pressure and heart rate. Contractility is insufficient, blood ejection into the systemic circle is also insufficient. Hence the generalized dysfunction of the whole body.
- Cardiac arrest and sudden death without prospects for resuscitation.
- Heart attack. Acute myocardial malnutrition, necrosis of active muscle tissue (read about the first signs of pre-infarction here).
- Stroke. Similar phenomenon. Its essence lies in the death of nerve cells and the development of persistent neurological deficits. What nature depends on the localization. Disability often occurs.
- Pulmonary edema. As a result of insufficient gas exchange. May lead to death from asphyxia. Restoration is urgent.
- Attack of cardiac asthma.
- Vascular dementia due to damage to the arteries of the brain.
All of these conditions are potentially fatal. Treatment is immediate, in a specialized hospital. The risks are great, so first aid must also be provided. The outcome depends on the quality of the event.
Causes of AHF
Automaticity of the heart - the ability to contract rhythmically can decrease due to heavy loads. Acute heart failure can manifest itself when the elasticity of the myocardial walls decreases due to inflammation caused by pathogenic bacteria and infections entering the patient’s blood after a viral disease (sore throat, meningitis, pneumonia, etc.). AHF can also be caused by diseases associated with impaired myocardial function.
In most cases, the patient's heart cannot eject the required volume of blood or accept the required amount into the ventricles. The main causes of acute heart failure:
- Diseases that reduce the contractile activity of the heart muscle: heart attack, myocarditis, surgery using an artificial respiration system.
- Weakening of the function of the heart muscle caused by impaired coronary circulation.
- Cardiac tamponade. Accumulation of fluid in the pericardial cavity, which leads to irregular contractions of the heart due to compression of the cavities.
- Hypertensive disease (hypertension), in which blood pressure rises above normal.
- Functional and morphological changes in the structure of heart valves and myocardium.
- Arterial hypertension, expressed as increased pressure in the system.
- Arrhythmia is a pathological condition that is accompanied by a violation of the heart rate, a change in the sequence and rhythm of heart contractions.
The following factors can also cause heart failure: focal brain damage due to stroke, electrical injury, brain injury, drug poisoning or ethyl alcohol intoxication.