Duphalac
Duphalac ®
(lat.
Duphalac
® ) - osmotic laxative drug, prebiotic.
Duphalac is a solution of the active substance
- lactulose in purified water. 100 ml of solution contains 66.7 g of lactulose. The solution has the appearance of a transparent viscous syrup from colorless to light yellow with a brownish tint. Supplied in bottles of 200 ml, 500 ml and 1000 ml or in the form of 15 ml single-use bags made of polyethylene and aluminum foil.
Duphalac has a hyperosmotic laxative effect, stimulates intestinal motility, improves the absorption of phosphates and Ca2+ salts, and promotes the excretion of ammonium ions. The active substance of Duphalac, lactulose, is broken down by colon bacteria into low molecular weight organic acids, which leads to a decrease in acidity and an increase in osmotic pressure and, as a result, an increase in the volume of intestinal contents. These effects stimulate intestinal motility and affect stool consistency. Constipation disappears and the physiological rhythm of bowel movements is restored. In hepatic encephalopathy or hepatic (pre)coma, the effect is attributed to the suppression of proteolytic bacteria by increasing the number of acidophilic bacteria (eg, lactobacilli); the transition of ammonia into ionic form due to acidification of the contents of the colon; bowel emptying due to a decrease in acidity in the colon and the osmotic effect, as well as a decrease in nitrogen-containing toxic substances by stimulating bacteria that utilize ammonia for bacterial protein synthesis. Inhibits the growth of salmonella in the intestines, shortens the period of bacterial excretion (Instructions for use of Duphalac).
Duphalac (lactulose) is the only laxative
an effective and safe drug in all age groups, approved for use in
pediatric practice
. The most important feature of Duphalac is its prebiotic effect. Prebiotics are partially or completely indigestible food components that selectively stimulate the growth and/or metabolism of one or more groups of microorganisms living in the large intestine, ensuring the normal composition of the intestinal microbiocenosis. From a biochemical point of view, this group of nutrients includes polysaccharides and some oligo- and disaccharides. For microorganisms, they are vital components of their nutrition, sources of energy and plastic material. The most well studied prebiotics are dietary fiber, oligosaccharides, lactose and lactulose. As a result of microbial metabolism of prebiotics in the colon, lactic acid, ortho-chain fatty acids, carbon dioxide, hydrogen, and water are formed. Carbon dioxide is largely converted into acetate, hydrogen is absorbed and excreted through the lungs, and organic acids are utilized by the macroorganism, and their importance for humans is difficult to overestimate. Duphalac, by stimulating the growth of normal intestinal microflora, helps maintain anti-infective protection, in particular against Shigella, Salmonella, Yersinia and rotavirus. When artificially feeding children with a milk formula containing 1.2 g/100 Kcal of lactulose with a lactose to protein ratio of 2.5:1, an almost pure culture of bifidobacteria is formed in the intestines, and the acidity of the intestinal contents decreases (Belmer S.V. et al.) .
The dose of Duphalac is selected individually, starting with 5 ml once a day. If there is no effect, the dose is gradually increased (by 5 ml every 3-4 days) until the desired effect is obtained. Conventionally, the maximum dose in children under 5 years of age is 30 ml per day, in children 6 - 12 years old - 40 - 50 ml per day, in children over 12 years old and adults - 60 ml per day. The frequency of administration can be 1 - 2 (less often 3) times a day. A course of Duphalac is prescribed for 1 - 2 months, and if necessary - for a longer period. Duphalac is discontinued gradually under control of stool frequency and consistency (Belmer S.V. et al.).
Duphalac, due to its unique properties, is rightfully considered the gold standard of laxatives. It, like other osmotic drugs, is capable of retaining water in the intestinal lumen, proportional to the number of its molecules. Lactulose, the active ingredient in Duphalac, is not metabolized or absorbed in the small intestine because brush border enzymes cannot hydrolyze the bond between galactose and fructose molecules, and it reaches the colon virtually unchanged. Here, under the influence of bacterial enzymes, lactulose decomposes to form short-chain fatty acids (lactic, acetic, propionic and butyric). These organic acids may be absorbed or remain in the intestinal lumen. In the latter case, there is an increase in stool acidity. Having pronounced osmotic activity, organic acids stimulate obligate excretion of water throughout the colon, which does not allow the mucous membrane to absorb the products of enzymatic decomposition of lactulose. As a result of the increase in intraluminal pressure caused by water retention and an increase in the volume of chyme, the peristaltic reflex is initiated and coordinated motor activity is stimulated, which leads to an acceleration of intestinal transit. An additional mechanism for stimulating peristalsis is an increase in the volume of intestinal contents due to an increase in the biomass of bifidobacteria and lactobacilli, the growth of which is stimulated by the products of enzymatic hydrolysis of lactulose. This phenomenon develops much later than the main effects, but makes a significant contribution to the development of the general laxative effect. Enzymatic processes lead to the formation of gas (10 g of lactulose - 1 liter of hydrogen and carbon dioxide), most of which is absorbed into the bloodstream and released with exhaled air. In some patients, the remaining gas may cause bloating. Flatulence is practically the only side effect of Duphalac. In some patients, it can develop 3-4 days after starting to take Duphalac and, as a rule, goes away on its own. In persistent cases, the dose of Duphalac should be reduced to eliminate flatulence. In order to prevent the development of flatulence, it is possible to recommend a gradual increase in the dose of Duphalac from the minimum to the most effective. It should also be remembered that exceeding the daily dose of Duphalac (more than 100 g of lactulose) can lead to severe diarrhea. Standard doses of Duphalac have a mild laxative effect due to lower, compared to other laxatives of this class, osmotic activity and suppression of water reabsorption in the colon (Pasechnikov V.D.). Due to the ability to bind water, the active substance of Duphalac, the synthetic disaccharide lactulose, like other osmotic laxatives, increases the weight of stool, softens the consistency and accelerates the movement of chyme through the colon. However, Duphalac induces gas formation and bloating.
.
Moreover, the intestinal microflora adapts to the daily intake of non-absorbable sugars. This circumstance reduces the effectiveness of Duphalac during long-term treatment and also forces one to constantly increase its dose
to achieve an effect (Makhov V.M., Beresneva L.A.).
If functional constipation occurs in children in the first year of life who are breastfed, it is necessary (for children from 4 months of age) to introduce complementary foods with a high content of dietary fiber. If there is no effect from the dietary correction, it must be combined with drug therapy - lactulose preparations (Duphalak, Normaze, Lactusan, etc.) (Sorvacheva T.N., Pashkevich V.V.).
For patients suffering from chronic liver diseases of any etiology, in order to correct hemodynamic disorders of portohepatic blood flow, provide a hepatoprotective effect, prevent and correct hepatic encephalopathy, long-term, at least six months, maintenance therapy is recommended, including Essentiale N 6 capsules per day, Duphalac 30-50 ml 3 times a day, and propranol or enalapril 10 mg per day or losartan 50 mg per day (Nikushkina I.N.).
About the use of Duphalac before colonoscopy, anorectal and colonic manometry, X-ray diagnostics and surgical interventions on the colon, see: “Preparation of the colon for instrumental studies.”
Professional medical publications concerning the use of Duphalac in the treatment of gastrointestinal diseases:
- Belmer S.V., Gasilina T.V., Khavkin A.I., Eiberman A.S. Functional disorders of the digestive system in children. M., RGMU, 2005.- 36 p.
- Makhov V.M., Beresneva L.A. Systemic factors in chronic constipation // Attending physician. – 2005. – No. 2.
- Pasechnikov V.D. Functional constipation caused by slow transit of intestinal contents // Farmateka. – 2003. – No. 10. – p. 16–23.
- Sorvacheva T.N., Pashkevich V.V. Functional disorders of the gastrointestinal tract in infants: methods of correction // Attending physician. – 2006. – No. 4. – p. 40–46.
- Nikushkina I.N. The state of portal-hepatic blood flow in chronic diffuse liver diseases (interorgan and hemodynamic relationships). Abstract of dissertation. Doctor of Medical Sciences, 14.00.05 - internal diseases. MGMSU, Moscow, 2007.\
On the website gastroscan.ru in the literature catalog there is a section “Laxatives”, containing medical articles relating to laxatives and their use.
Indications for use of Duphalac
:
- constipation: regulation of the physiological rhythm of bowel movements
- softening of stool for medical purposes: presence of hemorrhoids, upcoming surgery on the colon or anus
- hepatic encephalopathy: treatment and prevention of hepatic coma or precoma
- dysbacteriosis
- enteritis caused by salmonella or shigella
- salmonellosis in the stage of bacterial carriage
- in young children - putrefactive dyspepsia syndrome as a consequence of acute food poisoning
Doses of Duphalac for the treatment of constipation and for softening stools:
- adults: initial dose 15 - 45 ml (maintenance dose 10 - 25 ml)
- children 7-14 years old: 15 ml (10 ml)
- children 3-6 years old: 5 - 10 ml (5 - 10 ml)
- children under 3 years: 5 ml (5 ml)
Duphalac is best taken once a day in the morning with meals.
The clinical effect occurs within 1-2 days. The dose can be reduced after two days of use depending on the patient's needs. The dose or frequency of administration is increased if no improvement in the patient’s condition is observed within two days of taking the drug. Doses of Duphalac in the treatment of hepatic coma and precoma
. Initial dose 3 times a day, 30-45 ml. Then they switch to an individually selected maintenance dose, so that the stool is soft 2-3 times a day maximum, so that the acidity of the stool is within the range of 5.0-5.5 pH. In acute cases, Duphalac can be prescribed in the form of enemas in a ratio of 300 ml of Duphalac and 700 ml of water.
Doses for the treatment of intestinal dysbiosis
(prebiotic course):
- children under 1 year 1.5 - 3 ml
- children from 1 year to 3 years – 3 ml
- children from 4 to 7 years old - 5 ml
- children over 7 years old and adults - 10 ml
The minimum duration of the prebiotic course is 1 month with the possible continuous use of Duphalac in the same doses.
Doses for the treatment of salmonellosis, shigellosis
: in the first 10-12 days, 15 ml 3 times a day, after a one-week break at the same dose 5 times a day.
Contraindications
- galactosemia
- intestinal obstruction
- hypersensitivity to lactulose, fructose, galactose or lactose.
Duphalac should be used with caution
in patients with diabetes mellitus.
Duphalac can be prescribed to pregnant and nursing mothers
.
Side effect:
- in the first days of taking Duphalac, flatulence is possible, which usually goes away after two days
- in case of overdose, abdominal pain and diarrhea may occur, which requires a dose reduction
- when using high doses for a long time in the treatment of hepatic encephalopathy, the patient may develop electrolyte imbalance due to diarrhea
- possible flatulence, abdominal pain, nausea, vomiting, and when using high doses - diarrhea
- possible electrolyte imbalance as a consequence of diarrhea
Overdose
may cause abdominal pain and diarrhea. In this case, it will be enough to reduce the dose or stop taking the drug.
Interaction with other drugs
: Due to the mechanism of action of lactulose by increasing colonic acidity, drugs that have a release dependent on colonic acidity (such as 5-aminosalicylic acid preparations) may be inactivated.
special instructions
- If there is no therapeutic effect within two days or if constipation returns after treatment, you should consult your doctor.
- For patients with lactose intolerance, when using this drug, it is necessary to take into account the lactose content in the drug (for 15 ml of syrup, Duphalac contains up to 1.5 g of galactose and up to 0.9 g of lactose).
- the dose typically used for constipation should not pose a problem for patients with diabetes. The dose used in the treatment of hepatic (pre)coma is usually much higher and therefore must be adjusted when prescribed to patients with diabetes mellitus.
- When treated for more than 6 months with increased doses of Duphalac, the level of electrolytes in the blood plasma should be regularly monitored.
- Duphalac therapy does not have or has an insignificant effect on the ability to drive a car and operate machinery (Instructions for use of Duphalac).
Duphalac is an over-the-counter product.
Duphalac is approved for use by official bodies of Russia, Kazakhstan and some other CIS countries.
According to the pharmacological index, Duphalac belongs to the group «
Laxatives." For ATC - to the group “Osmotic laxatives”, code A06AD11.
Manufacturer:
Solvay Pharma, Netherlands.
Other drug brands
with the active substance
lactulose: lactulose poly, lizalak, normase, portlac, romphalac. Back to section
Duphalac in the treatment of constipation in elderly patients suffering from cardiovascular diseases
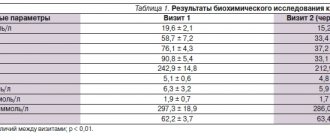
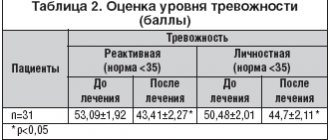
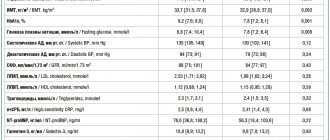
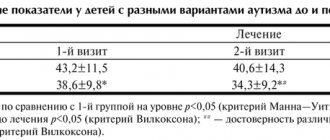
Among the main mechanisms of constipation in the elderly, a decrease in blood supply to the pelvis due to physical inactivity, weakening of the muscles of the anterior abdominal wall and diaphragm, progressive weakness of the pelvic floor muscles due to hypoxia and impaired tissue repair, atrophic denervation of the anal sphincter and puborectal muscles, decreased sensitivity of the anal sphincter, predominate. violation of VIPergic and serotonic regulation [2,3]. In addition, taking many medications for various chronic diseases that affect older patients can also worsen constipation and reduce the effectiveness of medications used to treat it. Hospitalization of patients due to the worsening of cardiovascular diseases most often requires a decrease in physical activity and relative physical inactivity, and also makes it necessary to intensify drug treatment (possibly increasing the doses and number of medications taken). Drugs that can aggravate constipation include drugs actively used in cardiac practice, such as b-blockers, calcium antagonists, centrally acting antiadrenergic drugs, angiotensin II receptor blockers, angiotensin-converting enzyme inhibitors, diuretics, etc. Many causative factors cause constipation is reflected in a wide variety of non-drug and drug treatments. Recommendations from gastroenterologists to change lifestyle and increase fluid and fiber intake are mainly theoretical, since most patients simply act in order to regulate bowel movements - use over-the-counter laxatives. In this case, they are usually guided by affordability and an indication of the herbal origin of the medicine. In the vast majority of cases, the drugs used independently by elderly patients are stimulant laxatives, which, contrary to official recommendations for their use, are usually used by patients frequently or constantly. But this group of laxatives, both of plant origin (based on alkaloids of hay, buckthorn, rhubarb, aloe), and of a synthetic nature, with long-term use, requires an increase in dose due to the rapid development of the addictive effect, and especially in elderly patients it is dangerous due to the potential for the development of serious side effects. effects. In elderly patients, with repeated use of laxatives that stimulate intestinal functions (motor and secretory), as a result of significant loss of salts, weakness may increase, coordination of movements may be impaired, dizziness, orthostatic hypotension and arrhythmia may develop. Sena-based laxatives stimulate excessive loss of potassium through the intestines, and this must also be taken into account when prescribing potassium-sparing diuretics. It can also be said that elderly patients are not shown laxatives, the laxative effect of which is associated with an increase in the volume of intestinal contents (methylcellulose, polycarbophil). The use of laxatives in this group can reduce the expected effect of anticoagulants, cardiac glycosides, and antibiotics. Laxatives that lubricate the intestinal mucosa (vaseline oil), disrupting the processes of normal absorption of medications, significantly reduce their effectiveness. In this regard, for elderly patients suffering from cardiovascular diseases, especially during hospitalization, the choice of an effective and safest drug for the treatment of constipation becomes relevant. Along with its effectiveness, this drug must be combined and not reduce the activity of other medications taken by the patient. The principal effect of the drug Duphalac is due to the fact that its active substance lactulose, entering the colon intact, is biotransformed in it to short-chain fatty acids, as a result of which the intestinal contents are acidified and the osmotic pressure in the colon increases [4,5] . The purpose of our study was to study the effectiveness of Duphalac therapy in elderly patients with chronic constipation undergoing hospital treatment for cardiovascular diseases. Material and methods The study included 32 patients over 65 years of age (15 men and 17 women, average age 72.8±1.5 years) hospitalized at the City Clinical Hospital named after. S.P. Botkin regarding exacerbation of various cardiovascular diseases. Table 1 presents a list of diseases that caused hospitalization of the examined patients. Due to the inclusion of elderly patients in the study, most of them had concomitant pathology. All patients in the hospital were selected for drug therapy aimed at improving prognosis, quality of life and eliminating symptoms of the disease. The main groups of medications used in the examined patients are presented in Table 2. The study included patients with diagnostic criteria for functional constipation (according to the Rome II consensus). The criteria for functional constipation noted in the examined patients are presented in Table 3. Accordingly, the severity of chronic constipation was assessed on an 8-point scale. The patients were divided into two groups: – with severe constipation (8 points) – 18 people, – with moderate constipation (5–7 points) – 14 people. Concomitant gastroenterological diseases that some patients had were in remission and did not aggravate constipation. For the treatment of functional constipation, patients were prescribed lactulose (Duphalac, pharmaceutical company Solvay Pharma) in initial doses of 20–40 ml depending on the severity of constipation: – for severe constipation – 20–40 ml (average dose 34.7 ± 1.7 ml ), – for moderate constipation – 20–30 ml (average dose 24.3±1.4 ml). Almost all patients took the entire dose at one time during breakfast. The effectiveness of the drug was assessed on an 8-point scale on the 3rd and 14th days of treatment, as well as its safety. At the same time, if necessary, the dose of the drug was adjusted. In addition, all patients were monitored for hemodynamic parameters (BP, pulse), ECG, and biochemical blood parameters initially, as well as on the 3rd and 14th days of therapy. Statistical processing of data with reliability assessment using Student's t test was carried out using the Biostatistics program (version 4.03). Results of the study The study showed that in the majority of patients on the 3rd day of Duphalac therapy using an initial average dose of 30.2 ± 1.5 ml (for patients with severe constipation - 34.7 ± 1.7 ml, with moderate constipation – 24.3±1.4 ml) the manifestations of chronic constipation significantly (p<0.001) decreased (from 7.4±0.1 to 1.0±0.3 points) (Table 4). At the same time, 9 (29%) patients (including 7 people with severe constipation) still had a feeling of incomplete bowel movement, 6 (19.4%) patients (including 5 people with severe constipation) had a feeling of obstruction in the anorectal area, in 2 (6.5%) patients (all with severe constipation) straining for more than 1/4 of the time of bowel movement, 1 person (3.2%) (with severe constipation) continued to require manual bowel emptying. Moreover, 4 (12.9%) subjects (all with severe constipation) did not have bowel movement on the 3rd day of observation. On the other hand, 9 (29%) patients (6 of them with severe constipation) noted rapid bowel movements (within 2–4 hours), 2–3 times per day, and mushy stools. Considering the results obtained, from the 4th day of the study in 10 (32.3%) patients, due to insufficient effect, the daily dose of Duphalac was increased, and in 9 (29%) patients it was reduced and was divided into groups: in persons with severe constipation 15–60 ml (average 36.2±3.1 ml), in persons with moderate constipation 10–40 ml (average 25.4±2.4 ml). On the 14th day of Duphalac therapy, almost all symptoms of chronic constipation disappeared in 30 (96.8%) patients (p<0.001). Only 1 patient (3.2%) with severe constipation maintained a frequency of bowel movements less than 3 times a week and a feeling of obstruction in the anorectal area. The same patient and 2 other patients with severe constipation (9.7% in total) still had a feeling of incomplete bowel movement, and therefore they were recommended to subsequently increase the dose of the drug to achieve a greater osmotic effect. A comparative analysis of the presence of criteria for chronic constipation in the examined patients on the 3rd and 14th days of Duphalac therapy did not reveal significant differences, which makes it possible to select the dose of the drug already in the first 2-3 days from the start of treatment. A decrease in the manifestations of constipation in the examined patients was accompanied by an improvement in the clinical course of the underlying disease. During the observation period, all patients showed positive dynamics of hemodynamic parameters, increased tolerance to physical activity, and improved general well-being. None of the patients had statistically significant deviations from the initial biochemical blood parameters (liver enzymes, lipids, glucose, electrolytes, urea, creatinine). The drug was generally well tolerated by elderly patients. In 7 (21.9%) patients who received an average of 26.3±3.8 ml of Duphalac, transient flatulence was observed in the first 2 days of administration, in 4 (12.5%) of them it was accompanied by mild abdominal pain that disappeared in the next few days. 2–3 days alone or against the background of small doses of myotropic antispasmodics. The use of antispasmodics (especially mebeverine) in these patients and/or the recommendation to pre-dissolve the drug in water made it possible to avoid discontinuation of the drug and improve its tolerability. Despite this, 1 patient (3.1%) with severe constipation independently stopped taking the drug on the 2nd day. The data obtained in our study are consistent with the results of previous studies of lactulose in geriatric patients [4,5]. Conclusions 1. Duphalac is effective and safe in the treatment of chronic constipation in elderly patients hospitalized for cardiovascular diseases. 2. Selection of the laxative dose is carried out individually and is possible in the first 2–3 days. The optimal initial dose is 20–40 ml of the drug. 3. Duphalac is metabolically neutral and does not worsen the main biochemical parameters of the blood.
References 1. Barret JA Faecal incontinence & constipation in the elderly. – Falk symposium, No. 95, 1996, p. 211–225. 2. Diarrhoea & constipation in geriatric practice. – Ed. Ratnaike RN – Cambridge University press, 1999. 3. Constipation. – Ed. Kamm MA, Lennard–Jones JE – Wrighston Biomedical Publishing LTD, USA, 1994. 4. Kr?ger M., Schumann C: Lactulose treatment of constipation in the elderly (Publication in Verbereitung. Data on file, Solvay Arzneimittel 1994, Report number H. 105.904G). 5. Sanders JF Lactulose syrup assessed in a double–blind study of elderly constipated patients. – J. Am. Gereat. Soc. 1978; 26, 236–239.
Normal microflora of the gastrointestinal tract and its functions
Normal human microflora is considered as a collection of many microbiocenoses that occupy numerous ecological niches (biotopes) on the skin and mucous membranes of all body cavities communicating with the external environment [3, 7]. The total number of microorganisms in the adult human body reaches 1015, which is more than 10 times the number of host cells [2]. There is no longer any doubt that the normal human microflora performs numerous functions to maintain homeostasis [1, 3, 7, 15, 19]. In this sense, the importance of microflora for humans is no less than the importance of any vital organ. The huge biomass, combined with the importance of its functions, allows us to consider the microflora as an independent organ [7]. More than 400 species of bacteria, representatives of 17 different families, live in the gastrointestinal tract (GIT) alone [3, 7]. The species and quantitative composition of microbial populations in different biotopes of the gastrointestinal tract is heterogeneous, but each biotope is an ecosystem, all components of which (macroorganism + microflora) perform mutually beneficial functions and are in a state of symbiosis, maintaining dynamic balance in this system.
Violation of the species and quantitative composition of microorganism populations and the growth of opportunistic microflora, leading to an imbalance in a given biotope, is called dysbacteriosis. The process may not end there, however. A change in the biocenosis in one biotope entails the movement of microorganisms into uncharacteristic biotopes and a decrease in colonization resistance of both individual biotopes and the entire human-microflora ecosystem. A manifestation of such microflora translocation can be excessive growth of bacteria in the small intestine, for example, with blind loop syndrome. Different biotopes of the gastrointestinal tract are unevenly populated by bacteria (see table).
The density of microflora is highest in the large intestine. About 400 species of microorganisms with a total biomass of about 1.5 kg live here [7]. Due to such a high population of microflora, the large intestine bears the greatest functional load compared to other biotopes of the gastrointestinal tract.
The main (resident) microflora of the colon consists of 90% bifidobacteria, bacteroides and lactobacilli. These bacteria are anaerobes. Resident microflora also include enterococcus and propionobacteria, but their share in the total microbial biomass is small [3]. The accompanying (facultative) microflora is represented mainly by aerobes: Escherichia, eubacteria, fusobacteria, cocci, a total of about 10%. Less than 1% accounts for numerous representatives of residual microflora, including aerobes and anaerobes. Thus, 90% of the colon microflora are anaerobes [1, 3].
Based on the nature of their metabolism, colon bacteria are divided into two groups: proteolytic and saccharolytic. Proteolytic species (bacteroides, proteas, Escherichia, clostridia, etc.) use the products of intestinal hydrolysis of proteins as a nutrient substrate and, as a result of their metabolism, form toxic substances, including aromatic amino acids, endogenous carcinogens, and sulfides. These substances contribute to the development of diarrhea, inflammation, and neoplasms. Most proteolytic microorganisms are opportunistic.
Saccharolytic flora (bifidobacteria, lactobacilli, some cocci, propionobacteria) use carbohydrate substrates entering the large intestine and polysaccharides of intestinal mucus. The metabolic functions performed by saccharolytic microbes are beneficial for the host organism, maintain homeostasis and neutralize the negative effects of proteolytic microflora.
The bulk of bacteria in the colon are bifidobacteria and lactobacilli. The dominance of these bacteria determines their greatest importance for humans. The beneficial functions of normal gastrointestinal microflora can be divided into 3 main groups: a) metabolic, b) protective and immune, c) antimutagenic and anticarcinogenic.
The metabolic functions of microflora are aimed at maintaining the optimal level of metabolic processes, digestive and motor functions of the gastrointestinal tract and include increased activity of gastrointestinal enzymes, regulation of lipid (cholesterol) levels, participation in the conjugation and recycling of bile acids, as well as the synthesis of:
- amino acids (arginine, tryptophan, tyrosine, cysteine, etc.);
- vitamins (groups B and K);
- short-chain fatty acids (SCFA), including acetic, butyric, lactic, propionic;
- biogenic amines (histamine, serotonin, piperidine, GABA);
- hormonally active substances (norepinephrine, steroids);
- antioxidants (vitamin E, glutathione).
The protective and immune functions of microflora are aimed at maintaining colonization resistance and antagonism towards pathogenic and opportunistic microorganisms. This is ensured by the antitoxic and sorption effects of microflora, as well as by the synthesis of:
- KZHK;
- other organic acids that regulate pH in the intestinal cavity;
- lysozyme (muramidase), hydrogen peroxide and antibiotic-like peptides-microcins, which have a wide spectrum of antibacterial activity and constitute a group of “natural” antibiotics [2, 3];
- secretory IgA in the human body.
In recent years, the immunomodulatory properties of normal intestinal microflora have been well studied. Bifidobacteria and lactobacilli affect various parts of the immune system, regulating nonspecific and specific cellular and humoral immunity, inducing the synthesis of immunoglobulins, lysozyme, interferon [3, 4, 17, 18].
The antimutagenic and anticarcinogenic activity of microflora is realized through the hydrolysis of metabolic products of proteins, lipids, carbohydrates, deconjugation of bile and hydroxylation of fatty acids, inactivation of histamine, xenobiotics and carcinogens. SCFAs also participate in the implementation of the anticarcinogenic potential of microflora.
The role of SCFA in the regulation of intestinal microbiocenoses and maintaining body homeostasis
A special role among microbial metabolites is played by SCFAs with a carbon chain length of 2 to 4 atoms (acetic, oily, lactic, propionic). SCFAs are the end products of metabolism of saccharolytic and proteolytic microflora and are used for an integral assessment of its condition [1]. The breakdown of SCFA produces a lot of energy, so they serve as an additional autonomous source of energy for the intestinal epithelium. Propionic acid regulates microcirculation in the mucous membrane and supports trophic processes in it, participates in gluconeogenesis and the synthesis of biogenic amines, and blocks the adhesion of pathogens. Butyric acid is an important regulator of proliferation and differentiation of the colon epithelium and thus determines the anticarcinogenic activity of microflora. Acetic acid provides an antimicrobial effect, regulates pH in the intestinal cavity and gastrointestinal motility. Lactic acid is involved mainly in the regulation of pH and local immunity and in lipogenesis. The lipid-lowering effect of microflora and vasoactive influences are provided by the metabolic effects of SCFA. Maintaining the pool of SCFAs in the colon by restoring normal microflora or through additional substrates for the formation of SCFAs (dietary fiber, oligosaccharides) is necessary for the normal functioning of the macroorganism, the prevention of atherosclerosis, colorectal cancer [14, 15].
Ways to correct microflora disorders
The species and quantitative composition of microflora and its functions can be disrupted under the influence of many exogenous and endogenous factors: natural and man-made toxins, medications (antibiotics, laxatives, sorbents, steroids, psychotropic drugs), stress. A huge negative role is played by the widespread use of diets for weight loss and the abuse of so-called methods of cleansing the body of toxins. Almost all chronic diseases of the gastrointestinal tract can lead to an imbalance of microflora due to a weakening of the protective properties of the mucous membranes.
Microflora disturbances are always secondary, so to correct them it is necessary, first of all, to eliminate the causes that cause them or to treat the underlying disease. If these measures are not enough, then three groups of agents with different mechanisms of action are used to restore the microflora: probiotics, prebiotics and synbiotics.
Probiotics are food products, medicines or dietary supplements in the form of monocultures or combined cultures based on living representatives of resident microflora (bifidobacteria, lactobacilli, enterococci) or non-pathogenic spore-forming microorganisms and saccharomycetes. Examples of probiotics: Baktisubtil ( B. cereus ), Sporobacterin (B. subtilis), Enterol.
Prebiotics are natural or synthetic agents of non-microbial origin. These are medicines, food products and dietary supplements that selectively stimulate the growth and/or metabolic activity of one or more types of microflora [12, 14]. Prebiotics are not absorbed in the small intestine and undergo bacterial fermentation in the colon. Most prebiotics are oligo- or polysaccharides (fiber). Oligosaccharides, in turn, can be natural (fructozooligosaccharide - inulin and galactoseoligosaccharide - lactitol) and synthetic (lactulose; drug - Duphalac). Prebiotics also include lysozyme, para-aminomethylbenzoic acid and calcium pantothenate.
Synbiotics are an optimal combination of probiotics and prebiotics. Synbiotics include Biovestin-lacto (B. bifidum, B. adolescentis, L. plantarum and bifidogenic factors), Maltodophilus (B. bifidum, L. acidiphilus, L. bulgaricus and maltodextrin), Bifido-bak (a complex of lactobacilli and bifidobacteria and fructose-oligosaccharides from Jerusalem artichoke), Laminolact (E. faecium L-3, amino acids, pectins, sea kale).
A separate group of drugs consists of microbial metabolites, such as Hilak forte.
Lactulose
The main group of prebiotics consists of oligosaccharides with 2–10 carbon atoms. Oligosaccharides are not hydrolyzed or absorbed in the small intestine because there are no enzymes in the brush border to break them down. Unchanged, they enter the large intestine, where they undergo bacterial fermentation. This group of prebiotics includes Duphalac (lactulose), a synthetic disaccharide consisting of fructose and galactose. Lactulose realizes its effect only in the large intestine. It is hydrolyzed mainly by bifidobacteria (to a lesser extent by lactobacilli), for which lactulose serves as a nutrient substrate, which leads to an increase in their biomass. Thus, this disaccharide is a bifido- and lactogenic prebiotic that normalizes the balance and restores the functions of microflora [12, 14, 15]. The end products of lactulose metabolism are formic acid and SCFA. Antagonism of bifidobacteria and lactobacilli and a decrease in pH in the intestinal cavity due to acidic metabolites leads to suppression of the growth of opportunistic proteolytic microflora. In addition to other biological effects (hypolipidemic, antiproliferative), SCFAs have an osmotic effect. The increase in microflora biomass and the osmotic effect of SCFA lead to an increase in stool volume, stimulation of motility and a corresponding laxative effect. Thus, lactulose combines the properties of a prebiotic and a mild osmotic laxative. These unique features can be successfully used for constipation of various origins, accompanied by microflora disorders. Thanks to the synthesis of SCFA and, above all, butyric acid, lactulose has an antiproliferative potential, which is realized in patients with constipation when taking the drug systematically.
The effect of lactulose on the growth of microorganisms in the colon in adult healthy volunteers was studied in a double-blind, controlled study using two methods: the traditional method of culturing intestinal microflora on selective media and the in situ hybridization method [20]. The use of molecular genetic analysis made it possible to assess the dynamics of both cultivated and uncultivated bacterial strains. To stimulate microbial growth, Duphalac was used at a dose of 10 g/day for a month. Microbiological examination of stool was carried out before the start of treatment, immediately after the end of taking the drug and 4 weeks after the end of its use. When cultivated on selective media, a significant increase in the growth of bifidobacteria, lactobacilli, enterococci, coliforms and an increase in the total number of aerobic bacteria was found in the group of subjects taking Duphalac. In a molecular genetic study, significant differences were identified only in relation to the growth of bifidobacteria. Thus, an increase in the growth of bifidobacteria when taking Duphalac was proven by two methods. The effect was more pronounced with an initially low content of bifidobacteria in the feces. Under the influence of treatment, there was a tendency towards a decrease in the number of clostridia.
Increased growth of bifidobacteria under the influence of lactulose was also proven in a 6-week study conducted by Bouchnic Y. [11]. Another test on healthy volunteers showed that when taking lactulose, the population density of bifidobacteria increases by 1.5 times compared to the initial level, and the population density of clostridia decreases in parallel by almost 3 times [10]. In the same study, when comparing the prebiotic effects of lactitol and lactulose, the advantage of the latter in stimulating the growth and enzymatic activity of bifidobacteria was shown [10].
The huge advantage of lactulose over probiotics is the possibility of its use together with antibacterial drugs in patients who need repeated courses of antibiotic therapy for other diseases (chronic nonspecific lung diseases, chronic pyelonephritis, etc.). In these cases, the prebiotic effect of lactulose is realized not only as a restorer in relation to the disturbed microbiocenosis of the colon, but also as a preventative, preventing the suppression of normal microflora. The effectiveness of probiotics in such cases is very low, which is quite natural, since the live strains of bacteria included in their composition are also negatively affected by antibiotics.
Lactulose also exhibits a preventive effect in the antibiotic therapy of intestinal infections. Moreover, it has been established that lactulose has an indirect antimicrobial effect due to the restoration of bifido- and lactobacilli and their antagonism against pathogens of intestinal infections. Thus, it has been shown that Duphalac, by stimulating the growth of bifidobacteria, leads to a decrease in pH in the colon by more than 2 times (due to acidic metabolites of normal microflora) and thereby inhibits the growth of salmonella, shigella and fungi of the genus Candida [6]. Lactulose suppresses the excretion of Salmonella, Shigella and Yersinia in feces during corresponding infections [9, 13, 16].
Recent studies have demonstrated disruption of the colon microflora in patients with hematologic malignancies during high-dose chemotherapy. The use of Duphalac led to an improvement in the microbial and metabolic status of the intestine. At the same time, the ratio of anaerobic and aerobic microflora was restored, as evidenced by the normalization of SCFA profiles in feces [5].
It is well known that normal microflora is involved in maintaining immunity. From the first days of life, intestinal microflora participates in the formation of the immune system [18]. On the contrary, disruption of the microbiocenosis of the gastrointestinal tract leads to perverted immune reactions, reduces the body’s resistance to viral and bacterial infections (not only intestinal), contributes to the development of atopic diseases, allergic dermatitis, neurodermatitis [3, 8, 17, 18].
Lactulose has been shown to restore cellular and humoral immunity [4]. As it turned out, its 2-week intake leads to a significant increase or complete normalization of the levels of IgA, T-helpers and T-suppressors in different categories of patients.
The powerful stimulating effect of lactulose on bacterial growth and metabolism has been successfully used in the treatment of hepatic encephalopathy. Reproducing acidophilus bacteria suppress the growth of proteolytic flora and absorb the ammonia and other nitrogen-containing toxins it produces, using them for protein synthesis [3]. Other prebiotics (including inulin and lactitol) have not found use in hepatic encephalopathy, apparently due to an insufficient stimulating effect on microbial growth.
Since Duphalac has the properties of a prebiotic and osmotic laxative, the choice of dose of the drug depends on the disease and the purpose for which it is used. Treatment of hepatic encephalopathy requires a high dose, which is 60–100 ml/day (Duphalac release form is syrup), which corresponds to approximately 40–70 g of lactulose. To achieve a laxative effect, the dose is on average 15–40 ml/day (may be higher in the elderly). The dose of Duphalac as a prebiotic is lower than laxative and is selected in such a way as not to change the frequency of bowel movements. Most studies of the prebiotic effect of lactulose used a dose of no more than 10 g/day [10, 20]. The recommended dose of Duphalac (3, 5 or 10 ml/day) is selected individually. The correct selection of the dose ensures that only the prebiotic or complex prebiotic and laxative effect of Duphalac is manifested, which allows it to be used for various purposes both for constipation and diarrhea caused by a violation of the microflora of the colon.