Deformities of the cranio-vertebral region
Fig. 1 General diagram of anomalies in the forms of the craniovertebral junction (Koval G.Yu. General issues of X-ray diagnosis of diseases of the skull)
Fig. 2 Basilar impression (Fig. 2a). Sagging of the squama of the occipital bone (Fig. 2c). Convexobasia (Fig. 2b).
Variants of normal skull shapes
Fig. 3 General diagram of normal variants of skull shapes (Koroluk I.P. “X-ray anatomical atlas of the skeleton”).
Mesocephalic skull (Mesocrane) is the normal anatomical shape of the skull, the average statistically encountered shape is the standard shape of the skull.
Dolichocephalic skull (Dolichocephalic) - a significant predominance of the anteroposterior size (A) of the skull over the frontal size (B).
Fig. 4 Dolichocephalic skull (Dolichocephalus)
Brachycephalic skull - an increased value of the frontal dimension (B) of the skull over the anteroposterior dimension (A).
Fig.5 Brachycephalic skull
Acrocephaly (Acrocephalus) is the predominance of the vertical size of the skull over the anteroposterior and frontal.
Fig.6 Acrocephaly
Variants of pathological forms of the skull
Additional seams. Suture bones
Fig. 7 Normal (Fig. 7a). Metopic suture (arrow in Fig. 7b). Intercalated suture bone in the area of the apex of the lambdoid suture (arrows in Fig. 7c).
Fig. 8 Intercalated suture bone at the junction of the coronal and sagittal suture (Fig. 8a). Fusion (synostosis) of the nasal bones and frontal bone in a patient with an occult nasal meningocele (Fig. 8b). Congenital isolated deformity of the frontal bone (Fig. 8c).
Plagiocephaly is an asymmetry of the human skull, or curvature of the bone shape, regardless of the cause. Most often it occurs with asymmetrical fusion of cranial sutures and growth of the skull in the direction with remaining open growth zones.
Fig.9 Plagiocephaly. Frontal plagiocephaly (Fig. 9a and Fig. 9b). Occipital plagiocephaly (Fig. 9c).
Frontal plagiocephaly - as a result of unilateral synostosis at the site of the coronal suture, the frontal region on the ipsilateral side is flattened, on the contralateral side it is convex, which causes pronounced asymmetry of the skull (“harlequin eye”).
Occipital plagiocephaly - as a result of unilateral synostosis at the site of the lambdoid suture, the occipital region on the ipsilateral side is flattened and the frontal region is excessively convex.
“Accept and live life to the fullest”: advice to parents of children with disabilities
A child with a disability was born into the family. The familiar world for parents is turned upside down and becomes different. People who have never encountered such a problem before sometimes do not know who to contact, where to go, and waste precious time. Chairman of the Public Council for Young Disabled People 18+ at the Department of Labor and Social Protection of the Population of the City of Moscow, expert of the Council of Trustees in the Social Sphere under the Government of the Russian Federation and Chairman of the Council of the Moscow City Association of Parents of Disabled Children (MGARDI) Yulia Igorevna Kamal answers the most important questions about what the first steps of parents should be so as not to miss the opportunity to rehabilitate their child.
— A child with a disability was born into the family. This is a lot of stress, both physical and psychological. What should a family do to avoid missing out on time and the opportunity for recovery? Where to turn for help first?
— The fact is that it is extremely rare that disability is diagnosed in the first year of life. And here, first of all, doctors will be able to help the baby, and both social service employees and non-profit organizations, such as MGARDI and others, will be able to help the family. It is worth noting that under the word “help” lies a huge and diverse complex. And only by combining the efforts of all organizations can we count on success.
It is very important for a structure such as the Early Help Service to work in our city. So far, such a service is available only at the Scientific and Practical Center for Medical and Social Rehabilitation of Disabled People named after L. I. Shvetsova and the Butovo Center for Comprehensive Rehabilitation of Disabled People. It is very important to develop this direction; an interdisciplinary team of specialists should get involved as early as possible and help not only the child, but the whole family.
Julia Kamal. Photo: Website of the Moscow City Duma duma.mos.ru
— What social services are provided to children with disabilities free of charge? How can the state help the family?
— Support measures are very diverse. In addition to federal measures, each region implements its own regional projects. In Moscow, this means not only payments, but also on-site rehabilitation, recreation and wellness, tax breaks, free travel on public transport, financial measures of additional support and much more. Parents often contact us with this question, and we inform them about all aspects of assistance in the city. MGARDI and ROO “Contact” have been implementing the “Parental Reception” project for several years: parents of children with disabilities address their problems, and our organizations help solve them. For five years now we have been holding an annual Congress of families raising children with disabilities and young people with disabilities. At the Congress there are consultation platforms for executive authorities, where everyone can get help in solving their problem. In parallel, discussions and round tables are held where systemic problems are discussed and ways to solve them are outlined.
— You often communicate with families raising a child with a disability. From your experience, what advice could you give to families to avoid emotional burnout?
— It’s easiest to give advice, but you need to understand that everyone has their own path and their own views. In my opinion, the most important thing is to love a child, learn to understand him and enjoy any successes, even the most seemingly insignificant ones. A special child is not a reason to stop living life to the fullest. Yes, life will change, and all the good in these changes depends only on ourselves. You need to accept and live a full and happy life.
— There are rehabilitation and educational centers in Moscow. Should parents strive to send their child there or should they make every effort to ensure that he or she attends a regular school? What is the best thing to do from a physical and psychological point of view?
— You only need to strive to ensure that the child is comfortable receiving knowledge to the extent of which he is capable. And where he gets them is the parent’s choice. All children are different, some feel great in inclusion, while others are more successful in a rehabilitation center. It is important that such centers exist in Moscow. I would like this unique experience to be replicated in the regions.
— In your opinion, how important is interaction with government agencies?
— It’s very important, without this not a single project will work, not a single idea will eventually become a document. The ability to conduct a dialogue, hear, listen and look for solutions together is the main thing.
— What issues did MGARDI manage to resolve last year?
— I would like to tell you something global: we have many issues that may not be important on a city scale, but on the scale of one family, on the contrary, are extremely important. Ramps, education, drug supply, legal issues: we deal with all this year-round. However, the biggest issue is the decision of the Ministry of Labor to cancel the requirement to submit electric wheelchairs and devices for medical and technical examination after the expiration of their use, as well as to confirm compliance in the case of independent purchase. Accordingly, all those who previously received a refusal due to the impossibility of submitting the above-mentioned technical means of rehabilitation for medical and technical examination due to their loss, disposal or non-compliance of the purchased product can apply again with an application for issue or compensation. Only prostheses with external energy sources remain on the list. Non-profit organizations have become involved in resolving this issue. Through joint efforts we managed to achieve this result.
— On June 8, Russia celebrated Social Worker Day. What would you like to wish to your colleagues from social protection?
— I want to wish all social workers health and happiness! May all good deeds return to them a hundredfold! Thank you for having us!
Press service of the Department of Labor and Social Protection of the Population of Moscow
Normal formation of cranial sutures
After 3 years, throughout the entire length, the width of the lumen of the seam does not exceed 0.5-1.0 mm. In adults, the lumen of the suture looks like a thin hairline and cannot be measured. Starting from the 2nd year of life, the lumen clearly competed, and from 4-8 years an intense stripe appears along its edge - the so-called zone of physiological sclerosis (Fig. 10a and Fig. 10b).
Fig. 10 Cranial sutures of a 2-year-old child (Fig. 10a), cranial sutures of a 9-year-old child (Fig. 10b), craniostenosis in a 4-year-old child (Fig. 10c).
What is craniostenosis in children?
First of all, it depends on whether the child has other developmental defects. Sometimes pathology accompanies various syndromes - then it is called syndromic. For example, it can occur simultaneously with fusion of fingers or toes, cleft palate or lip, or cerebral hernia.
If fusion of the sutures in the bones of the skull occurs without other developmental defects, it is considered non-syndromic, that is, independent.
Doctors classify the disease into types based on which cranial sutures are fused:
- metopic,
- lambdoid,
- coronary,
- sagittal.
Synostosis - or suture fusion - can involve one to several sutures. There is a concept of pansynostosis - complete overgrowth of all seams. This type of pathology can be considered the most severe; it is less common than others.
Craniostenosis
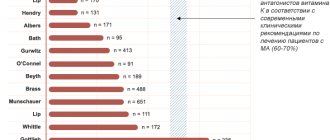
Craniostenosis is the most common developmental disorder of the skull (Fig. 10c). According to V. A. Kozyrev (1969), Schurmann and co-authors (1969), it is observed in 0.7% of newborns, more often in boys (65%).
Normally, the increase in the volume of the brain and skull is strictly correlated. Premature cessation of suture function while the brain continues to grow leads to craniostenosis. Untimely closure of cranial sutures and fontanelles is accompanied by a decrease in volume and deformation of the brain skull.
Fig. 11 Craniostenosis in a 4-year-old child
Based on the number of synostotic sutures, the following are distinguished:
- full
- partial craniostenosis,
by time
- early (occurring in utero or at the age of 1-3 years, that is, during the period of most active brain growth),
- late and
- premature (during the period of slow brain growth),
according to the rate of development of synostoses
- fast
- slow,
in phase
- progressive
- and stabilized
by stage
- compensated and
- decompensated.
With craniostenosis, primary damage to the nervous system is usually not observed.
The pathology can be combined with deformation of the base of the skull and anomalies of the vertebrae. A combined disorder of the formation of the skull and limbs is called craniosynostosis-syndactyly and can be accompanied by brain atrophy, hydrocephalus, congenital heart defects, kidney defects, hypogonadism, diabetes mellitus, etc.
The combination of craniostenosis with syndactyly is explained by the fact that differentiation of both the skull and limbs occurs between the 29th and 35th days of embryogenesis. The earlier intrauterine development is disrupted, the more significant the changes.
Craniostenosis is inherited. In this case, there is a developmental disorder with autosomal transmission according to a recessive trait. This is especially clearly seen when craniostenosis is combined with syndactyly. The possibility of mutations cannot be ruled out.
With craniostenosis, intracranial hypertension develops.
Closure of one of the main sutures of the cranial vault with partial craniostenosis leads to characteristic deformities:
- synostosis of the metopic suture causes the formation of a sphenoid frontal bone (trigonocephaly);
- closure of the coronal suture - its flattening (platycephaly) and development of the tower skull (turicephaly, acrocephaly);
- early closure of the sagittal suture of the skull acquires a scaphoid shape (scaphocephaly);
- isolated synostosis of the lambdoid suture is characterized by flattening of the occipital bone (bothriocephaly);
- asymmetrical closure of the coronoid or lambdoid sutures forms an oblique skull (plagiocephaly).
Fig. 12 Asymmetric synostosis of cranial sutures.
Why is craniostenosis dangerous?
The absence of movable sutures in the skull severely limits the brain. Therefore, the sooner help comes for craniostenosis, the higher the likelihood of a complete cure for the child in the future. Compensation mechanisms in infants under 2 years of age are very high, but rehabilitation after this age turns out to be more complex and lengthy. If not treated promptly, the disease can cause the following conditions:
If you do not receive treatment in a timely manner, the disease can cause the following conditions:
- delayed physical, mental, intellectual development;
- disruption of normal brain functions;
- skeletal underdevelopment;
- compression and atrophy of the optic nerve up to complete loss of vision;
- headache;
- ophthalmological diseases;
- death.
Synostosis of cranial sutures
Synostosis of sutures normally begins after 30 years, but it is possible for sutures to persist into old age. Earlier, the coronal and sagittal sutures synostose, later the lambdoid, and only in old age can synostosis of the parietal-mastoid, occipital-mastoid and squamosal sutures be observed.
Fig.13
Since the sutures are growth zones, even their partial premature closure leads to a pathological change in the shape of the skull. Additional sutures are formed due to the development of the bones of the arch from several ossification points. They are characterized by early synostosis.
Mental factors
Also, chronic traumatic situations associated with:
- conflict between drives and sense of duty;
- emotional stress due to increased responsibility;
- requirements for the child from the parents.
These children, even before the appearance of obsessive states, show excessive fearfulness of everything new (moving from one place to another, meeting strangers). In preschool age, they are characterized by suspiciousness, a tendency to come up with various prohibitions against themselves, and a belief in magic. During games, they like to come up with new rules, similar to rituals, and are also characterized by strict consistency when performing everyday actions, for example, dressing or eating.
In almost 90% of cases, a schoolchild suffering from obsessive-compulsive disorder has problems in school, family relationships, and difficulties communicating with peers.
Cephalohematoma
Cephalohematoma is not quite an anomaly of the skull, but a pathological local deformation of the skull that occurs in the postnatal period due to trauma and the use of forceps during childbirth, in which hemorrhage occurs between the inner and outer plates of the diploe. If this hematoma is not evacuated in childhood, it will persist throughout life, and cloud-like calcifications can be found in its stoma.
Fig. 14 Cephalohematoma
Infections
In the genesis of obsessive-compulsive disorders , the role of an infectious disease is primarily played by streptococcal (beta-hemolytic streptococcus) infection of the nasopharynx.
Typically, patients suffering from streptococcal infections begin to show signs of obsessive-compulsive disorder 3-4 years earlier than other children suffering from obsessive disorders, for example, arising from organic brain damage due to an unsuccessful birth.
The role of infection is indicated by exacerbation of symptoms in the evening and the clearly recurrent nature of the disease. The doctor should also take into account the fact that with obsessions that arise during the neuroinfectious process, the following is noted:
- pronounced emotional lability;
- pronounced anxiety reaction in case of separation from parents;
- motor hyperactivity;
- impulsivity and absent-mindedness, correlated in time with an exacerbation of streptococcal infection.
Morgagni syndrome
Morgani-Stuart-Morel syndrome (Morgagni syndrome) is not a developmental anomaly, but in this context appears based on its anatomical location. This pathological process is called pluriglandular syndrome ; it usually develops in postmenopausal women with metabolic disorders, obesity, and arterial hypertension. The diagnostic criterion is a thickening of the diploe of the frontal bone and an uneven, tuberous, irregular shape; there may even be an asymmetrical thickening of the internal plate of the diploe of the frontal bone. The reason for such local bone hypertrophy is seen in the remaining sensitive receptors to growth hormone in this area, which is replaced by a structurally similar glucocorticoid hormone. However, the cause of this hyperostosis is not completely clear. Clinically it usually does not manifest itself in any way.
Fig. 16 Morgagni syndrome
Craniostenosis, craniosynostosis and cranial deformities
Craniostenosis, craniosynostosis and cranial deformations are the result of premature or uneven ossification of cranial sutures (Greek kranion - skull; synostos - fusion; stenos - narrow, close). The incidence of craniostenosis is 1 in 1000 newborns. The immediate cause of the development of craniostenosis is seen in: a) metabolic disorders, which entails accelerated osteosynthesis of the skull bones (Greek osteon - bone; synthesis - connection, combination, composition); b) disorder of the blood supply to the bones and membranes of the brain; c) reducing the force acting through the dura mater on the cranial vault and promoting its stretching.
There are primary, or idiopathic (Greek idio - special; pathos - suffering, disease), and secondary craniostenosis. Primary craniostenosis is hereditary or associated with a hereditary predisposition. This, for example, is the symptom complex of Tersil (1942), which includes: 1) tower skull; 2) exophthalmos; 3) nystagmus; 4) mental retardation; 5) epileptic seizures; 6) intracranial hypertension and 7) optic atrophy with blindness. Primary craniostenosis is included in the clinical picture of many hereditary mental retardation syndromes with different types of inheritance. Secondary craniostenosis develops for various external reasons, such as inflammatory processes, vitamin D-deficiency rickets, phosphorus deficiency in the blood, overdose of thyroid hormone (in the treatment of hypothyroidism), X-ray exposure in the first half of pregnancy.
Normally, in newborns, all the bones of the skull are not fused, the anterior and posterior fontanelles are open. The posterior fontanel closes by the end of the 2nd month, the anterior one - during the 2nd year of life after childbirth. By the end of the 6th month, the bones of the calvarium are connected to each other by a dense fibrous membrane (Latin fiber - thread). By the end of the 1st year, the child’s head size is 90%, and by 6 years it reaches 95% of the adult’s head size. The closure of the sutures by connecting the jagged edges of the bones begins by the end of the 2nd year and is completely completed by the age of 12–14 years.
Premature overgrowth of the fontanelles and cranial sutures leads to a narrowing of the skull and a decrease in the volume of the cavity of the cranium. This interferes with normal brain development and creates conditions for liquorodynamic disturbances. With an increase in intracranial pressure, an associated hypertensive headache occurs (Greek hyper + Lat. tension - tension). The development of congestion in the fundus of the eye, concentric narrowing of the visual fields, and subsequently secondary atrophy of the optic nerves with a progressive decline in vision up to its loss are also possible. Typically, exophthalmos occurs on both sides, disorders of the oculomotor nerve, thinning of the skull bones, and the appearance of digital impressions in the bones of the calvarium, visible on x-rays. There is a high risk of developing mental retardation.
In case of secondary craniostenosis in the early stages of its formation, conservative treatment of the underlying disease can be effective. In case of primary craniostenosis, as well as secondary craniostenosis in the case of already developed significant intracranial hypertension, shunting and decompression therapy are indicated: the formation of craniectomy passages up to 1 cm wide along the line of suture ossification. Timely surgical treatment for craniostenosis ensures further normal development of the brain.
Premature or uneven overgrowth of the fontanelles and cranial sutures also leads to deformation of the skull. The shape of the skull is assessed taking into account the cranial index (CI) - the ratio of the transverse and longitudinal dimensions of the skull. Normally, or mesocephaly (Greek mesos - average), the CI is 76–80.0 in men, 77–81.9 in women. With premature overgrowth of the sagittal (Latin sagittal - arrow) suture dividing the skull into the right and left halves, dolichocephaly (Greek dolichos - long) occurs with a CI of less than 75. A variant of dolichocephaly is scaphocephaly (Greek skaphe - boat) or cymbalocephaly (scaphoid head), in which the elongation of the head is complemented by a protruding forehead and nape. There may also be a saddle-shaped skull - it is elongated and depressed in the parietal region.
With premature overgrowth of the coronal sutures (coronal or coronal synostosis), brachycephaly occurs (Greek brachys - short) - an increase in the transverse size of the head with a CI of more than 81. In this case, the face of children is flattened, and exophthalmos often occurs. With premature overgrowth of the coronal suture on one side, plagiocephaly (Greek plagos - oblique), or cross-headedness is formed: the skull is asymmetrical, the frontal bone on the side of the synostosis is flattened, on the same side there may be exophthalmos, as well as an increase in the middle and posterior cranial fossae.
If both the sagittal and coronal sutures heal prematurely, the growth of the skull continues only in height. As a result, a high conical skull is formed, somewhat flattened in the anteroposterior direction - acrocrania (Greek akron - limb), or tower skull. A variant of acrocrania is a pointed skull, or oxycephaly (Greek oxis - sharp) - a high skull, tapering upward and with a sloping forehead.
Premature fusion of the frontal suture is characterized by a narrow frontal and broad occipital bone. In this case, the frontal bones grow together at an angle, and a “ridge” is formed at the site of the frontal suture. If the posterior parts of the skull enlarge compensatoryly and its base deepens, trigonocrania occurs (Greek trigonon - triangle).
Brachycephaly, scaphocephaly and trigonocephaly are usually not accompanied by neurological pathology. If there is no brain damage, then there is no psychiatric pathology.
Return to Contents
Kimerli anomaly
Kimerli's anomaly is not an anomaly of the skull, but appears in this context due to its anatomical location and clinical significance. The anomaly is the formation of a bone bridge at the site of the presence of a ligament above the groove of the vertebral artery of the atlas , completely covering the ring with the formation of the opening of the vertebral artery of the atlas or partially - in the form of a semi-ring.
Fig. 17 Kimerli anomaly
Pathogenesis at different stages of OCD
Obsessive actions have an ambiguous pathogenesis at different stages of the disease.
For example, in schizophrenia: first the protective nature of rituals, then (with the disappearance of the emotional component) - motor and speech automatisms. Children with obsessions try to avoid homework and household responsibilities. Obsessive states in children are often combined with depressive and anxiety disorders. For example, adolescents may develop an obsessive urge to commit suicide. Also relatively often, apparently in at least a third of cases, obsessions are accompanied by various tics.
Monotonous, stereotypical movements are observed in cases of mental retardation, autism, tics; obsessions occur in eating disorders.
Bibliography
- Koval G. Yu., Danilenko G. S. “X-ray diagnosis of diseases and injuries of the skull.
- Esinskaya G.N. “A short guide to neuroradiology”, Medicine Publishing House, 1965.
- I.P. Korolyuk, “X-ray anatomical atlas of the skeleton (norm, options, interpretation errors)”, Moscow publishing house “VIDAR” 1996.
Author: radiologist, Ph.D. Vlasov Evgeniy Alexandrovich
Full or partial reprint of this article is permitted by installing an active hyperlink to the source
If you still have doubts about the conclusions of your MRI, you can order a review of your study with a detailed transcript here: