Molluscum contagiosum in children
Molluscum contagiosum is more common in children than in adults. Children up to one year old practically do not get sick with molluscum contagiosum. This is due to the fact that in the first year of life the child’s circle of contacts is small: the child moves in a limited space, often specially prepared for him and under the strict supervision of adults, without trying to come into contact with other children. But as soon as a child begins to actively communicate and independently explore the world, the threat of becoming infected with molluscum contagiosum increases sharply.
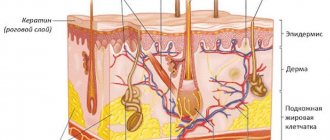
The peak incidence of molluscum contagiosum in children occurs between the ages of 2 and 6 years. Immunity at this age is still weak. Children become infected through toys or dirty hands. The virus penetrates the skin in the place where the integrity of the skin is damaged - through wounds, abrasions, cracks. Children's skin is delicate and sensitive, and the activity of a preschool child is great. As a result, numerous microtraumas occur, opening the way for infection. Cases of infection with molluscum contagiosum while swimming in the pool have also been described.
From 6 to 10 years, the incidence of molluscum contagiosum decreases. Instilling household hygiene skills is of great importance. The sooner your child starts taking care of clean hands, the better.
Method of transmission and risk groups
The content of the article
Since this disease is sexually transmitted, the most common method of transmission is unprotected sex. Since the virus spreads from person to person through contact with broken skin, it can also be transmitted through towels, clothing or toys. In an infected person, the virus spreads very easily by touching or scratching other parts of the body.
Most frequently infected groups:
- sexually active young people;
- then children (from 1 to 10 years);
- people with weakened immune systems;
- aged people.
Symptoms of molluscum contagiosum
The incubation period of the disease ranges from two weeks to several months, but most often the rash appears on the 14-15th day.
At first, single rashes appear, then there are more of them. Molluscum contagiosum can affect any area of the skin except the palms and soles. In children, exposed areas of the arms and legs, as well as the face and neck are most often affected. In adults, the genital area and the inner thighs are most often affected.
In the typical form of the disease, the rashes are located only in one anatomical area; in the generalized form, they spread throughout the body.
Rash
The elements of the rash look like protrusions (papules), firm and painless to the touch, pink or flesh-colored, with a pearlescent top. In the center of the papule there is a small depression, from which, when pressed, a white pasty mass is squeezed out. Papules have a round or oval shape, the size usually varies in the range of 2-5 mm, but sometimes the nodules merge, and then such formations can reach a diameter of 1 cm or more.
More about the symptom
Itching
In some cases, the rash is accompanied by itching, which intensifies when scratching. Under no circumstances should papules be scratched, as this can lead to a bacterial infection. The presence of a bacterial infection is indicated by redness of the skin around the papules, swelling, and suppuration.
More about the symptom
Folk remedies
Photo: kräutererleben.at
Traditional medicine has long been familiar with molluscum contagiosum and methods of its treatment. To get rid of rashes, use:
- Celandine juice. The juice from a freshly picked celandine stem is applied directly to the shellfish once a day until complete recovery. This remedy should be used with great caution, since celandine contains toxic components.
- A decoction of the string. Two tablespoons of dry string are brought to a boil in 250 ml of water, allowed to brew for an hour and filtered. The resulting decoction is used for a week, wiping the area of the rash three times a day.
- Garlic. The head of garlic, ground to a pulp, is mixed with butter in a 1:1 ratio. Before use, warm the oil to room temperature and lubricate the rashes three times a day. If the skin is not sensitive to garlic, only the juice of this plant can be used for rubbing.
- Alcohol tincture of calendula copes well with infection and prevents the development of bacterial complications.
- Various oils and ointments based on eucalyptus extract can also be used to lubricate rashes.
- After surgery, bird cherry juice will help greatly to restore the integrity of the skin and prevent the formation of scars. It has good regenerating properties and promotes rapid healing. Bird cherry juice is squeezed from the leaves of the plant. It is recommended to take fresh juice for each new use, but it is also acceptable to store it in the refrigerator for several days.
- If you have potassium permanganate powder somewhere in your supplies, then a strong solution made from it is suitable for fighting molluscum contagiosum. The rash should be lubricated 2 times a day for a week.
- Like celandine juice, nodules are treated with juice from freshly picked dandelion stems and leaves 2-3 times a day. You can also prepare an alcohol tincture from dandelion roots, which should be used to treat large areas of rashes.
- Herbal decoction. To prepare it, calendula, eucalyptus, juniper berries, pine shoots, birch buds, and yarrow herb are used. Everything is taken in equal proportions, crushed to a homogeneous mass and mixed thoroughly. A fresh decoction is prepared every day. For a glass of water you need a pinch of the mixture. Bring to a boil, let cool. Take half a glass orally at a time, twice a day, and also lubricate the rash with gauze soaked in the broth.
Herbal tincture. Walnut leaves, calendula and celandine are mixed in equal proportions. After grinding, the mixture is poured with vodka in a ratio of 1:3. Infuse in a dark, cool place for 3-4 weeks, after which the prepared tincture is applied to the rashes 4 times a day.
The information is for reference only and is not a guide to action. Do not self-medicate. At the first symptoms of the disease, consult a doctor.
Methods for diagnosing molluscum contagiosum
Molluscum contagiosum can be confused with manifestations of other diseases, including serious ones such as syphilis or cancer. Also, the activity of the molluscum contagiosum virus increases with a decrease in immunity, so in 20% of cases molluscum contagiosum accompanies HIV infection. This means that when rashes appear that correspond to the description of molluscum contagiosum, a medical examination is required to rule out such options.
When contacting a dermatologist, the doctor will examine the patient, make a diagnosis and suggest a treatment method.
Inspection
In most cases, the diagnosis of molluscum contagiosum is made by a dermatologist based on the results of an examination of the patient.
PCR diagnostics
Since HIV often accompanies molluscum contagiosum, PCR diagnostics for HIV can be prescribed.
More information about the diagnostic method
Serological blood test
When molluscum contagiosum is detected in adults, a serological blood test is prescribed to identify sexually transmitted infections (hepatitis B and C, HIV, syphilis, etc.).
More information about the diagnostic method
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Diagnostics
Photo: shareably.net
The diagnosis of molluscum contagiosum is based on the clinical picture - the detection of specific nodules on the patient’s skin. However, in cases of atypical forms, scraping of elements will be required for microscopic examination. Using special dyes, large brick-shaped viral bodies are detected under a microscope in epithelial cells.
For the differential diagnosis of molluscum contagiosum, skin diseases such as vulgar warts, flat warts, keratoacanthomas, milia, and acne are excluded.
Treatment methods for molluscum contagiosum
Molluscum contagiosum should be treated by a doctor. You should not try to remove papules yourself - this can lead to bacterial infection.
Treatment of molluscum contagiosum depends on a number of factors, primarily on the stage of development of the disease, the severity of symptoms and the state of the patient’s immunity. The following methods can be used:
Instrumental removal
Papules can be removed instrumentally, followed by treating the wound with antibacterial agents.
Credestruction
Cryodestruction is the removal of papules using exposure to low temperatures. Papules are treated with liquid nitrogen. Tissues treated in this way freeze and die.
Radio wave removal
Molluscum contagiosum papules can be removed using the radio wave method (using the Surgitron apparatus) and using a laser.
Electrocoagulation
Electrocoagulation is the effect of high-frequency current on papules. It is popularly described as “cauterization with electricity.” At the moment of discharge, a local strong thermal effect occurs, the tissues coagulate, which virtually eliminates the risk of infection at the treatment site.
Conservative treatment
The course of treatment for molluscum contagiosum may include conservative treatment with ointments and creams, as well as taking antiviral drugs (if the affected area is large).
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
Rate how useful the material was
thank you for rating
Medicines
Photo: chinastudy.it
After destruction of the molluscum contagiosum element, solutions of iodine, brilliant green, and fucorcin are used for reliable and relatively long-term disinfection of the skin.
To treat molluscum contagiosum, topical agents containing antiviral and immunomodulatory components can be prescribed. For example:
- Cycloferon, Viferon, Infagel. The drug has an anti-inflammatory effect and inhibits the ability of the virus to reproduce. Effective in the fight against viruses of molluscum contagiosum, herpes, as well as infectious diseases of the oral cavity and genital organs. Apply twice a day for a week.
- Imiquad. An immunostimulant cream that enhances the body's production of interferons - special substances necessary to fight viral infection. It should be applied to previously cleansed skin and not washed off for a long time, for example at night.
- Oxolinic ointment. Has a pronounced antiviral effect. Apply two to three times a day until the elements of molluscum contaginosis disappear.
- Acyclovir. In the form of an ointment, it is also applied to the nodules 2-3 times a day until recovery. Used in children over 3 years old. To enhance the antiviral effect, it can be used in a mixture with oxolinic ointment in a 1:1 ratio.
To strengthen the immune system and better fight infection, the following may be prescribed for internal use:
- Isoprinosine tablets. The medicine has anti-inflammatory and immunomodulatory properties, helps the body fight infection.
- Viferon in the form of candles. Has similar effects. Convenient for use in children.
Acyclovir and other antiviral drugs are prescribed only to patients with impaired immunity.
Main transmission options
The virus that causes the disease is transmitted from one person to another. Representatives of the animal world are not carriers of orthopoxvirus. There are 3 main infection options:
- Due to sexual intercourse with an already infected person;
- through water;
- contact-household method.
The last case occurs most often. You can become infected through tactile touch (hugs, travel on public transport, massage of a sick subject). This explains why children are often treated for this disease.
The indirect contact route is dangerous because a person cannot be sure that infection will not occur even in the absence of obvious signs (an incubation stage is possible).
You can simply walk into an unfamiliar room, sit on the sofa and become a carrier of the virus. After all, it is wonderfully preserved in various materials. Therefore, it is necessary to carry out thorough disinfection in residential premises and public places.
Another situation is frequent change of sexual partners. In this case, the person takes responsibility for his health. You need to understand that contraception cannot protect against all diseases.
In this case, even a hug will be enough to cause health problems. Although the virus foci are predominantly located in the genitals, so a condom can still protect against infection.
The waterway is often not classified as a separate group. In fact, infection occurs through water, but viral particles enter it from an infected subject. Therefore, many experts are inclined to believe that this is also a household contact route.
A similar outcome of events is possible when visiting swimming pools, saunas and public beaches.
In addition, a person who has previously suffered from molluscum contagiosum may become self-infected again. This happens when the skin rubs. But regardless of the method of infection, the clinical symptoms are very similar.
Some people are immune to this infection.
Treatment
If the eyelid area and genitals are not affected, it is recommended not to resort to therapy. Literally after a few months the signs disappear on their own. The human body develops immunity to the virus that causes the disease. But this takes time. But after removing the nodules, traces may remain.
However, in some cases, doctors still advise removing the nodules. Children tend to scratch them, which leads to a protracted form of the disease. In addition, concomitant diseases are possible.
Removal is carried out using liquid nitrogen or products designed to remove various warts.
Often one of the active ingredients is salicylic acid. But still, experts are in no hurry to remove such formations, so as not to leave traces, and it is better to ensure immunity to this disease. The body itself must resist viruses of this kind. Complications are rare.
There are 4 ways to remove molluscum on the skin:
- freezing;
- mechanical;
- taking antibiotics;
- immune therapy.
The mechanical method uses a scalpel or a special device. This method has a significant drawback: there is no anesthesia, so it is a rather painful process.
Afterwards the rash is cauterized with iodine. This removal option is not recommended for children.
Laser removal is a modern and popular method. Despite the high cost, this is what most experts recommend.
The skin is minimally injured and it does not take much time. No discomfort. Relapse is minimized. But we must not forget that we need to disinfect clothes and household items.
Immune therapy is preferred for skin lesions in children. It is based on antiviral ointments. After the course of treatment, formations disappear and the immune system is strengthened.
Treatment with antibiotics is undesirable. It is necessary in advanced stages with a large number of rashes and severe redness of the skin.
The most gentle treatment option is immunotherapy. There is no serious burden on the body and no pain.
Recommendations for caring for a child during illness
To avoid spreading the infection to other parts of the body, the following recommendations should be followed:
- Cover the lesions with tiny bandages.
- Wash your hands often.
- Wash clothes in hot water and iron with a hot iron.
- Clean your child's skin with a hydrogen peroxide solution.
Rice. 15. If you have molluscum contagiosum, you should constantly clean and lubricate the skin with antiseptics.
Prevention
Special complications usually do not arise. Prevention lies in following the rules of skin care. It is necessary that each family member has their own means of cleansing the body.
Most often, molluscum contagiosum affects children. Parents must take care of the child's hygiene. Swimming pools are especially dangerous. Often the virus is contained in the water in which a large number of people bathe.
Most modern pools are thoroughly disinfected, but there are exceptions.
It is important to wash your hands after using public transport. It is advisable to use an antiseptic.