Pathophysiology
The content of the article
Under normal conditions (in a healthy person), the contents of the gastric juice with high acidity periodically enter the esophagus, but internal protective mechanisms either reduce the amount of acid secreted to a minimum or remove the acid, which is quickly removed by “cleansing” the esophagus. Therefore, symptoms of acid irritation of the esophagus are not felt or are minimal.
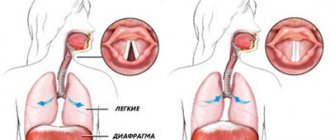
Mechanisms that protect the esophagus from stomach acid include the lower esophageal sphincter (sphincter) and normal esophageal motility (motility). When these mechanisms are disrupted, reflux occurs and symptoms of GERD occur.
Gastroesophageal reflux
On a note
Trying to relieve the unpleasant symptoms of heartburn, many are accustomed to drinking baking soda dissolved in water. Under no circumstances should this be done. Soda may initially “put out the fire,” but then the acid is produced with a vengeance. And this can cause even more heartburn. In addition, soda enters into a violent chemical neutralization reaction with acid (a good example is quenching soda with vinegar). The gas released stretches the stomach and can cause bloating and worsen stomach ulcers.
By the way
Heartburn often accompanies pregnancy. One of the reasons for this is toxicosis, which is often accompanied by nausea and vomiting. Vomit irritates the esophagus, causing a burning sensation. In addition, the increasing size of the uterus leads to increased intra-abdominal pressure. As a result, the stomach valve does not close tightly, causing food to flow back into the esophagus.
Important!
When treating heartburn, it is very important not only to temporarily neutralize the acid (antacids), but also to normalize gastric motility (prokinetics)!
Etiology: a new approach
The prevailing theory (since 1935) is that GERD occurs when acidic stomach acid spills from the stomach into the esophagus, chemically and mechanically damaging the lining of the esophagus, causing burns, irritation, erosions, and ultimately more serious consequences. However, this traditional theory of chemical and mechanical irritation of the esophageal mucosa cannot fully explain many things associated with the onset, symptoms and course of GERD.
There are now reports that GERD may be an immune-mediated inflammatory disease caused by immune reactions rather than direct chemical damage to the lining of the esophagus by gastric juices. The hypothesis about the etiology of immune GERD is confirmed by one of the clinical studies conducted in the USA. The study results were published in the Journal of the American Medical Association.
Preliminary data from this study showed that T-cell esophagitis, basal cell hyperplasia, and spleen cell hyperplasia were observed in patients with severe GERD treated effectively with proton pump inhibitors (PPIs) after PPI discontinuation, but with resistant superficial cells.
According to study leader at the Dallas Veterans Medical Center, Dr. Kerry Dunbar, This finding suggests that the pathogenesis of reflux disease may be related more to inflammatory mediators and cytokines than to chemical damage to the esophageal mucosa.
The inflammatory immune theory of GEB could more easily and better explain not only the onset and course of the typical symptoms of this disease, but also the pathophysiology of the complications of this pathology - metaplasia of the esophagus and Barrett's mucosa.
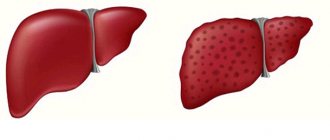
Barrett's esophagus
Recent experimental studies in rats also suggest that GERD is more related to immune rather than chemical acid damage to the esophageal mucosa. Reflux and chemical acid irritation are thought to only initiate immune inflammatory responses in the esophageal mucosa and therefore play a less important role.
If the immuno-inflammatory theory of the etiopathogenesis of GERD turns out to be correct, it may be necessary to reconsider the existing regimen for the treatment and prevention of relapses of GERD. It is possible that the location and role of antisecretory drugs (PPIs, H2 blockers) may change.
It is assumed that the immune theory of reflux disease can explain in more detail the causes and essence of not only typical, but also recently described atypical forms (so-called subtypes) of GERD.
Researchers suggest that PPIs and H2 blockers may remain the most important drugs for treating GERD, but treatment regimens for this disease should also include drugs that affect the immune-inflammatory response cascade, especially for more severe and refractory forms of GERD.
Active ingredient: Calcium carbonate + magnesium hydroxycarbonate
Trade name of the drug:
- Rennie (tablets) (Bayer)
Features of the drug that are important for the patient to know about
Due to the content of calcium carbonate, it is one of the fastest-acting antacids. In just 3-5 minutes, Rennie turns acid - the main cause of heartburn - into water. The drug is in the form of chewable tablets with a pleasant taste and does not need to be washed down with water. Rennie can be used throughout pregnancy. Contraindicated in the presence of kidney stones and severe renal failure.
Treatment of gastroesophageal reflux disease
According to current guidelines, GERD is treated in stages. Goal of treatment: control the symptoms of the disease, treat esophagitis, prevent relapses of esophagitis and complications of the disease.
Treatment of GERD consists of the following steps:
- Lifestyle changes and control of gastric juice secretion (antacids, PSI, H2B).
- If necessary, surgical treatment is used, and corrective antireflux surgery is performed.
Non-pharmacological measures include the following:
- Reducing excess weight;
- Refusal of certain drinks and foods (alcohol, chocolate, citrus fruits, tomatoes), mint, coffee, onions, garlic;
- Frequent meals at regular intervals;
- Sleep at least 3 hours after eating, with your head raised (~ 20 cm);
- Limiting squats, bending, etc.
Eating frequently at regular intervals
Prevention
To avoid heartburn, you must first eat right. Try to eat more often and little by little, have dinner no later than two, and preferably three hours before bedtime.
Eliminate fast food, spicy, fried, fatty foods, as well as carbonated drinks, coffee, citrus fruits and other sour fruits from your diet.
Do not lie down after lunch for the next hour and a half. After lunch, it is advisable to stand or walk. This will help the food move further under the influence of gravity.
When sleeping, your head should be 15 cm higher than your body - raise the head of the bed.
Try not to wear clothes that are too tight and put pressure on your stomach.
Avoid work that involves constant bending.
Mint and alcohol. 8 foods that cause heartburn Read more
Antacids
Until the 1980s, antacids were the standard treatment for mild forms of GERD. They are still used to reduce symptoms of mild reflux. Antacids are taken after each meal and before bed.
Taking antacids before bed
Antacids are also useful for side effects: they relieve constipation (aluminum antacids: ALternaGEL, Amphojel), they can increase loose stools (magnesium antacids: Phillips Milk of Magnesia). Aluminum hydroxide increases the pH of the stomach contents to >4 and inhibits the proteolytic activity of pepsin, reducing the symptoms of indigestion. Antacids do not reduce the frequency of reflux, but they do reduce the acidity of the fluid.
Magnesium hydroxide suppresses the symptoms of acidosis and improves digestion. Magnesium hydroxide antacids osmotically retain fluids in the intestine, which distends the intestinal wall, stimulates intestinal motility, and softens stools (laxative effect). When interacting with hydrochloric acid of gastric juice, magnesium hydroxide is converted into magnesium chloride.
Active ingredient: Algeldrate + magnesium hydroxide
Trade name of the drug:
- Gastracid (tablets)
Features of the drug that are important for the patient to know about
A classic antacid with an adsorbing and enveloping effect. The use of the drug during pregnancy and breastfeeding, as well as for children under 12 years of age, is not recommended without consulting a doctor.
Are you suffering from heartburn? How not to overpay for drugs Read more
New antacids and antirefluxants
Alginic acid salts have been used clinically to relieve symptoms of heartburn and esophagitis for over 30 years. Alginic acid salts have a unique mechanism of action: when interacting with gastric acid, alginates precipitate and form a gel that covers the esophageal mucosa with a protective layer and promotes its restoration.
In vitro and in vivo studies have shown that alginates combine carbon dioxide and some antacid components. Recent kinetic studies have shown that alginates bypass acidic contents and reach the esophagus before the esophageal contents, protecting the organ mucosa from mechanical and chemical irritation from hydrochloric acid. According to clinical studies, alginates also act as a physical barrier, thereby more effectively suppressing reflux.
Alginate products contain antacids, which are acid neutralizing agents that reduce heartburn, but studies have not shown that the effectiveness of these combination drugs depends on their neutralizing properties.
The clinical effectiveness of alginate preparations depends on many factors: the amount and penetration of carbon dioxide released, the characteristics of the molecule, additional ingredients (aluminum, calcium) that have a positive potentiating effect.
Alginate preparations remain in the stomach for several hours, so they last significantly longer and are more effective in suppressing the symptoms of GERD than traditional antacids, they begin to work quickly and last a long time. Alginate preparations are completely safe and are therefore used to reduce the symptoms of reflux in infants, children and pregnant women.
For example, one of these magnesium alginate preparations, Refluxaid, is used in European countries to reduce the symptoms of reflux and acidosis in GERD, peptic ulcers, esophagitis, functional dyspepsia, and other functional and inflammatory diseases of the gastrointestinal tract, manifested by heartburn, reflux, and epigastric discomfort.
Refluxaid drug
The magnesium alginate in Rexluxaid is a natural substance extracted from seaweed. The drug has a high viscosity, which increases anti-reflux effectiveness and duration of action. It has emulsion and swelling properties.
Studies have shown that the highly viscous compound Refluxaid, when ingested into the stomach, creates a physical barrier that binds and neutralizes gastric juice, thereby protecting the esophagus from symptoms of reflux: heartburn, burning behind the sternum, chest pain, epigastric discomfort, etc. Taking these The medication reduces heartburn, acid regurgitation, dysphagia and odynophagia (difficulty swallowing and pain) are reduced, and extrazophaginic symptoms of GERD are also suppressed - cough, hoarseness.
Refluxaid is a prescription medication. It is used for episodic relief of symptoms of acidosis, reflux and esophagitis, on demand or in combination with anti-reflux medications (antisecretory PPIs, H2 blockers, prokinetics).
It has been found that when a person sleeps, magnesium alginate can remain in the stomach for up to 8 hours without breaking down—enough time for the patient to get a good night's sleep. Taking reflux before bed may improve the quality of sleep in a patient with GERD because the symptoms caused by nocturnal reflux will be suppressed.
Interesting
Can also lead to heartburn:
Smoking. This bad habit weakens the barrier between the stomach and esophagus and reduces the resistance of the esophageal mucosa to damage.
Excess weight. The more you weigh, the more likely you are to have heartburn. Fat that accumulates in the abdominal cavity lifts the diaphragm and thereby weakens the esophageal valve.
Genes. Research in recent years has shown that 30 to 45% of heartburn cases depend on genetic factors. Everything else depends on you - on nutrition, bad habits and lifestyle.
Antisecretory drugs, H2 receptor blockers
This is the first-line treatment for mild to moderate GERD and grade I-II esophagitis. Four H2 blockers are commonly used in clinical practice: ranitidine, famotidine, cimetidine, and nizatidine. They are more effective in suppressing unstimulated secretion of gastric juice with food and are therefore recommended on an empty stomach or at night.
H2 blockers are effective in the treatment of mild esophagitis (70-80% of patients recover), as well as in antirecessive treatment and prevention of relapses. The effectiveness of H2 blockers decreases with long-term use, leading to tachyphylaxis. An H2 blocker is recommended for patients suffering from nocturnal reflux symptoms, especially in Barrett's temple.
Who should not take it
There are contraindications for prokinetic drugs:
- Hypersensitivity to the active substance.
- Stomach or intestinal bleeding.
- Perforation of the stomach or intestines.
- Intestinal obstruction.
- Acute liver failure, kidney dysfunction.
It is not recommended if the work requires increased attention and concentration, as well as for those who drive a car. Prokinetics should be prescribed to older people with caution.
Proton pump inhibitors (PPIs)
These are powerful drugs that suppress gastric secretion. Clinical studies have shown that they are most effective in treating GERD. PPIs are generally well tolerated and cause relatively few side effects. However, PPIs can disrupt calcium homeostasis, exacerbating existing cardiac conduction abnormalities. PPIs increase the risk of hip fractures in postmenopausal women.
Multiple clinical trials have concluded that PPIs are more effective than H2 blockers in controlling GERD symptoms over 4 weeks. And are more effective in treating esophagitis within 8 weeks. It also reports that no one PSI drug was found to be more effective than others in controlling GERD symptoms over 8 weeks.
Although PPIs are the most effective antisecretory drugs, their use, especially over a long period of time, is associated with many side effects. Firstly, PPIs have restrictions on their use: they cannot be used in children under 1 year of age, pregnant or lactating women. PPI use during pregnancy has been shown to increase the risk of birth defects (heart defects).
Restrictions on the use of PPIs
Research conducted in the United States shows that overuse of PPIs has dangerous consequences. Therefore, the US FDA warns doctors and patients that there should be no more than three 14-day courses of treatment per year. Long-term or frequent use of PPIs is associated with an increased risk of bone fractures, hypovitaminosis B12, electrolyte imbalances (primarily hypomagnesemia), muscle spasms, and even seizures.
Excessive suppression of gastric acid secretion when taking PPIs can cause epigastric discomfort, indigestion, increased intestinal infections (C. difficile, etc.), and the risk of aspiration pneumonia. The risk of infectious complications is even higher when PPIs are used with H2 blockers.
We recommend:
Exercises to prevent heartburn
Starting position - standing, sitting or lying on your back.
1. Place your palms on the lower abdomen on either side of the navel.
2. Close your mouth and inhale through your nostrils.
3. Slowly exhale the air, slightly pressing the abdominal wall and as if lifting your stomach with your hands.
4. Inhale slowly, pushing your stomach out as far as possible.
5. Repeat the exercise 2-3 times. Over time, increase the number of repetitions to 12 times.
Are you suffering from heartburn? What is the reason and how to get rid of it Read more
Prokinetics
Prokinetics are only effective in treating mild forms of GERD. If GERD is more severe, in addition to prokinetics, drugs that inhibit the secretion of gastric juice are usually prescribed.
Of the prokinetic agents, metoclopramide (10 mg/day orally) is prescribed in European clinics - this is the most commonly prescribed regimen in adults with GERD. Long-term treatment with prokinetic drugs can be dangerous, with serious, even fatal, complications.
ONLINE REGISTRATION at the DIANA clinic
You can sign up by calling the toll-free phone number 8-800-707-15-60 or filling out the contact form. In this case, we will contact you ourselves.
For what diseases is it prescribed?
As mentioned above, prokinetics are used in monotherapy or together with antibiotics. Doctors know that there are diseases for which the administration of prokinetics increases the effectiveness of treatment several times. This group includes:
- Diseases of the digestive system with impaired motor activity.
- Gastroesophageal reflux disease.
- Peptic ulcer of the stomach (duodenum).
- Idiopathic gastroparesis.
- Vomiting.
- Constipation.
- Irritable bowel syndrome.
- Diabetic gastroparesis.
- Flatulence.
- Nausea caused by drug and radiotherapy, infection, functional disorders, poor diet.
- Dyspepsia.
- Biliary dyskinesia.
Active ingredient: Ranitidine
Trade name of the drug:
- Gistak (Ranbaxy)
- Zantac (Glaxo Smith Klein)
Features of the drug that are important for the patient to know about
One of the most famous drugs in this group. It lasts for about 12 hours, so it is taken 2 times a day. May cause a false positive reaction when testing for protein in the urine. Contraindicated in children under 12 years of age. Smoking reduces the effectiveness of the drug. It can enter into numerous drug interaction reactions, increasing the concentration in the blood and, accordingly, the toxicity of other drugs. Therefore, before taking this drug, you must tell your doctor in detail about all previously prescribed medications.