With vitiligo, light spots with evenly defined edges form on the skin of the hands, face or entire body. The pathology is non-contagious and has the nature of a chronic disease that occurs for internal reasons. The disease can progress, that is, go through several stages in development and become more and more noticeable. The appearance of a person with vitiligo attracts the wary attention of others and often becomes a cause of psychological discomfort.
It is important to understand that vitiligo is not just a cosmetic skin defect. Pigmentation disorders can cause serious problems in the body that require attention and, without treatment, can lead to complications. You can consult a doctor for symptoms of vitiligo, undergo diagnostics and discuss treatment options with a specialist at the Medical Center on Botanichnaya.
What is vitiligo and how does this disease manifest itself?
The disease vitiligo is a disorder of the synthesis of melanin, the skin pigment. In some areas of the skin, the number of special cells - melanocytes, which give the skin its usual color, sharply decreases.
As a result, light beige, almost white spots of irregular shape are formed, which stand out sharply against the background of healthy skin and are separated from it by clear boundaries. The number and size of spots may vary depending on the stage of the disease.
Light areas appear:
- on the face;
- on the skin of the hands, most often on the elbows, wrists and backs of the hands;
- under the knees;
- in the armpit area;
- in the groin and other parts of the body.
Sometimes the disease also affects the scalp, and in men, the skin in the area where the beard and mustache grow.
Vitiligo is characterized by the sudden appearance of depigmented spots due to a violation of the secretory function of melanocytes or their death, develops in individuals with a genetic predisposition, is accompanied by pronounced dysregulatory changes in cell-mediated reactions of the immune system, autonomic imbalance with a predominance of sympathetic tone and serious social maladaptation caused by personal characteristics and external social factors.
Vitiligo is a common dermatosis. In the world, the number of patients with this disease exceeds 1% of the total population. In 70% of cases, the disease begins at the age of 10-25 years; children under 10 years of age, including newborns and infants, make up approximately 25% of all patients with vitiligo [1]. Vitiligo can occur at any age, lasts indefinitely, and spontaneous restoration of normal skin color is rare.
The reasons for the appearance of depigmented lesions are not known. It is not clear enough as a result of what disorders the synthesis of melanin abruptly stops and melanocytes die. Various endogenous and exogenous factors can have direct and indirect damaging effects on melanocytes.
Among external factors, the most important are infectious and toxic agents, excessive ultraviolet radiation, and stress. For many decades, vitiligo has been associated with autoimmune thyroiditis, rheumatoid arthritis, lupus erythematosus, atopic dermatitis, liver diseases of infectious or toxic origin, helminthic infestation and a number of congenital syndromes [2]. However, the incidence of vitiligo in these patients is no higher than in the general population. A number of authors [3, 4], summarizing the results of many years of research, believe that patients with vitiligo in most cases do not have any severe or chronic concomitant diseases, and therapy for functional disorders of the digestive organs, vegetative-vascular dystonia, identified in 28% of patients, had no effect on the result of repigmentation .
Many researchers believe [5, 6] that vitiligo is a serious cosmetic defect that occurs in individuals with a genetic predisposition and, in most cases, who have suffered emotional disorders. Only 4-7% of patients have vitiligo combined with autoimmune thyroiditis.
Modern genetic studies have demonstrated the connection between the occurrence of vitiligo and various aspects of inheritance. Among sporadic cases of vitiligo in the European population, the average age of onset of the disease is 24.2 years, while in families with multiple cases of the disease, the average age is 21.5 years (statistically significant differences) [7]. Earlier onset of disease in “familial” cases and risk of disease in distant relatives is a typical characteristic of polygenic disease. About 20% of vitiligo patients have at least one blood relative with a similar disease. Formal genetic segregation analysis of vitiligo determines the existence of many loci, disturbances in which form a predisposition to vitiligo. However, the key genes responsible for the manifestation, progression or predisposition to this disease have not been discovered.
In vitiligo, a decrease in antioxidant potential was found, leading to an active damaging effect on melanocytes of free radicals and the accumulation of lipid peroxidation products [8, 9]. Later it turned out that free radicals have a damaging effect on various cells involved in various types of inflammatory reactions, and violations of antioxidant defense are not the main mechanisms of depigmentation in vitiligo.
The theory of disorders of immune regulatory mechanisms is the most substantiated. With a long course and widespread pathological process, changes in the subpopulation composition of T-lymphocytes are observed. At the same time, especially in the initial stages of the disease, the levels of lymphocyte activation receptors increase, reflecting the degree of activation of immunocompetent cells [10]. Currently, most researchers believe that the leading role in the development of autoimmune diseases belongs to cell-mediated reactions, in which a pronounced imbalance of cytokines is observed. In vitiligo, a decrease in the activity of regulatory T-lymphocytes is detected, which is confirmed by a decrease in the amount of transforming growth factor-β (TGF-β) and interleukin-10 (IL-10) in the blood serum of patients [11].
Treating vitiligo is a daunting task. Since the causes of its occurrence are unknown, in most cases the disease develops against the background of complete physical well-being. It is proposed to use mainly topical steroids and/or immunomodulators for lesions up to 20%, as well as long-term phototherapy [12, 13]. Complex therapy includes enzyme preparations, hepatoprotectors, vitamins and microelements (zinc, copper) [14, 15]. A number of recommendations contain information on the use of sedatives and antidepressants.
The purpose of this study is to study the clinical features of the course of vitiligo and the effectiveness of complex therapy, including the immunomodulatory component - thymogen and externally 1% pimecrolimus, and the correction of affective disorders in patients with various forms of vitiligo using the antidepressant drug agomelatine.
Material and methods
All patients with different forms of vitiligo were fully examined (clinical blood and urine tests, biochemical blood tests, ultrasound examination of the abdominal organs and thyroid gland, thyroid hormones T3, T4, thyroid-stimulating hormone - TSH and antibodies to thyroid peroxidase - AT-TPO according to indications, consultation with a neurologist according to indications, consultation with a psychiatrist, immunological studies - population and subpopulation composition of lymphocytes, levels of pro-inflammatory and regulatory cytokines).
results
From 2006 to 2011, we observed 84 patients with vitiligo (46 women, 38 men) aged 18 to 56 years.
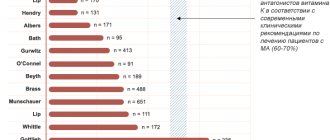
The duration of the disease varied from 6 months to 30 years, the average duration was 6.5±4.8 years. Among the probable reasons for the development of vitiligo, most patients named stress (39 patients, 46%). Vitiligo occurred after surgery in 3 (3.5%) patients, after trauma - in 4 (4.5%). According to 4 (5%) women, depigmented spots first appeared after childbirth, during lactation, and 1 patient noted that after the 2nd and 3rd births the area of the lesion increased and fresh lesions appeared. In 14 (17%) patients, the disease occurred after exposure to prolonged ultraviolet radiation; 20 (24%) patients could not associate the appearance of depigmented spots with any significant causes (Fig. 1).
Figure 1. Probable causes of vitiligo. 21 patients among their immediate relatives had manifestations of vitiligo of varying duration and degree of prevalence; in 2 of them, in addition to skin lesions, areas of hair were discolored.
When examining patients with vitiligo, it was found that the most common (in 48 patients, 57.1%) are biliary dyskinesia and cholelithiasis, chronic cholecystitis, and fatty hepatosis. Gastritis was found in 16 (19%) patients. During the examination, pathology of the thyroid gland (autoimmune thyroiditis, diffuse toxic goiter, thyroid cysts) was identified or confirmed in 13 (15.4%) patients with vitiligo. Only 4 out of 13 patients with thyroid pathology had AT-TPO detected, which confirmed the diagnosis of autoimmune thyroiditis.
Gynecological diseases (dysfunctional menstrual cycle disorders, fibroids) were found in 5 (5.9%) women. In 10 (11.9%) patients, hypertension of I-II degree was confirmed, in 1 (1.2%) type 2 diabetes mellitus was detected, in 3 (3.5%) alimentary obesity of II-III degree was detected. No significant deviations from normal values were found in clinical blood tests. No severe chronic diseases or decompensated conditions were identified in patients with vitiligo (Table 1).
We observed patients with different forms of vitiligo (Table 2).
Among them, 7 (8.3%) patients had a segmental form with a lesion area of 2% (Fig. 2).
Figure 2. Segmental form of vitiligo. The vulgar form was observed in 44 (52.3%) patients. In these cases, the affected area was 3-70% of the skin area (Fig. 3, a, b).
Figure 3. Patient (a) and patient (b) with vulgar form of vitiligo. A separate group consisted of patients with the acrofacial form (31 people, 36.9%) with depigmented lesions on the face and limbs (Fig. 4, a-c).
Figure 4. Acrofacial form of vitiligo (a-c). In 10 (11.9%) patients, clinical examination revealed Setton's nevi (Fig. 5).
Figure 5. Setton's nevi.
Vitiligo is a serious psychological problem [16, 17]. When studying the level of anxiety using the Spielberger-Khanin method, a low level of reactive anxiety was observed in 52 (61.9%) patients, and in 32 (38.1%) moderately severe reactive anxiety. In 55 (77.4%) patients with vitiligo, a high level of personal anxiety was noted, and it did not depend on either the area of the lesion or the duration of the disease. The presence of depressive disorders was confirmed using the Hamilton Hospital Scale (average score 13.9±2.4 points) and the Beck Scale (average score 22.4±2.8 points). The majority of those examined had depressive disorders of a neurotic level, characterized by depressed mood, sleep disturbance, anxiety and asthenic manifestations.
Thus, the examination did not reveal any severe concomitant diseases. According to the literature, affective and autonomic disorders are observed in almost all patients with vitiligo and require adequate correction.
An immunological study carried out on 25 patients with vitiligo revealed significant deviations from control values in the subpopulation composition of T-lymphocytes and an imbalance of pro-inflammatory cytokines (Table 3; Fig. 6).
Figure 6. Content of cytokines in the serum of patients with vitiligo. Note. IL-2, IL-8, TNF-α, IFN-γ, IL-10 in pg/ml; TGFβ, in ng/ml. Thus, the content of CD8+ in the blood of patients with vitiligo was significantly higher than that of healthy people, and the immunoregulatory index (IRI) also had significant differences from control values. In the blood serum of patients with vitiligo, increased levels of IL-2, IL-6, IL-8 and tumor necrosis factor-α (TNF-α), interferon-γ (IFN-γ) were found against the background of low levels of regulatory cytokines TGF-β and IL -10 compared to control.
Complex treatment of patients was carried out taking into account the clinical features of vitiligo, including duration, prevalence and activity of the pathological process. We used targeted immunomodulatory therapy - thymogen (nasal spray 1 ml/day for 20 days) and pimecrolimus (1% cream 2 times a day for 4-6 months). Psychocorrective therapy was carried out with agomelatine, which is a melatonin agonist (MT1 and MT2 receptors) and a 5HT2c antagonist. Patients with vitiligo took agomelatine 25 mg/day once a day for at least 6 weeks. After consultation with a psychiatrist, 5 patients with moderate signs of depression were prescribed agomelatine at a daily dose of 50 mg for 12-24 weeks.
We carried out complex treatment for 57 patients with different forms of vitiligo (3 patients with the segmental form, 25 with the acrofacial form, 29 with the vulgar form).
In all patients with segmental form of vitiligo, 100% repigmentation was observed 4 months after the start of therapy.
In patients with the acrofacial form, complete clinical remission was observed in 16 (64%) cases after 5 months of therapy. Significant improvement with 100% repigmentation of most lesions and a reduction in the area of depigmentation lesions by more than 60% was observed in 7 patients. Insignificant effectiveness was noted in 2 patients, and the normal color of the skin in the periorbital and perioral areas was completely restored, on the dorsum of the hands and in the phalanges, the area of depigmented lesions remained practically unchanged, the area of lesions in the area of the ankle joints partially (up to 40%) decreased.
Positive changes after complex therapy were observed in all patients with vulgar form of vitiligo. Clinical remission was observed in 20 of 29 patients in this group.
During the first 3 months of therapy (12 weeks), these patients began to actively repigment the lesions, the area of which was reduced by 30-60%. By the end of the 6th month, the skin color was completely restored.
In 6 patients, there was a reduction in the area of depigmented lesions by 50-70% due to complete repigmentation of individual lesions and partial restoration of normal skin color in individual areas. In 3 patients, minor positive changes were observed, which were expressed in the restoration of pigmentation in fresh, small areas (no more than 2 cm2), smoothing of the boundaries along the periphery of the foci of depigmentation (Table 4).
All patients tolerated the treatment well; there were no side effects, complications, or refusals of therapy. In the process of therapy, it was possible to change the patients’ attitude towards their disease and evaluate positive changes in the treatment process. Against the background of active repigmentation of the lesions, immunological indicators normalized and there was a reduction in signs of depressive disorders.
Thus, our results indicate the possibility of reasonable effective and safe treatment of vitiligo.
Stages and forms of vitiligo
There are several stages of vitiligo:
- Initial stage. The first light area on the skin appears and, in general, the pigmentation of the skin is disturbed.
- Progressive vitiligo. At this stage, the shade of the spots changes, the difference in the pigmentation of skin areas becomes more noticeable, and new light areas appear. This usually happens gradually over 3–4 months. But in 20% of cases, vitiligo develops at lightning speed.
- Stationary vitiligo . New spots no longer appear during this period and no significant changes occur in the condition of the skin. The shade of the affected areas may vary slightly, but within the established boundaries.
- Repigmentation . This is the improvement stage when light spots on the skin gradually regain their natural shade. It can occur as a result of effective treatment or with mild reversible forms of vitiligo (arising, for example, as a side effect after a procedure by a cosmetologist or taking medications).
There are also two forms of the disease depending on the size of the affected area. If light spots are located within one area on the body (for example, vitiligo on the face), they speak of a segmental form of the disease. If vitiligo affects almost the entire body, it is a generalized form.
“Of course, we’ll have to learn to live with it all over again.”
Daria, 31 years old
“I developed vitiligo 14 years ago. I was 17, I was entering my first year of college. It was not clear why it started - spots simply appeared on the thighs and began to grow. Now I even have vitiligo on my face, around my eyes.
The doctor told me that there is very little information about this disease. I bought some ointment at the pharmacy and tried to be treated with folk remedies, but then I stopped using anything - nothing helped.
Of course, complexes appeared. I cried, was very worried, and used foundation to cover it all up. Some ill-mannered classmates asked me: “Are you sunbathing with glasses on? What are your spots? Of course, I was embarrassed, I wanted to turn away, hide... It’s just this kind of situation: you live for 17 years with the same appearance, and then one day it changes not at all according to your wishes. Of course, you will have to learn to live with this again.
My boyfriend helped me accept myself. When I started communicating with him, he gave me the opportunity to believe that I was special, that there was nothing special about my spots. I posted my first photo with vitiligo on Instagram in 2021, when someone wrote to me in direct message: “What’s wrong with your face?” And I decided to post a photo without filters, without anything, and write that I have vitiligo and that it is not contagious. Many acquaintances, having seen the photo, wrote to me that they did not even notice my spots and did not pay attention to them. In general, everyone reacted adequately.
Now many people come to me with the same problem as me, especially those who have it recently: “You are such a cheerful girl, how do you cope? I’m depressed because of this...” I’m pleased that I’m sharing my experience: maybe it will help someone. And if they write to me something about some new treatment for vitiligo, I immediately close the dialogue. I have already accepted this fact and I don’t want to give myself unnecessary hope. Only time will help you accept yourself. “Reconcile” is not the right word here, just accept. It took me five years.
Causes of vitiligo
The causes of vitiligo are always internal: it is a non-infectious disease.
Factors that can trigger the development of the disease include:
- Heredity. Melanin deficiency can be congenital, and this increases the risk of vitiligo.
- Malfunctions of the immune system. In 1959, A. Lörincz suggested that some patients develop vitiligo due to autoimmune disorders, and today this is a scientifically accepted theory.
- Neuroendocrine causes are malfunctions of the adrenal glands, pituitary gland, ovaries, pancreas and other organs that produce hormones.
- Sun, thermal and chemical burns, skin injuries, as well as systematic ultraviolet irradiation without protective equipment with SPF.
- Gastroenterological diseases: disorders of the liver, stomach, intestines.
- Infectious diseases of a viral or bacterial nature (vitiligo can develop against a background of weakened immunity).
- Severe intoxication.
- Severe stress.
Although it has been proven that a predisposition to vitiligo is sometimes transmitted genetically, it is rare for a child to be born with this pathology. As a rule, vitiligo on the hands, face or body develops later: from 10 years to about 30 years of age.
Science has established the causes of vitiligo not so long ago, but the disease itself has been known since ancient times. The term “vitiligo” was first used by the ancient Roman physician Aulus Cornelius Celsus (1st century AD).
“Mom has white bangs, and so do I.”
Alina, 28 years old - I have had vitiligo since birth.
Until I was six years old, I was taken to doctors, we tried all the folk remedies and even went to my grandmother to remove the damage. As a result, my family reconciled, realizing that it was all useless, and stopped tormenting me. I can say that I was lucky: my hands and face were not affected by vitiligo, but there are light strands on my head - such a white bang. On the arms, spots extend from the wrist to the elbow, and they are also present on the stomach and legs. At school, the teachers were indignant about why my mother dyed my bangs blonde, but she explained everything to them, and it ended. I don’t remember any reaction from my classmates.
Of course, in adolescence there was a rejection of appearance, there were complexes. I tried to wear clothes that were as closed as possible so that the stains would not be visible, and I used self-tanner. Vitiligo also affects your lifestyle - it’s better not to sunbathe, because you can instantly get burned. As a child, I was always burned.
There were no problems in my personal life or with friends. The only thing that bothered me was strangers who could look at me on the street. But the older you get, the less you care what others think. Previously, I hid the spots when strangers looked, but now, when they look at me, I look straight in the eyes - interest in me instantly disappears.
Now I have another problem: I worry about my daughter, how she will cope with the same situations that I had. She was also born with white bangs. While she is four years old, she doesn’t ask any questions, she just says: “Mom has white bangs, and so do I.” The husband reacts calmly to all this: he says that he got two such beauties.
Is vitiligo treatable?
Success in treating vitiligo depends on the causes of the disease.
If the pathology is genetic or appears as a result of incurable autoimmune disorders, it is often impossible to completely restore pigmentation. But well-chosen therapy will help stop the progression of vitiligo.
If the cause of vitiligo is reversible disorders in the functioning of internal organs, you need to start with their diagnosis and treatment. In this case, there is a chance for significant improvement.
In parallel with the treatment of the main internal problem, the doctor may prescribe procedures that affect the skin condition:
- a course of specially selected hormonal medications, as well as vitamin complexes;
- phototherapy;
- laser therapy;
- methods of hardware cosmetology: peelings, polishing, etc.;
- treatment with a UV lamp;
- skin whitening. This method does not directly treat vitiligo, but it reduces the contrast between light spots and pigmented areas;
- in rare cases, surgical intervention by transplanting healthy skin cells. This method is not always justified and has contraindications.
How to protect skin with vitiligo?
With vitiligo, protection is a very important step, especially if therapy is carried out and it helps. Tanning, going to the solarium, and so on are completely prohibited; you should always use products with SPF. There is no harm from SPF products, especially now the choice of products is huge, there are also decorative cosmetics with a sun protection factor.
To prevent burns, sunscreen must have a factor of at least 30 (SPF30). And to avoid tanning, the factor must be even higher, for example, SPF50. At the moment, SPF50 is the highest factor; if a product says 60 or higher on the packaging, then rest assured, this is already a marketing ploy.
Introduction
Vitiligo
- one of the most common types of hypomelanosis. According to official data, it affects from 3 to 6% of the world's population (the largest number of cases was recorded in Asia and the Middle East). However, in recent years, it appears that the number of patients with vitiligo has been steadily increasing. Let us recall that dyschromia is manifested by spots of depigmentation due to the loss of the ability of certain areas of the skin to produce melanin. This is due to the absence of the enzyme tyrosinase in melanocytes, which stimulates the process of pigment formation. Due to the presence of a pronounced cosmetic defect, patients with vitiligo experience severe stress and psycho-emotional discomfort. This dictates to clinicians and researchers the need to find new ways to treat this disease.
Currently, the lack of a holistic concept of the pathogenesis of vitiligo makes it difficult to develop a unified approach to treatment and predict the clinical course of this disease. In a number of scientific studies of the pathogenesis of vitiligo, preference is given to various theories: genetic, neurogenic, autoimmune, theory of oxidative stress, etc. All these theories have been repeatedly confirmed experimentally, but scientists have not yet come to a consensus. In addition, there are also a number of provoking factors: exposure to UV radiation, psycho-emotional stress, changes in the state of the peripheral nervous system, etc.
Disorders of skin pigmentation in vitiligo, provoking factors
For patients who suddenly experience skin discoloration, it may only seem like it happened out of the blue. In fact, the process could have been preceded for a long time by factors provoking it. Most suspicious:
- taking neurotropic substances, due to which the neuroregulation of the production of melanin pigment was affected;
- disruption of trophism (nutrition) of cells that produce melanin and “go on strike” in the form of “downtime” against forced “starvation”;
- inflammatory processes on the skin - especially recurring ones (for example, due to constant infection of skin wounds, even superficial ones);
- disruption of local immune processes of the skin in the form of autoimmune reactions.
At the moment, the role of heredity in the occurrence of vitiligo is also being studied.
But skin pigmentation disorders begin immediately after the action of provoking factors. First of all this:
- stress provocation;
- intoxication;
- chronic diseases;
- synthetic clothing.
Symptoms
The reason for contacting a dermatologist may be the appearance of clearly defined milky or white spots on certain parts of the body. Most often, the affected area is the face, arms and legs, groin areas and between the buttocks, and scalp.
Sometimes the disease is accompanied by:
- local baldness, hair fading;
- inflammation of the retina;
- scleroderma;
- psoriasis;
- lichen planus;
- chronic diseases of the gastrointestinal tract;
- lack of reaction to cold, heat, external stimuli, dulling of reflexes in affected areas;
- various dermatitis;
- deterioration of the liver (inability to filter toxins).
Procedure protocol
Before starting therapy, all patients participating in the study signed informed consent for the “off label” procedure and permission to publish their photographs in scientific journals.
The course of mesotherapy procedures with NCTF135 consisted of 5 sessions, once a week. Emla cream was previously used as local anesthesia for patients for 30–45 minutes. Then, NCTF135 was administered in a volume of 3.0 ml intradermally, using a papular technique, at a distance of approximately 1.0 cm from each other (Fig. 5). A 30G × 13 mm needle was used for injections. The duration of the procedure was 15–20 minutes (excluding anesthesia time).