Ranexa - a new milestone in the treatment of stable angina
As an advertisement
Modern medicine offers a wide range of drugs used to treat coronary heart disease, including both drug therapy and invasive treatment methods. But, despite all the advances in medicine, a significant proportion of patients suffering from coronary heart disease continue to experience symptoms of angina pectoris, which significantly limits their activity and reduces the quality of everyday life.
For these reasons, at the present stage, one of the main tasks in the treatment of patients with stable angina remains to reduce the frequency and intensity of angina attacks in order to improve the patient’s quality of life.
presents a new drug in its cardiology line - Ranexa®. Ranexa® is an innovative treatment for stable angina.
Ranexa® was first registered in the United States in 2006, where it was approved by the Food and Drugs Administration of the United States (FDA) as a drug for the treatment of stable angina. The drug has been on the European market since 2008.
Ranexa® is a new drug for the treatment of stable angina with an innovative mechanism of action that reduces ischemia in patients with stable angina.
The clinical manifestations of stable angina are based on transient myocardial ischemia, which is caused by a discrepancy between the myocardial oxygen demand and its delivery. Under conditions of ischemia, cardiomyocytes are overloaded with calcium ions, which in turn leads to impaired myocardial relaxation during diastole and impaired diastolic filling of the coronary arteries, provoking an attack of angina.
Ranolazine, the active ingredient of the original drug Ranexa®, is a powerful inhibitor of late sodium current. By selectively inhibiting the late sodium current, ranolazine prevents overload of cardiomyocytes with sodium ions, thereby blocking reverse sodium-calcium metabolism and, accordingly, the accumulation of calcium ions in the cell. It helps to improve the mechanical and electrical function of the myocardium by improving diastolic relaxation and coronary blood flow without affecting or independent of hemodynamic parameters. Thanks to this mechanism of action, the drug breaks the vicious circle of ischemia, restoring the balance between oxygen delivery and consumption by the myocardium.
The mechanism of action of ranolazine is unique and fundamentally new, which distinguishes it favorably from other classes of drugs for the treatment of stable angina and suggests the emergence of a new modern class of antianginal drugs.
The high efficacy and safety profile of ranolazine were studied in large multicenter clinical trials (MARISA, CARISA, ROLE, ERICA, MERLIN-TIMI, TERISA), which involved more than 8,000 patients. Ranolazine has an effective antianginal and anti-ischemic effect, has been proven to reduce the frequency of angina attacks and increases exercise tolerance in patients with stable angina.
The drug is included in European and American guidelines for the diagnosis and treatment of stable angina.
Ranexa® is available in two dosages: 500 mg and 100 mg. The recommended starting dose of Ranexa® is 500 mg 2 times a day. After 2–4 weeks, the dose, if necessary, can be increased to 1000 mg 2 times a day. The maximum daily dose is 2000 mg.
The drug can be used both as monotherapy and as part of a combination treatment of stable angina.
Proven clinical efficacy, a well-studied safety profile and excellent tolerability, hemodynamic neutrality, and the possibility of use in patients with concomitant diseases - all this can make it a good addition to the anti-ischemic drugs available in the doctor’s arsenal and take its rightful place among drugs for antianginal therapy.
Ranexa, 60 pcs., 500 mg, extended-release film-coated tablets
Concomitant use is contraindicated
Potent CYP3A4 inhibitors
Ranolazine is a substrate of cytochrome CYP3A4. Concomitant use with inhibitors of CYP3A4 isoenzyme activity increases the concentration of ranolazine in the blood plasma. Potential dose-dependent side effects (eg, nausea, dizziness) may also increase with increasing plasma concentrations of the drug. Simultaneous treatment with ketoconazole 200 mg 2 times a day increases the AUC of ranolazine by 3-3.9 times.
The simultaneous use of ranolazine and potent inhibitors of the CYP3A4 isoenzyme (for example, itraconazole, ketoconazole, voriconazole, posaconazole, HIV protease inhibitors, clarithromycin, telithromycin, nefazodone) is contraindicated.
Grapefruit juice is also a potent inhibitor of the CYP3A4 isoenzyme.
Concomitant use with caution
Medium strength inhibitors of the CYP3A4 isoenzyme
Diltiazem (180-360 mg 1 time / day), an inhibitor of the CYP3A4 isoenzyme of moderate strength, causes, depending on the dose, an increase in the average Css value of ranolazine in blood plasma by 1.5-2.4 times. For patients receiving diltiazem and other moderately potent CYP3A4 inhibitors (e.g., erythromycin, fluconazole), dose titration of ranolazine is recommended. A dose reduction of ranolazine may be necessary.
Inducers of CYP3A4 isoenzyme activity
Concomitant use of ranolazine with inducers of CYP3A4 isoenzyme activity (rifampicin, phenytoin, phenobarbital, carbamazepine, St. John's wort (Hypericum perforatum)) may lead to a decrease in the effectiveness of the drug. For example, rifampicin (600 mg 1 time / day) reduces the Css of ranolazine in blood plasma by approximately 95%. Therefore, the use of ranolazine should not be started in patients receiving treatment with inducers of the CYP3A4 isoenzyme.
P-glycoprotein inhibitors
Ranolazine is a P-glycoprotein (P-gp) substrate. P-gp inhibitors (eg, cyclosporine, verapamil) increase ranolazine plasma concentrations. Verapamil (120 mg 3 times/day) increases the Css of ranolazine by 2.2 times. For patients receiving treatment with P-gp inhibitors, dose titration of ranolazine is recommended. A dose reduction of ranolazine may be necessary. On the other hand, ranolazine is a moderate P-gp inhibitor and a weak CYP3A4 inhibitor and may increase plasma concentrations of P-gp or CYP3A4 substrates. The tissue distribution of drugs that are transported by P-gp may be increased.
Substrates of the CYP2D6 isoenzyme
There is evidence that ranolazine is a weak inhibitor of the CYP2D6 isoenzyme. Taking ranolazine 750 mg 2 times a day increases the concentration of metoprolol in the blood plasma by 1.8 times. Therefore, when used simultaneously with ranolazine, the effect of metoprolol or other substrates of the CYP2D6 isoenzyme (for example, propafenone and flecainide, to a lesser extent, tricyclic antidepressants and antipsychotics) may be enhanced; therefore, a dose reduction of these drugs may be required.
Substrates of the CYP2B6 isoenzyme
The potential to inhibit the CYP2B6 isoenzyme has not been established. Caution is recommended when administered together with substrates of the CYP2B6 isoenzyme (for example, bupropion, efavirenz, cyclophosphamide).
Digoxin
There is evidence of an increase in the concentration of digoxin in the blood plasma by an average of 1.5 times with the simultaneous use of digoxin and ranolazine. Therefore, it is necessary to monitor digoxin levels at the beginning and after the end of ranolazine therapy.
Substars of the CYP3A4 isoenzyme
Ranolazine is a weak CYP3A4 inhibitor, which may result in increased plasma concentrations of CYP3A4 substrates and may require dose adjustment for sensitive CYP3A4 substrates (e.g., simvastatin, lovastatin) and CYP3A4 substrates with a narrow therapeutic index (e.g., cyclosporine, tacrolimus, sirolimus , everolimus).
Simvastatin
The metabolism and clearance of simvastatin is highly dependent on the CYP3A4 isoenzyme. Taking ranolazine 1000 mg 2 times a day increases the concentration of simvastatin lactone, simvastatin acid, which increases the inhibition of HMG-CoA reductase by 1.4-1.6 times. Taking simvastatin in high doses is associated with the development of rhabdomyolysis, and cases of rhabdomyolysis have also been described with the simultaneous use of ranolazine and simvastatin. The maximum dose of simvastatin for patients concomitantly taking ranolazine should not exceed 20 mg/day. For other statins metabolized by the CYP3A4 isoenzyme (lovastatin), dose limitation is possible.
Tacrolimus, cyclosporine, sirolimus, everolimus
An increase in plasma concentrations of tacrolimus, a substrate of the CYP3A4 isoenzyme, was observed in patients receiving ranolazine. When tacrolimus and ranolazine are used concomitantly, it is recommended to monitor the concentration of tacrolimus in the blood plasma and, if necessary, adjust the dose. This approach is also recommended for other CYP3A4 substrates with a narrow therapeutic index (for example, cyclosporine, sirolimus, everolimus).
Drugs that prolong the QT interval
There is a theoretical possibility that with simultaneous use of ranolazine and other drugs that prolong the QT interval, a pharmacodynamic interaction may occur and the risk of developing ventricular arrhythmias may increase. These drugs include certain antihistamines (eg, terfenadine, astemizole, mizolastine), certain antiarrhythmics (eg, quinidine, disopyramide, procainamide), and erythromycin and tricyclic antidepressants (eg, imipramine, doxepin, amitriptyline).
Ranexa®
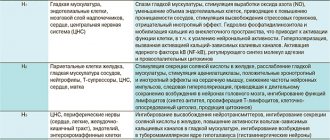
Mechanism of action.
Ranolazine is the active ingredient of Ranexa®. Ranolazine has a complex mechanism of action that is partially established and is based on the ability of ranolazine to inhibit the late sodium ion current in myocardial cells. A decrease in intracellular sodium accumulation leads to a decrease in excess intracellular calcium ions. This reduces the intracellular ion imbalance observed during ischemia. Reducing excess intracellular calcium promotes myocardial relaxation and thus reduces diastolic tension of the ventricular wall. Clinical evidence of inhibition of late sodium current by ranolazine is a significant shortening of the QTc interval (QTc is the corrected value of the QT interval based on heart rate) and a positive effect on diastolic relaxation found in an open study in patients with long QT syndrome ( patients with LQT-3 syndrome who have mutations in the SCN5A AKPQ gene).
These effects of the drug are independent of changes in heart rate, blood pressure (BP), or the degree of vasodilation.
Impact on hemodynamics:
in controlled clinical studies in patients treated with ranolazine as monotherapy or in combination with other antianginal agents, a slight decrease in heart rate (< 2 beats/min.) and a decrease in systolic blood pressure (< 3 mm Hg) were noted.
Effects detected by electrocardiography:
In patients treated with ranolazine, a dose- and plasma concentration-dependent prolongation of the QTc interval (about 6 ms when taking 1000 mg twice daily), a decrease in T wave amplitude, and, in some cases, double-humped T waves were observed.
These electrocardiographic effects result from ranolazine's inhibition of the fast forward potassium current rate, which prolongs the ventricular action potential, as well as the inhibition of the late sodium current, which shortens the ventricular action potential. A population-based analysis of pooled data from 1308 patients with stable angina and healthy volunteers showed that ranolazine resulted in a QTc prolongation from baseline of an average of 2.4 ms at ranolazine plasma concentrations of 1000 ng/mL. In patients with clinically significant liver failure, the degree of QTc prolongation was higher.
The MERLIN-TIMI 36 study, conducted in 6560 patients with ACS (acute coronary syndrome)-unstable angina/NSTEMI (non-ST segment elevation myocardial infarction), did not show a positive effect on outcomes. However, in 3162 patients treated with ranolazine, 7-day Holter ECG monitoring was performed, which resulted in a significantly lower incidence of arrhythmias compared with placebo, including ventricular tachycardia ≥ 8 beats, and in patients treated with ranolazine, no no proarrhythmic effects were recorded.
Clinical efficacy and safety.
Clinical studies have established the effectiveness and safety of ranolazine for the treatment of patients with stable angina, both in monotherapy and in combination therapy with insufficient effectiveness of other antianginal drugs.
The pivotal CAR.ISA trial evaluated ranolazine 750 mg or 1000 mg twice daily or placebo added to standard antianginal therapy with atenolol 50 mg once daily or amlodipine 5 mg once daily in 823 patients over 12 weeks. , or diltiazem 180 mg once daily. Ranolazine was more effective in increasing the duration of physical activity, and there was a significant reduction in the frequency of angina attacks per week and the use of short-acting nitroglycerin compared with placebo. During the entire period of therapy, there was no development of tolerance to ranolazine, and there was no increase in the frequency of angina attacks after abrupt discontinuation of the drug.
Similarly, in the ERICA clinical trial, in which 565 patients were randomized to receive an initial dose of ranolazine 500 mg twice daily or placebo in addition to concomitant amlodipine 10 mg once daily for 1 week, then the dose of ranolazine was increased to 1000 mg twice daily. once a day for 6 weeks. The ranolazine group achieved a significant reduction in the frequency of angina attacks per week (p = 0.028) and short-acting nitroglycerin consumption (p = 0.014) compared with placebo.
The pivotal MARISA study, involving 191 patients, was conducted to determine the optimal dose of ranolazine (500 mg twice daily, 1000 mg twice daily, 1500 mg twice daily) for monotherapy. The study demonstrated that ranolazine was significantly superior to placebo in increasing exercise duration, time to onset of angina, and time to 1 mm ST-segment depression for all three doses, with a dose-dependent effect observed.
The MERLIN-TIMI 36 study found no differences between ranolazine and placebo in the risk of all-cause death, sudden cardiac death, or incidence of documented symptomatic arrhythmias when added to standard drug therapy (including beta blockers, calcium channel blockers). , nitrates, antiplatelet agents, lipid-lowering drugs and ACE inhibitors). Approximately half of the patients in the MERLIN-TIMI 36 study had a history of angina. Results show that exercise duration increased by 31 days in patients treated with ranolazine compared to patients treated with placebo (p = 0.002).
Due to the small number of non-white patients in controlled clinical trials, it is not possible to draw conclusions regarding the effectiveness and safety of ranolazine in this group of patients.
In the RIVER-PCI study of 2604 patients aged ≥18 years with a history of chronic angina with incomplete revascularization after percutaneous coronary intervention (PCI), the dose of ranolazine was gradually increased to 1000 mg twice daily. The risk of all-cause death, cardiovascular death or major adverse cardiovascular events (MACEs), and hospitalization for heart failure was similar between groups in the overall population; however, LBP was more common in patients ≥75 years of age receiving ranolazine compared with placebo (17.0% and 11.3%, respectively); in addition, there was a numerical increase in all-cause mortality in patients ≥ 75 years (p=0.074). There were no statistically significant differences between the ranolazine and placebo groups in the primary composite endpoint (time to first ischemic revascularization or ischemic hospitalization without revascularization). In clinical trials, ranolazine did not affect overall mortality, mortality from cardiovascular disease and the incidence of symptomatic arrhythmias in patients with stable angina.