How does Forlax work?
Forlax 4g contains macrogol 4000, an osmotic laxative also known as polyethylene glycol (PEG).
Macrogol 4000 retains water in stool. It softens hard stools and increases their volume. This speeds up the transit of intestinal contents, facilitates bowel movements and gives a natural feeling of relief. Macrogol 4000 is not absorbed by the body and is excreted unchanged.
What else is important to know: laxatives
Forlax in the treatment of chronic constipation: features of therapy for elderly patients
Minushkin O.N., Elizavetina G.A.
Constipation is a widespread condition that has by no means lost its significance today. A single daily bowel movement is not strictly a sign of normal bowel function. The frequency of stool in healthy people varies widely and depends on the nature of nutrition, lifestyle, and habits. In order to standardize concepts, an international definition of functional constipation was prepared by a group of international experts in accordance with the Rome II criteria (1999). Functional constipation (category C3) refers to a group of functional disorders manifested by “... persistent, difficult, infrequent or seemingly incomplete bowel movements.”
According to the Rome Consensus II, diagnostic criteria for functional constipation (C3) include the presence of two or more symptoms that have existed for at least 12 weeks, but which do not necessarily have to be consistent over the past 12 months:
- less than 3 bowel movements per week;
- difficulty with > 1/4 bowel movements;
- bloating or hard stool with > 1/4 bowel movements;
- feeling of incomplete evacuation with > 1/4 bowel movements;
- feeling of anorectal obstruction (blockage) at > 1/4;
- manual assistance in performing > 1/4 of bowel movements (“digital” evacuation, pelvic floor support, etc.).
Thus, defecation problems are widespread, burdensome and reduce the quality of life of patients.
Modern ideas about the treatment of constipation are based on special diagnostic methods and careful selection of a therapeutic approach. Unfortunately, laxatives are often prescribed and used without reason. This statement is true both for self-medication and for medical recommendations.
Treatment of constipation should always begin with non-drug methods. These include increasing physical activity, playing sports, normalizing water balance and diet with the obligatory inclusion of dietary fiber.
Adding ballast dietary fiber to the diet (bran, pectin, microcrystalline cellulose, psyllium, various dietary supplements with a high content of soluble and insoluble fiber) is the basis for the treatment of constipation in young patients, but is not always possible in the elderly. Dietary fibers are hydrophilic colloids: in a liquid medium they create stable micelles that significantly increase the volume of intestinal contents and stimulate peristalsis. For the successful action of dietary fiber, a daily volume of liquid of at least 1.5 liters is required, otherwise they act as sorbents, i.e. absorb fluid from the intestines and increase constipation. However, elderly patients cannot always maintain water balance due to heart failure, difficulties moving around the apartment, bed rest, etc., therefore, dietary fiber should be recommended to this category of patients with great caution, monitoring their use. This dictates the need for wider use of laxatives in elderly patients, while for young people they are prescribed only when non-drug methods are ineffective.
Laxatives are also used for drug-induced constipation, when the drugs that cause it cannot be withdrawn (opiates for chronic pain, antidepressants, antiparkinsonian drugs). Short courses of laxatives are recommended in the pre- and postoperative periods, in preparation for intestinal examinations.
Groups of laxatives
Existing laxatives are divided into 3 groups according to their mechanism of action:
- Increasing the volume of intestinal contents:
dietary fiber (bran, microcellulose, seaweed, flax seed, plantain, agar-agar, Mucofalk);
- osmotic:
oligosugars (lactulose, lactitol);
- polyethylene glycol - macrogol 4000 (Forlax);
- alcohols (sorbitol, mannitol, glycerin);
- saline laxatives (magnesium sulfate, Glauber's salt, etc.);
- anthraglycosides (preparations of senna, buckthorn, rhubarb);
- Vaseline and other mineral oils.
Intestinal volume-increasing (bulk) laxatives are products of natural origin or synthetic modified polysaccharides that are difficult to digest or not digested at all, as a result of which they are almost not absorbed. When they absorb water, they swell and cause stretching of the intestinal walls due to their increase in volume. In this way, a propulsive wave is excited and, ultimately, defecation is accelerated by a reflex reaction. Prerequisites for achieving this effect are the preserved ability of the colon to respond to bulk laxatives and swell sufficiently, as well as simultaneous fluid intake (from 1.5 to 2 liters).
Osmotic laxatives (sugars, polyhydric alcohols, salt preparations), despite the common mechanism, differ from each other in their zone of action. Thus, alcohols with a relatively short chain of 3-6 carbon atoms (sorbitol, mannitol, glycerin) and saline laxatives act at the level of the small intestine and contribute to the release of large amounts of fluid into its lumen, which is accompanied by dilution of stool and often provokes diarrhea. Saline laxatives act quickly (within 2-4 hours), but are not suitable for long-term use, as they can cause severe disturbances in water and electrolyte balance.
Oligosugars, primarily the synthetic disaccharide lactulose, are not absorbed in the small intestine, since there are no enzymes there that break them down. The drug acts exclusively in the colon, where lactulose undergoes bacterial fragmentation and hydrolysis to fructose and galactose, mainly under the influence of bifidobacteria and, to a lesser extent, lactobacilli. The end products of lactulose metabolism are volatile fatty acids, which, in addition to hypocholesterolemic, hypolipidemic and antiproliferative effects, have an osmotic effect.
Osmotic processes in the large intestine are less pronounced than in the small intestine, fluid secretion into the intestinal lumen is lower, therefore the laxative effect of lactulose is milder than that of saline laxatives, although it develops just as quickly. The second important mechanism of action of lactulose is an increase in bacterial biomass, which contributes to an increase in fecal volume and stimulates peristalsis. Thus, lactulose has a dual mechanism of action: it restores colonic microbiocenosis, being a bifidogenic and lactogenic prebiotic, and increases the volume of intestinal contents due to osmotic action and stimulation of bacterial growth. However, increasing doses of the drug is accompanied by bloating and distension of the abdomen, which often forces patients to abandon long-term use of lactulose. Therefore, selection of the minimum effective dose is the most important component of working with this drug.
These mechanisms of action determine its therapeutic value, making it one of the most acceptable drugs for the treatment of constipation in elderly patients. An increase in biomass and the formation of volatile fatty acids is also observed when taking dietary fiber. The mechanisms of these phenomena are the same as when using lactulose.
A pronounced osmotic effect is exerted by Forlax (macrogol 4000), a high molecular weight polyethylene glycol, which is effective and safe with long-term use, is not absorbed, is not metabolized, forms hydrogen bonds in the intestinal lumen, thereby increasing the volume of intestinal contents, softening its consistency. Forlax does not develop addiction; the effectiveness of the drug does not depend on the state of the intestinal microflora.
Stimulant laxatives include drugs that promote secretion and local irritants.
All laxatives with secretory action (anthraquinones, diphenylmethane derivatives, castor oil) interact with the epithelial structures of the intestine and cause active secretion of fluid into its lumen, while simultaneously reducing absorption. All these drugs cause short-term, and with long-term use, constant secretory diarrhea, which is characterized by an increase in the flow of fluid and electrolytes into the intestines. It is important to note that the decrease in potassium concentration in the blood associated with their use inevitably leads to smooth muscle relaxation and increased constipation if it is caused by hypotonicity of the intestinal wall. Disruption of fluid homeostasis contributes to the development of secondary hyperaldosteronism, which further increases the loss of potassium, and thus the “vicious circle” closes. This is one of the main mechanisms of addiction and increased constipation with long-term use of all “secretory” laxatives.
The second mechanism of addiction has been proven for anthraquinones and diphenylmethane derivatives. These drugs, acting at the level of neurons of the submucosal plexus, cause the formation of nitric oxide, which relaxes smooth muscles and inhibits peristalsis. With prolonged use, degenerative changes in the enteric system develop. It is assumed that laxatives of these groups also have a mutagenic effect and are genotoxic. Thus, stimulant laxatives are not recommended for long-term, much less chronic, use, especially in elderly patients in whom intestinal hypotension and delayed transit are the main mechanisms of constipation.
Drugs with a local irritant effect can be used in elderly people in the form of suppositories to stimulate the tone of the anal sphincter and improve bowel movements.
Products that soften feces include petroleum jelly, olive, almond and other vegetable oils. The laxative effect of their use develops after 5-6 hours. Softening laxatives are used, as a rule, in cases where a quick effect is needed (for example, in case of poisoning, in the postoperative period, in preparation for a diagnostic examination of the intestine).
Basic rules for prescribing laxatives
When using laxatives, you should always remember the negative side of their use. The negative properties of laxatives are associated with the fact that as the duration of their use increases, the receptor apparatus becomes accustomed, as a result of which the effectiveness of these drugs steadily decreases. After 3 years of regular use of laxatives, it drops to 73%, after 5 years - to 50%, and after 10 years only 11% of patients respond to laxatives. During long-term therapy with stimulant laxatives, atrophic and inflammatory changes in the intestinal mucosa are observed, caused by local irritation and dysbiosis, increased loss of protein and potassium through the intestine, and decreased tone of the intestinal muscles.
With chronic use of laxatives, there is no need to take them daily. It is advisable to prescribe the drugs once every 3-4 days, periodically taking breaks from taking laxatives, and changing laxatives every 2 years.
When choosing laxatives, you should adhere to the following tactics:
- if it is necessary to achieve rapid bowel movements in 2-4 hours, cleansing enemas, saline laxatives, castor oil, Fortrans, contact laxatives in the form of suppositories (bisacodyl) are used;
- if it is necessary to ensure the evacuation of intestinal contents within 24 hours, then stimulant laxatives (anthraquinones, diphenones) are prescribed;
- For long-term use and course treatment, osmotic laxatives are used: Forlax, lactulose with the inclusion of dietary fiber (bran, microcellulose) in the diet.
As mentioned earlier, in the treatment of chronic constipation in the elderly, preference is given to lactulose preparations. However, it should be remembered that in order to reduce the frequency of side effects possible during treatment with drugs of this group, combination therapy is required, which for elderly patients seems burdensome due to other existing pathologies that also require long-term and/or constant drug treatment. Thus, it is urgent to search for drugs no less effective than lactulose for the monotherapy of chronic constipation in the elderly.
We have our own experience in treating patients with functional constipation with the drug Forlax with different methods of prescribing it mainly to elderly patients.
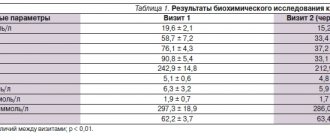
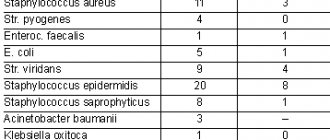
The design of the first study included a course of Forlax administered to 30 patients with functional constipation, i.e. daily use of 2-3 sachets of this drug (10 g of macrogol 4000 in 1 sachet) for 10-12 days.
The age of the patients (three men and 27 women) ranged from 20 to 85 years (average 63.1±2.8 years), the majority of patients were elderly.
Before taking Forlax, only 3 people did not use laxatives, the remaining 27 patients regularly took various laxative medications: stimulants - 25, saline laxatives - 2, rectal suppositories (glycerin) - 3 people; 7 out of 30 people periodically used cleansing enemas.
Forlax was prescribed daily in the morning, 2 sachets (20 g); during treatment, 6 people increased its dose to 3 sachets; 3 patients, on the contrary, reduced the dose to 1 sachet per day.
In 20 (66.7%) patients, daily bowel movements were observed from 2-3 days of taking Forlax. The stool was of a soft consistency, and patients felt a complete bowel movement. The laxative effect of Forlax was not accompanied by abdominal pain and painful tenesmus. In 5 (17%) people, while taking Forlax, daily stool was noted in the first 6-7 days, and then, due to the absence of stool for more than 2 days, patients added other laxatives. In another 5 (17%) patients, the use of Forlax was assessed as ineffective, since throughout the entire period of treatment with the use of 3 sachets of the drug, bowel movement was achieved only with the addition of laxatives with a different mechanism of action or with the help of cleansing enemas.
Over the next week, bowel movements without Forlax use were assessed. 12 (40%) of 30 patients had an aftereffect, i.e. Spontaneous bowel movements continued daily or every other day. Another 12 people were forced to resort to previously used laxatives 1-2 times a week, but in a significantly lower dosage than before using Forlax. In 6 (20%) patients, bowel movements returned to baseline.
Forlax did not cause side effects, the drug was well tolerated.
Thus, a positive effect during treatment with Forlax was observed in 83% of patients. The mild and long-lasting effect of the drug, its good tolerability, and acceleration of intestinal motor function were noted. Forlax had an aftereffect in 40% of patients; in addition, it enhanced the effects of previously used laxatives with a different mechanism of action, apparently by restoring the sensitivity of the intestinal mucosal receptors to them.
The design of the second study was to evaluate the effect of Forlax when used “as needed” with the goal of providing stool at least 3 times a week.
The objectives of the study also included determining the minimum and maximum doses of the drug used as maintenance therapy, as well as assessing the aftereffect of Forlax over the next 2 weeks without its use.
The study included patients with chronic functional constipation, long-term and, in most cases, long-term use of various laxatives.
32 patients were under observation: 6 men and 26 women. The age of the patients ranged from 46 to 80 years (mean 64.6±3.4 years). The majority of patients were elderly.
According to the method of taking the drug, patients were divided into two groups. The first group (22 people) started taking Forlax 2 sachets in the morning on an empty stomach, 17 of them took the drug after 2-3 days, and 5 patients with persistent constipation in the first 3-4 days received Forlax 2 sachets daily due to slowly developing effect. During treatment, 7 patients on days 6-8 increased the dose of Forlax to 4 sachets per day due to the absence of stool for more than 2 days and the appearance of bloating. Four patients, from the 2-3rd day of taking the drug, reduced its dose to 1 sachet after 2 days with the effect of daily emptying. As a result, 19 patients achieved a positive effect. Bowel movement, as a rule, occurred 24-30 hours after taking Forlax. The stools were of soft consistency (formed and/or semi-formed).
The second group - 10 elderly patients with long-term persistent constipation - began taking Forlax with 4 sachets every 2 days. In 3 patients, no effect was achieved; in the remaining 7 people, fairly complete bowel movements were observed daily or every other day.
Thus, during treatment with Forlax, a positive effect was obtained in 26 (81.3%) patients. A slight laxative effect of the drug was noted (the stool was semi-formed and formed). The use of Forlax once every 2-3 days in most cases ensured fairly complete emptying of the stomach every day or every other day. The dose of the drug was selected individually, taking into account the duration of constipation. In the majority of patients (62.5%), the effective dose of Forlax was 2 sachets taken every 2 days. In 18.8% of patients with refractory constipation, Forlax was effective at a dose of 4 sachets (also after 2 days).
In 6 (18.7%) of 32 patients, the use of Forlax was assessed as ineffective. While taking 4-5 sachets daily for 3-4 days, bowel movement did not occur, and on days 3-4 these patients underwent cleansing enemas or switched to using laxatives from other groups. As a rule, these were patients who had been taking stimulant laxatives, mainly from the anthraquinone group, for many years. Apparently, in these patients, the restructuring of intestinal activity due to the transfer to an osmotic laxative takes a long time, and the use of Forlax should be longer.
After discontinuation of Forlax, the aftereffect for 5-14 days was observed in 47% of patients.
The results of the study showed that Forlax can be successfully used as monotherapy “as needed” in the treatment of chronic functional constipation at any age, and especially in elderly patients. In each specific case, the dose and route of administration of the drug must be selected individually.
In case of persistent slow-transit constipation, a dosage adjustment of Forlax is required to increase the latter with daily dosing of the drug in the first 3-4 days, since in such patients the restoration of lost intestinal motor function occurs gradually. Forlax in these cases can be combined with prokinetics (in particular, with selective 5-HT4 receptor agonists).
In patients who have used stimulant laxatives for many years, switching to osmotic drugs such as Forlax requires prolonged use of these drugs, since it takes a long time to restore the sensitivity of the receptor apparatus of the intestinal mucosa to natural stimuli.
In conclusion, I would like to emphasize once again that effective treatment of constipation is achieved by choosing the optimal treatment regimen that improves the patient’s quality of life. Taking into account the high effectiveness and good tolerability of the drug Forlax, in many cases it should be preferred, especially when treating elderly patients. The use of this laxative allows for stable and long-term treatment of patients with constipation, ensuring the achievement of a lasting therapeutic effect.
Literature 1. Minushkin O.N., Elizavetina G.A. Constipation and some principles of their treatment // Clinical pharmacology and therapy. 1997. No. 1. P. 52-53. 2. Minushkin O.N., Elizavetina G.A. Forlax is a new drug for the treatment of constipation” // Materials of the 3rd Russian Gastroenterological Week. 1997. P. 105. 3. Minushkin O.N., Elizavetina G.A. Laxatives in the treatment of constipation // Clinical pharmacology and therapy. 1998. No. 1. P. 87-90. 4. Minushkin O.N., Elizavetina G.A., Zverkov I.V. Constipation and forlax // Materials of the congress “Man and Medicine”. M., 1999. P.63. 5. Grigorieva G.A. Constipation and modern laxatives // Clinical medicine. 1997. No. 1. P. 52-56. 6. Grigorieva G.A., Hammad E.V., Mikhailov A.N. Problems of gastroenterology in gerontology. M., 1994. S. 45-46. 7. Kabanov A.V. Functional constipation: mechanism of development and the role of dietary fiber in treatment. Diss. Ph.D. honey. Sci. M., 1989. 8. Frolkis A.V. Functional diseases of the gastrointestinal tract. L., 1991. 9. Rumyantsev V.G. Constipation: tactics of patient management in the clinic // Consilium medicum. 2002. No. 1. P. 30-33. 10. Grigoriev P.Ya., Ya Kovenko E.P., Agafonova N.A. Constipation in clinical practice // Russian Medical Journal (Diseases of the digestive system). 2004. T. 6. No. 2, pp. 57-63.
Recommended dose of Forlax 4 g
For children:
- from 6 months to 1 year – 1 sachet per day,
- from 1 year to 4 years 1-2 sachets per day,
- from 4 to 8 years 2-4 sachets per day.
The effect of Forlax appears 24-48 hours after administration.
The duration of treatment should not exceed 3 months . Maintaining the effect after restoring normal bowel function should be achieved through an active lifestyle and a diet rich in plant fiber.
Forlax
Forlax (INN - macrogol) is an original French laxative with osmotic properties. Used in the treatment of constipation in both adults and children. Urbanization, sitting in front of a computer monitor, a decrease in the quality of life, and bad gastronomic habits (lack of plant fiber in the diet and excess flour) have long made the problem of constipation one of the most urgent. It is necessary to clearly understand that taking laxatives is an extreme measure, which should be resorted to only if physiological methods of correcting digestion are unsuccessful. But drug therapy is also not a panacea in this case: after all, as you know, as the duration of the course increases, the effectiveness of laxatives disappears (after 10 years of regular use, on average, no more than 11% of patients respond to them). At the same time, the constant use of laxatives over time negatively affects the functions and structural and morphological characteristics of the colon: dyskinesia is noted (about a third of patients develop inertia of the large intestine), atrophic degeneration of the mucosa, and local foci of inflammation. The drug Forlax, as its manufacturer, a well-known French pharmaceutical company, assures, is largely devoid of these shortcomings. The active substance of Forlax, macrogol, is a high-molecular compound that is capable of hydrogen bonding water molecules, holding it in the intestinal lumen. The result of this is the normalization of consistency (increased fluid content) and volume of stool, optimization of intestinal motility without interfering with neurohumoral regulatory mechanisms.
As a result, the previous defecation regime is restored. Forlax is not absorbed, is not metabolized and does not change the acidity of intestinal contents. When taking Forlax, unlike many other laxatives, there is no irritation of receptors and damage to the intestinal mucosa, even with prolonged use (in fairness, it should be recognized that this positive quality is characteristic of all osmotic laxatives). This circumstance, coupled with the high effectiveness of Forlax, makes it one of the best means of correcting chronic constipation. And although elderly patients are more often prescribed lactulose-based laxatives, it should be noted that at the slightest manifestation of negative side effects, transferring such a patient to Forlax would be completely justified.
Forlax is available in powder form for the preparation of an oral solution for adults and separately for children. The therapeutic effect begins to appear a day or two after taking the drug. The dosage regimen is as follows: 1-2 sachets in the morning or 1 sachet in the morning and in the evening (this is not a dogma - the dose can be adjusted according to circumstances). Before use, the powder is dissolved in a glass of water. The duration of treatment for adult patients and children over 8 years of age is usually 3 months. If symptoms of constipation persist after 3 months of regular use of the drug, an additional in-depth diagnostic examination is necessary.
Mode of application
Contents of 1 – 2 packets (10 – 20 g), preferably as a single dose in the morning or 1 packet (morning and evening) in case of taking 2 packets per day. The daily dosage should be adapted according to the clinical effect and may vary from 1 packet every day (especially in children) to 2 packets per day. The contents of each package should be dissolved in a glass of water immediately before use. The effect of taking Forlax® is expressed within 24 – 48 hours after taking the drug.
Recommended course of treatment for children and adults – 3 months
Maintaining the effect after restoring normal bowel function should be achieved through an active lifestyle and a diet rich in plant fiber.
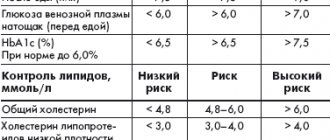
- Does not contain sugar, salt, electrolytes.
- Suitable for people with diabetes and galactose intolerance
- Can be taken by pregnant and lactating women
Maintaining the effect after restoring normal bowel function should be achieved through an active lifestyle and a diet rich in plant fiber.
- Does not contain sugar, salt, electrolytes.
- Suitable for people with diabetes and galactose intolerance
- Can be taken by pregnant and lactating women
Contraindications
- Inflammatory bowel diseases (eg, ulcerative colitis, Crohn's disease, pathological dilatation of the intestine);
- Intestinal perforation or risk of its occurrence;
- Intestinal obstruction or suspicion of it;
- Abdominal pain of unknown origin.
- Hypersensitivity to macragol (polyethylene glycol) or any of the components of the drug
- Children under 8 years old
For more detailed information, see the Instructions for medical use of the drug Forlax 10 g
Instructions for medical use of the drug Forlax 10g (pdf, 566 kB)
Literature: 1. S.V. Cheryomushkin, Yu.A. Kucheryavyi, A.Yu. Goncharenko et al. “Retrospective assessment of the effect of polyethylene glycol in the treatment of chronic constipation” // Journal Vrach.-3. 2013 2. Dupont C. et al. A dose determination stidy of polyethylene glycol 4000 in constipated: factors influencing the maintenance dose. J Pediatr Gastroenterologist Nutr. Feb 2006; 42(2):178-85