Legionellosis ranges in severity from a mild febrile illness to a serious and sometimes fatal form of pneumonia and is caused by exposure to a variety of Legionella bacteria that is found in water and soil mixtures.
Cases of Legionnaires' disease are often classified based on the type of exposure (community-acquired, travel-acquired, or hospital-acquired).
The most common cause of illness, including outbreaks, is the bacterium Legionella pneumophila. Legionella pneumophila and related species are commonly found in lakes, rivers, streams, hot springs, and other bodies of water. Other species, including L. longbeachae, can be found in potting mixes.
The bacterium L. pneumophila was first identified in 1977. It was the cause of an outbreak of severe pneumonia at a convention center in the United States in 1976. It has since been associated with outbreaks associated with poor maintenance of man-made water systems, particularly in cooling towers and evaporative condensers used in air conditioning and industrial refrigeration systems, hot and cold water systems in public and private buildings, and in hot tubs. .
The dose of infection is unknown, but in susceptible individuals it can be assumed to be low because symptoms appear after short exposure and at distances of 3 km or more from the source of outbreaks. The likelihood of disease depends on the concentration of Legionella in the water source, the production and spread of aerosols, characteristics of the infected person such as age and pre-existing health status, and the virulence of the particular strain of Legionella. In most cases of infection, the disease does not manifest itself.
Cause
The causative factors are Legionella bacteria found in water or soil mixtures. The most common cause of the disease is the freshwater species L. pneumophila, which is found in natural aquatic environments throughout the world. However, the most likely source of the disease is artificial water systems, which create conditions conducive to the growth and spread of Legionella.
These bacteria live and multiply in water systems at temperatures of 20-50 degrees Celsius (optimal temperature is 35 degrees Celsius). Legionella can survive and reproduce as parasites in single-celled protozoans and biofilms that form in aquatic systems. They can cause infection by infecting human cells, a mechanism similar to that of protozoan infections.
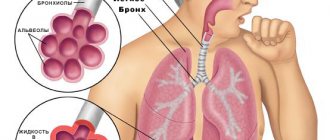
The mechanism of the onset and development of the disease
In water, Legionella bacteria grow and reproduce in amoebas and ciliated protozoa, which are small single-celled organisms. In addition to providing nutrients for Legionella to reproduce and grow, protozoa also act as a refuge that protects Legionella from adverse environmental conditions such as extreme temperatures and chemicals such as bleach or bleach.
Human immune cells called alveolar macrophages are very similar to protozoa. Once in human lungs, the Legionella bacterium invades alveolar macrophages and grows in them, mistaking them for a natural host, this leads to the development of Legionnaires' disease and other diseases in humans.
Broadcast
The most common form of transmission of Legionella is through inhalation of contaminated aerosols. Sources of aerosols that have been associated with transmission of Legionella include air conditioning cooling towers, hot and cold water systems, humidifiers, and hot tubs. Infection—especially among vulnerable hospital patients—can also occur through aspiration of contaminated water and ice, and when newborn babies are exposed to the bacterium during water births. The infection is not transmitted directly from person to person.
A little about legionnaires
Where does such a strange name come from?
The fact is that the history of Legionnaires' disease began on July 21, 1976, when the American Legion, an organization of military veterans, had the misfortune of opening its annual three-day convention at the Bellevue-Stratford Hotel (Pennsylvania), equipped with the latest climate control systems. Just three days after the conference, a series of mysterious deaths began. Over the next few days, out of 2,000 participants at the convention, more than 150 people were hospitalized. The outbreak killed 29 veterans. The search for the reasons that led to the epidemic took six months. In January 1977, the source of legionellosis infection was identified - a bacterium whose name - Legionella - forever imprinted the image of the first people to become ill - legionnaires. Some experts believe that Legionella began its destructive activity much earlier. Presumably, they could be responsible for outbreaks of pneumonia in the United States even before 1976. Nevertheless, a massive “attack” of bacteria began simultaneously with the creation of household appliances and systems in which there is a possibility of stagnation of warm water.
Legionella pneumophila, which received an excellent opportunity to live and develop in the moist and comfortable microenvironment of swimming pools, internal water supply systems, showers, refrigerators, Jacuzzis, fountains, modern dental equipment, car windshield washers and, of course, air conditioning systems, continues to be the cause of 2 –15% of all cases of community-acquired pneumonia in the world requiring hospitalization [1].
Incidence rate
The prevalence of known cases of Legionnaires' disease varies widely depending on the level of surveillance and reporting. Since many countries do not have adequate diagnostic methods for this infection or sufficiently developed surveillance systems, incidence rates are unknown. In Europe, Australia and the USA, there are about 10-15 cases per year per million inhabitants.
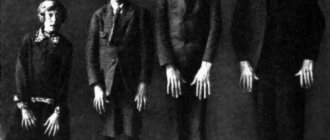
It is reported that 75-80% of patients are over the age of 50 years and 60-70% of them are men. Other risk factors for community-acquired legionellosis not associated with travel include: smoking, binge drinking, lung disease, impaired immunity and chronic respiratory or kidney disease.
Risk factors for hospital-acquired pneumonia include the following: recent surgery, intubation, which is the process of inserting a tube into the windpipe, mechanical ventilation, suction, presence of nasogastric tubes, and use of respiratory therapy equipment. The most susceptible subjects are patients with compromised immune systems, including organ transplant and cancer patients, and patients taking corticosteroids.
Prognostic factors for death due to Legionnaires' disease are late diagnosis and late initiation of appropriate treatment with antibiotics, advanced age and the presence of concomitant diseases.
Diagnosis of legionellosis
Once admitted to hospital, patients can expect to undergo a series of special tests, including a sample culture test on a medium designed specifically for Legionella bacteria. The environment allows bacteria to grow faster so doctors can observe and identify them.
Other common tests for Legionnaires' disease include an antibody test, a blood test that shows the presence of antibodies that fight Legionella bacteria; a urinary antigen test, which helps detect bacteria in urine; and direct tests for fluorescent antibodies (immunofluorescence assay (IFA)), during which the bacteria are stained and made visible under a special fluorescent microscope.
Symptoms
Legionellosis is a general term that describes pulmonary and non-pulmonary forms of Legionella infection.
The nonpulmonary form (Pontiac disease) is an acute, self-limiting influenza-like illness that usually lasts 2 to 5 days. The incubation period ranges from several hours to 48 hours. Main symptoms: fever, chills, headache, malaise and muscle pain (myalgia). This type of infection is not fatal.
The incubation period for the pulmonary form of Legionnaires' disease ranges from 2 to 10 days (however, in a number of outbreaks that have occurred, it has been up to 16 days). Symptoms initially include fever, loss of appetite, headache, malaise and lethargy. Some patients may experience muscle pain, diarrhea, and confusion. A mild cough is also common, but up to 50% of patients may produce sputum. Bloody sputum or hemoptysis may occur in approximately one third of patients. The severity of this illness ranges from a mild cough to a rapidly fatal pneumonia. Death occurs as a result of progressive pneumonia with respiratory distress and/or arrest and multiple organ failure.
If Legionnaires' disease is left untreated, it usually gets worse within the first week. Like other risk factors for severe pneumonia, the most common complications of Legionnaires' disease are pulmonary failure, shock, and acute kidney and other organ failure. Restoration of function in all cases requires treatment with antibiotics and usually takes several weeks or months. In rare cases, severe progressive pneumonia or ineffective treatment of pneumonia can cause complications in the brain.
Mortality rates from Legionnaires' disease depend on the severity of the disease, the adequacy of initial antimicrobial treatment, the site of Legionella infection, and the characteristics of the patient (meaning that the disease tends to be more severe in immunocompromised patients). The mortality rate can be as high as 40-80% in patients who are not treated for immunocompromised conditions, and can be reduced to 5-30% through appropriate management and depending on the severity of clinical indications and symptoms. Overall, the mortality rate is usually 5–10%.
Treatment of Legionnaires' disease
Legionnaires' disease is treated with antibiotics as Azithromycin , Ciprofloxacin and Levofloxacin . Many cases of Legionnaires' disease can be successfully treated, but even healthy people usually require hospitalization. It is important to note that early detection and diagnosis can increase the likelihood of treatment success for Legionnaires' disease, shorten recovery time, and help prevent serious, long-term complications.
If you (or a loved one) begin to exhibit signs and symptoms of Legionnaires' disease while at a public pool or water park, staying at a hotel, on a cruise ship, or living in a large apartment building, seek medical attention immediately.
About 1 in every 10 people who get Legionnaires' disease will die due to complications caused by their disease. Even those who contract Legionnaires' disease while in a health care facility (about 1 in every 4) will die.
How does the disease develop?
Legionella enters the human body through the respiratory tract. The pathogen is fixed in different parts of the respiratory system (including in the lung tissue). The depth of its penetration depends on the size of aerosol infected particles, their dose and breathing patterns. Microorganisms can also enter the human body along with protozoa infected by them and during certain surgical and other medical procedures. It is possible that they will be introduced into the body along with contaminated drinking water.
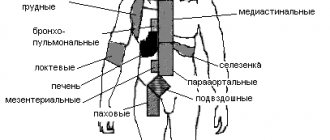
Through the bloodstream, the pathogen can enter various systems and organs. The lungs, liver, kidneys, nerve tissues and bone marrow are most often affected. With a high level of Legionella in the blood, the disease can develop as a septic type and be accompanied by the appearance of secondary purulent foci or septic endocarditis.
Prevention and recommendations
Legionnaires' disease is a life-threatening disease that can be contracted from a number of sources. Fortunately, many cases, especially if identified and diagnosed early, can be successfully treated with professional medical care and antibiotics .
The easiest way to protect yourself is to keep your lungs (respiratory system) healthy, do not smoke, wear a protective mask if you work with large water supply systems, and wash it with bleach every time you take a bath.
Legionella pneumonia: treatment
The pathogens in Legionella pneumonia are located inside cells, so to treat inflammation, drugs are used that can accumulate in the cell in high concentrations. Macrolides, fluoroquinolones and tetracyclines are used in therapy. The drug of choice is erythromycin. At the beginning of therapy, the antibacterial agent is administered intravenously or intramuscularly to obtain the best effect. In the future, they switch to using drugs orally. The course of antibiotic therapy is from 7 days. The full duration of treatment is determined by the attending physician, taking into account the dynamics of therapy. On average, therapy can take several weeks. You cannot stop taking antibiotics on your own until complete recovery, which must be confirmed by tests. Otherwise, pneumonia will not be completely cured, and a relapse of the acute condition is possible. In addition, with the uncontrolled use of antibiotics, bacteria become unstable to this type of drug.
Treatment of legionella pneumonia is recommended to be performed in a hospital. The patient should be under the supervision of a physician to monitor the condition and adjust therapy if necessary. The Yusupov Hospital offers its patients comfortable rooms that are equipped with everything necessary for a comfortable stay. Patients are provided with round-the-clock qualified medical care. Patients' meals are prepared by a nutritionist based on the therapist's recommendations and the patient's individual preferences. There is a picturesque park on the hospital grounds where patients can walk and breathe fresh air (after permission from the attending physician).
At the Yusupov Hospital, therapists use effective methods of evidence-based medicine to treat pneumonia, the effectiveness of which has been confirmed by research and personal practice, which allows us to obtain the best results. You can make an appointment with a therapist or pulmonologist, or get specialist advice by phone.