Gastroesophageal reflux disease (GERD) is one of the most serious and complex pathologies of the esophagus. The disease can significantly impair the patient's quality of life. As it progresses, it leads to dangerous complications, including Barrett's esophagus and adenocarcinoma. GERD affects both men and women equally often and is difficult to treat. Experienced specialists at the ACMD clinic will help you get rid of the unpleasant manifestations of GERD once and for all. Do not delay your visit to the doctor, contact us at the first symptoms!
Reflux esophagitis: etiology and pathogenesis
GERD is a chronic disease that occurs when the lower esophageal sphincter, also called the “muscle valve,” does not function properly. Gastroesophageal reflux occurs when stomach contents (undigested food, acid) reflux into the esophagus. Frequent contact of the esophageal mucosa with the contents of the stomach causes inflammation. Gastric juice literally dissolves the esophageal mucosa.
Important information! The World Organization of Gastroenterologists has recognized GERD as the most common disease of the 21st century. According to official data, about 50% of the world's population faces this disease.
The main cause of GERD is insufficiency of the lower alimentary sphincter, which develops due to a general decrease in tone or excessively frequent relaxation of the LES not associated with swallowing. Relaxation of the LES (lower esophageal sphincter) can be provoked by increased pressure in the peritoneum or subthreshold pharyngeal stimulation.
Why does reflux disease develop?
Very often, the exact cause of the development of GERD cannot be determined. The disease can be provoked by a combination of different factors, namely such as:
- weight gain;
- overeating fatty foods, unhealthy diet;
- excessive coffee consumption;
- alcoholism and energy drink consumption;
- smoking and other bad habits;
- taking certain medications.
Medicines that reduce the tone of the lower esophageal sphincter include:
- anticholinergic medications;
- antihistamines;
- tricyclic antidepressants;
- calcium channel blockers;
- progesterones and nitrate-containing agents.
Important information! American scientists associate GERD with a hereditary predisposition. The development of the disease can also be affected by: stressful situations, hormonal imbalances, and injuries to the esophagus.
Gastric reflux may be temporary. It is considered pathological only in cases where the frequency of attacks is more than 50 per day, as well as when the pH in the esophagus reaches 4.0 or lower. An attack of pathological reflux can be provoked by: a change in body position, increased abdominal pressure, or disruption of the usual diet.
Esophagitis: symptoms
The most striking and specific symptom of GERD is heartburn with or without the penetration of stomach contents into the oral cavity. Feelings of heartburn:
- “chill” at the bottom of the throat;
- burning and stinging in the throat;
- bitter or sour taste in the mouth;
- lump in the throat;
- nausea and stomach pain.
Frequent attacks of heartburn can lead to irritability, insomnia, anorexia, and chronic aspiration of stomach contents into the respiratory tract. Signs of chronic aspiration: cough, hoarseness, sore throat.
Distal reflux esophagitis may be accompanied by:
- pain when swallowing;
- esophageal bleeding;
- pain in the chest area;
- an unpleasant taste in the mouth that does not go away even after brushing your teeth.
Due to constant throat irritation, patients with GERD may develop chronic pharyngitis or laryngitis. At the same time, symptoms characteristic of the listed diseases are added (pain when swallowing, swelling of the throat, intoxication).
Clinical symptoms of GERD
Clinical symptoms of GERD are divided into esophageal and extraesophageal.
Esophageal symptoms
Heartburn “a burning sensation ascending from the stomach or lower chest to the neck.” With severe heartburn, this feeling may spread to the lateral chest and neck area, reaching the lower jaw. Heartburn may be accompanied by a feeling of “a warm wave rolling up to the throat” associated with the reflux of gastric contents. Heartburn may appear or worsen when bending forward, straining, lying down, or after eating. Standing, swallowing saliva, drinking a few sips of water, or taking antacids may reduce its intensity.
Regurgitation (or regurgitation) is the passive movement of stomach contents into the esophagus and then into the oral cavity. Often accompanied by a feeling of acidity or bitter taste in the mouth. It is provoked or aggravated by a horizontal position of the body, tilting the body, or an increase in intra-abdominal pressure. Regurgitation can lead to the reflux of contents into the pulmonary tract (aspiration) and lead to the development of laryngitis, cough, asthma and pneumonia. Belching is one of the variants of regurgitation. The main component is not gastric contents, but air. It can also be bitter or sour. Dysphagia, a feeling of food being “stuck” when swallowing and passing through the esophagus. At the initial stages of the disease, dysphagia occurs due to impaired motor function of the esophagus and is intermittent. In advanced cases with esophageal stricture, dysphagia becomes persistent.
Signs of the disease also include pain and discomfort in the epigastric region, pain in the chest, behind the sternum.
Extraesophageal manifestations of GERD
Symptoms of diseases of neighboring organs that can be caused by reflux:
- Cardiac symptoms (pain in the left half of the chest, heart rate abnormalities) can be triggered by reflux, hypermotility of the esophagus. Unlike angina, these pains have several features: they have a burning tint, have a retrosternal localization without irradiation, are caused by food intake, appear when changing body position and subside after taking drugs that reduce acidity.
- Pulmonary manifestations (cough, asthma attacks) are associated with vagal irritation and the appearance of bronchospasm or with the entry of stomach contents into the bronchi during regurgitation and the development of chronic bronchitis, repeated pneumonia, bronchial asthma and fibrosis of the lung tissue.
- ENT manifestations (hoarseness and loss of voice, dysphonia, sore throat, neck, hypersalivation) are associated with inflammation of the posterior wall of the larynx, pharynx, and the development of chronic laryngitis and pharyngitis.
- Dental manifestations (burning tongue, cheeks, impaired taste, caries) are caused by oxidation of saliva in the oral cavity, damage to the mucous membrane and demineralization of tooth enamel.
- Gastric (rapid saturation, fullness, distension of the stomach, nausea, bloating, flatulence.
GERD: classification and features of different forms
There are two main forms of GERD:
- Non-erosive - the most common, characterized by swelling and inflammation of the esophageal mucosa, but does not lead to the formation of wounds.
- Erosive - leads to the appearance of ulcers and erosions on the surface of the esophageal mucosa under the influence of an aggressive gastric environment.
The Los Angeles classification distinguishes the following degrees of GERD:
- A – one damage to the mucosa, limited to the esophageal folds, with a diameter of no more than 5 mm;
- B – one or more lesions of the mucous membrane, limited to the esophageal folds and not merging with each other, with a diameter of more than 5 mm;
- C – numerous lesions of the mucous membrane, occupying less than 70% of the circumference of the esophagus;
- D – numerous confluent lesions of the mucous membrane of the esophagus, occupying over 70% of its circumference.
How is GERD diagnosed?
If symptoms of reflux pathology appear, you should contact your family doctor or directly a gastroenterologist. First of all, the doctor carefully studies the clinical picture and complaints of the patient. Often the diagnosis can be made only by the clinical picture, without additional research. Sometimes the patient is prescribed additional diagnostic procedures, namely:
- endoscopy is the most informative way to diagnose GERD , which consists of visually studying the structure of the esophagus (helps determine narrowing, the presence of erosions and ulcers, changes in the composition of the epithelium);
- daily monitoring of the pH level in the esophagus - helps to assess the nature and synchronicity of the reflux of stomach contents into the esophagus;
- X-ray examination of the esophagus with barium - allows you to identify narrowings and hernias of the esophageal passage of the diaphragm.
Interesting fact: a healthy esophagus is able to push food into the stomach when swallowed in any body position, even when a person is lying upside down. And all thanks to proper peristalsis (muscle contractions).
GERD Treatment Methods
Treatment of GERD is carried out by a gastroenterologist. Treatment is aimed at relieving inflammation of the esophageal mucosa, reducing the frequency of reflux of stomach contents into the esophagus, reducing the damaging properties of refluxate (the substance that enters the esophagus from the stomach), and increasing the protective properties of the esophageal mucosa.
Of great importance is:
Drug treatment
Treatment with medications is prescribed by a doctor and must take into account the individual characteristics of the patient.
Lifestyle change
Normalization of lifestyle is of great importance. It is necessary to quit smoking, limit, or better yet eliminate, alcohol consumption. You should not eat fatty, spicy, sour foods, as well as coffee, tea, chocolate, legumes, cabbage, peas, and brown bread. It is better to take food more often (4-6 times a day), but in small portions. You should not eat before bed (the last meal should be 2-2.5 hours before bedtime). You should sleep with your upper body elevated to reduce the likelihood of reflux during sleep.
Make an appointment Do not self-medicate. Contact our specialists who will correctly diagnose and prescribe treatment.
GERD in children
Reflux esophagitis in children with diseases of the gastrointestinal tract is detected in 17% of cases (approximately). The exact prevalence of GERD in childhood is unknown, due to the variety of clinical manifestations of the disease.
Important information! The process of GERD itself can be quite natural for a child under one year of age. Due to the insufficient length and immaturity of the esophagus, stomach contents regularly enter it, and from there into the throat and oral cavity. In common parlance this is called regurgitation.
Signs of GERD in childhood are varied and numerous. You can suspect a disease in a child by:
- regular severe vomiting after eating;
- frequent belching with a sour aroma;
- prolonged hiccups;
- morning cough;
- a feeling of bitterness in the mouth;
- chest pain;
- night snoring;
- attacks of difficulty breathing;
- thinning and darkening of tooth enamel.
Treatment of gastroesophageal reflux disease in children is not much different from therapy for adults. Often the child outgrows the disease on his own, and it disappears without a trace, forever.
Modern treatment of gastroesophageal reflux disease
Treatment for GERD is aimed at combating symptoms and preventing consequences. It can be conservative and medicinal. First, doctors suggest the patient try to change their lifestyle:
- get rid of excess weight;
- switch to a normal regime of wakefulness and rest;
- give up bad habits (smoking, alcohol);
- switch to a balanced, gentle diet.
Diet is the main method of non-drug treatment of GERD. You need to eat small portions 5 times a day. It is recommended to avoid evening overeating (the last meal should be at least 2 hours before bedtime). You need to include more vegetables in your diet. Meat should be consumed after boiling or steaming. Spices, fatty foods, fried foods, carbonated drinks, and sour fruits are excluded from the diet. Dishes should not be too hot or cold.
Patients should avoid situations that increase abdominal pressure. You cannot wear tight trousers, belts, corsets, sweaters, or bandages. It is not recommended to jump, lift weights, or perform intense exercises that strain the abdominal muscles. Ideal sports for people with GERD: swimming, cycling, walking.
If heartburn attacks occur only when lying down, it is recommended to raise the head of the bed or choose a larger pillow. You should not lie down immediately after eating or drinking.
The patient will have to give up medications that can provoke attacks of GERD. Such drugs include:
- nitrates and nitrate-like agents;
- nifedipine, Theophylline, Progesterone;
- antidepressants and antispasmodics;
- non-steroidal anti-inflammatory drugs.
If symptoms of GERD persist, you need to switch to drug therapy. Help to get rid of the manifestations and complications of the disease:
- drugs from the group of proton pump inhibitors;
- combined antacids;
- dioctahedral smectite;
- prokinetics.
Drug treatment for GERD lasts from 4 to 8 weeks. After the main course, you need to undergo maintenance therapy lasting 6-12 months.
Complicated and advanced forms of GERD are treated surgically. To correct a defect in the esophagus, antireflux surgery is performed. In case of a hiatal hernia, a fundoplication is prescribed - suturing the stomach to the diaphragm around the opening of the esophagus, thereby creating a cuff that regulates the passage of food.
GERD: Algorithm of treatment tactics
Vladimir Trofimovich Ivashkin , academician of the Russian Academy of Medical Sciences, Doctor of Medical Sciences:
– We are moving on to our next series of lectures. And now Tatyana Evgenievna Polunina will tell us about the algorithm of treatment tactics in patients with gastroesophageal reflux disease.
Tatyana Evgenievna Polunina , professor, doctor of medical sciences:
– Dear Vladimir Trofimovich, dear colleagues! The presentation will present: epidemiology, pathophysiology, clinical manifestations, classification, diagnosis and modern treatment algorithm for gastroesophageal reflux disease. Particular attention will be paid to the modern three-step approach to the treatment of gastroesophageal reflux disease, according to which a rational choice of drugs is proposed.
Gastroesophageal reflux disease is a chronic, relapsing disease that is potentially dangerous due to its complications. About 40% of the world's adult population regularly experience heartburn. But gastroesophageal reflux disease appears as an iceberg. At the top are the symptoms, in particular heartburn, and at the bottom is a real iceberg, which can manifest itself in other clinical manifestations. In particular, these are bronchospasm, chest pain, obstruction, laryngitis, and so on.
In the epidemiology of acid-related diseases in the last millennium, you see an increase in gastroesophageal reflux disease, aka, esophageal carcinoma. And this explains such close attention to this nosology. According to Igor Veniaminovich Maev and Professor Trukhmanov, the constituent forms of gastroesophageal reflux disease include the non-erosive form - 68%, erosive esophagitis - 37% and Barrett's esophagus, a formidable complication of gastroesophageal reflux disease, is 3%.
GERD is a disease that reduces quality of life and is associated with the release of acidic contents from the stomach into the esophagus. The prevalence of GERD is widely underestimated. Some researchers suggest that GERD affects about 50 million people in Europe and 21 million people in the United States.
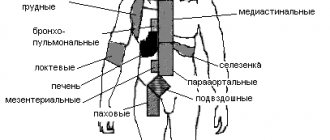
Extraesophageal manifestations of gastroesophageal reflux disease are very often a bronchopulmonary pathology, which is manifested by a dry cough, attacks of difficulty breathing, hoarseness, and an unpleasant taste. Laryngological symptoms and, accordingly, cardiological ones will be discussed in more detail in the next slide.
But the main factors in the formation of gastroesophageal reflux disease are decreased motility of the esophagus, decreased pressure of the lower esophageal sphincter, reflux of acid, pepsin, bile acids, slower gastric emptying from solid foods and impaired motility of the antrum of the stomach. Great importance is currently attached to the acid pocket, which is very important for the reflux of acid from the stomach, namely from the cardiac part of the stomach into the esophagus. It's presented here. A hiatal hernia complicates the course of gastroesophageal reflux disease. And this option always requires special endoscopic control.
This slide presents the symptoms. Heartburn is a key symptom, pain behind the breastbone, regurgitation, pain when passing food down the esophagus (odynophagia), feeling of a lump in the throat (dysphagia), bad taste in the mouth, persistent dry cough, hoarseness of the voice, episodes of difficulty breathing, rapid heartbeat and arrhythmia. With such symptoms, patients come not only to a gastroenterologist or therapist, but also to pulmonologists, ENT specialists, and cardiologists. And it is very important to have contacts with specialists in related specialties, because it is these symptoms that in some cases cause problems for pulmonologists, in particular dry cough, who cannot find out the cause. And accordingly, diagnostics are carried out to find out the true cause.
You see that heartburn ranks first according to statistics. Both hoarseness and cough are 4-7%, flatulence, sleep disturbance, indigestion, chest pain, nausea, sore throat, epigastric pain - this is the situation that is typical for patients with gastroesophageal reflux disease. Here are the epidemiological criteria of the Mail Clinic, which are fundamental in all epidemiological studies, in particular 15 clinical studies: 1 time per month is considered rare symptoms, but 1 time per week heartburn is the equivalent of gastroesophageal reflux disease. And if it repeats within 12 months, then it is clinically possible to make a diagnosis of gastroesophageal reflux disease.
“Masks” of GERD, about which we have already said that there is a pseudocardial form, ENT pathology, otology, bronchopulmonary and gastroenterological, so to speak, the main form. They are presented on this slide. Many faces. I would like to draw your attention to the presence of the Los Angeles endoscopic classification, which is key and is used in the Russian Federation and other countries.
In particular, by stages. You see. Grade A is one lesion (or more) of the mucous membrane, which is limited to the folds, and the length is 5 millimeters. Grade B is a damage of more than 5 millimeters, grade C - naturally, this lesion extends to two or more folds of the mucous membrane, but occupies less than 75%. And grade D is damage to the mucous membrane, which extends to 75% or more.
The Montreal Gastroenterology Consensus, which was held in 2005, proposed dividing gastroesophageal reflux disease into esophageal syndromes and extraesophageal syndromes. Esophageal syndromes without damage to the esophagus are a typical reflux syndrome and, accordingly, reflux chest pain syndrome. With damage to the esophagus, these are refluxoesophagitis, esophageal stricture, Barrett's esophagus and esophageal adenocarcinoma.
But extraesophageal symptoms, when a connection is established with gastroesophageal reflux disease, are just cough, reflux asthmatic syndrome, laryngitis, erosion of tooth enamel. The alleged connection with GERD is pharyngitis, sinusitis, recurrent otitis media, idiopathic pulmonary fibrosis.
Complications of gastroesophageal reflux disease are esophageal strictures. In particular, Barrett's esophagus is one of the most dangerous complications. And you see: here is the morphological shape of Barrett's esophagus with a normal esophagus, and how the edges of the velvety red mucosa are clearly defined, which is located on the pale mucosa of the esophagus, which the endoscopist has the right to place simply by visual inspection.
Barrett's esophagus is an acquired condition that is a complication of gastroesophageal reflux disease and is the replacement of stratified squamous epithelium with non-cylindrical epithelium with the phenomenon of intestinal metaplasia. It is a precancerous condition and occurs in 6-12% of patients with symptoms of gastroesophageal reflux disease. And most often - in 90-95% of cases - it is not diagnosed. Most often, this option in good clinics is established using not only endoscopic examination and chromatin staining, but also with NBI radiation, which is carried out during the examination. Most often this is 1% of the population.
Among patients, the age group of Barrett's esophagus, you see, begins to increase in patients from 50 years of age. It is dominated by men most often. But I want to say that from the age of 30 there is already a decent increase in statistics for Barrett's esophagus at the present time, and these data are currently being discussed. Because the sudden development of Barrett's esophagus is a very important point that requires monitoring.
Endoscopic classification is presented on this slide. You can see that there are both short segments and long segments in Barrett's esophagus, depending on the degree of damage to the mucous membrane and the length of the lesion, which is presented here on this slide.
Symptoms. There are no specific symptoms. These are frequent and prolonged attacks of heartburn, usually more than five years, dysphagia, nausea, chest pain. But weight loss (because food causes discomfort and pain) occurs quite often. During endoscopy, the columnar intestinal epithelium has a specific red color and “velvet” appearance. Easily distinguished from the thin, pale, glossy-surfaced normal squamous epithelium of the esophagus.
I would like to show you the film. Endoscopically - you can see here the length of the tongue damaging the esophagus. It is very important to pay attention to the edges of this tongue, measure the length, and take a biopsy in the required place. Biopsies are taken in five different locations. The location of the biopsy must be determined - this is a very important point. And you see different versions of Barrett's esophagus, which are presented here on microfilm. And, accordingly, different stages of damage and different species positions that endoscopists observe. They definitely record this on camera and take a biopsy from the edge.
Chromoesophagogastrography can be performed with methylene blue, and it is actively absorbed by the intestinal epithelium, “staining” areas of intestinal metaplasia. This is very important, because metaplasia can be of the large or small intestinal type, or complete or incomplete, which indicates different morphological stages. Metaplasia is a concept that is very important and includes the persistent replacement of differentiated cells of one type with differentiated cells of another type while maintaining the main species of the tissue. Metaplasia is a relatively benign change in tissue structure in response to chronic physical or chemical irritation.
Here is a goblet cell - a sign of intestinal metaplasia. It is a very important element. Accordingly, the count of goblet cells, as well as the structure of the epithelium, is a stage of dysplasia. And the histological stages of Barrett’s esophagus are necessarily indicated in the morphological protocol, because the patient’s management tactics depend on this; observation is necessarily indicated. Here in the first picture - there is no dysplasia. And a low degree of dysplasia, which implies a low number of goblet cells and, accordingly, small intestinal metachondria, is a fairly common option. And a high degree of dysplasia, which implies a large number of goblet cells and requires monitoring very clearly once every three or six months.
Suppression of clinical manifestations of gastroesophageal disease is the goal of treatment of Barrett's esophagus. Healing of erosive esophagitis, prevention of the development of adenocarcinoma.
Here is an algorithm for the diagnosis and treatment of gastroesophageal reflux disease, which was presented in Switzerland in the city of Stadt by an expert who deals with gastroesophageal reflux disease, is a new European treatment algorithm and it is based on three stages. Three stages: self-medication, treatment with a general practitioner and a specialist. I would like to point out that episodic symptoms of heartburn, which can be treated with over-the-counter drugs, such as antacids, in particular Maalox, alginates, and only then drugs from the group of proton pump inhibitors, in some cases histamine H2 blockers, are added. This is a situation that comes out at the stage of self-medication. Accordingly, if treatment is effective, it continues. If the symptoms cause concern, then you should consult a general practitioner. Alarming symptoms: dysphagia, bleeding, anemia, weight loss, suffocation, chest pain, frequent vomiting - these are moments of alarming symptoms, which, of course, require contacting a gastroenterologist.
A consultation with a therapist implies optimization and the inclusion in the first place not of antacids, but of proton pump inhibitors, which are long-acting drugs that block the secretion of hydrochloric acid. And in addition to the combination, drugs from the group of antacids are included, in particular Maalox, alginates, and the duration of this treatment is from 4 to 8 weeks. If this is a confirmed diagnosis of gastroesophageal reflux disease.
If treatment is effective, step therapy followed by discontinuation at relapse is therapy that requires tapering after 4 to 8 weeks at the lowest effective dose. If the treatment is ineffective, the dose of inhibitors is increased - not once, but twice a day and, accordingly, antacid drugs are prescribed for at least four weeks, with a re-examination and the doctor’s decision on patient management tactics. An alternative diagnosis in the absence of effectiveness should be considered and the presence of alarming symptoms requires referral to a gastroenterologist.
An appointment with a gastroenterologist, of course, optimizes therapy based on the results of the examination. Endoscopy is a mandatory test. And for non-erosive gastroesophageal reflux disease or gastroesophageal reflux disease, class A and B, respectively, include the duration of treatment, which depends on 4-8 weeks, respectively. Both class C and D are 8 weeks. Accordingly, the issue of the duration of maintenance therapy is decided depending on the effectiveness of treatment, and proton pump inhibitors in some cases are prescribed from 3 to 6 months on demand.
I would like to say that this algorithm does not imply pathogenetic treatment, but symptomatic treatment. And unlike previous algorithms, much attention is paid to drugs from the antacid group, because in this situation they are very important drugs that improve compliance.
Well, diet and lifestyle are very important points. In particular, the harmful effects of smoking should be excluded, hot and cold foods should be excluded; avoid the consumption of acidic foods, tangerines, sour fruits, foods that increase gas formation, Coca-Cola, coffee, carbonated drinks, excess fat, chocolate, spices. In particular, garlic, onions, peppers, and other spicy foods. Avoiding alcohol, especially carbonated alcohol, is also an important point; red wine is a risk factor for the development of gastroesophageal reflux disease. You should not eat several hours before bedtime or overeat. Normalizing body weight is key. And to reduce the intensity of reflux, moderate elevation of the head of the bed at night is recommended. Avoid straining the abdominal muscles, bending over, and wearing tight belts that provoke reflux. Do not assume a horizontal position after eating or eating various foods.
Regarding antacids, I would like to draw your attention to drugs from the group of combined antacids, in particular Maalox, which is capable of neutralizing hydrochloric acid, adsorbing pepsins, bile acids, and lysolecithins. And thus potentiates the cytoprotective properties on the mucous membrane. Pay attention to the safety of taking the drug, which is very important, which does not affect motor skills and does not cause electrolyte disturbances, which has been proven in a number of studies by Russian and foreign authors.
I would like to draw your attention to the fact that Maalox is a drug that has been used for quite a long time. And the work of Vladimir Trofimovich Ivashkin on the study of these properties of the drug, Trukhmanov, Maev, our famous gastroenterologists, who confirmed that magnesium and aluminum hydroxide are active components, which in interaction also have a rapid action and a delayed prolonged action of up to 3.5 hours. The acid-binding ability of this drug is much higher than its competitors, in particular calcium carbonate, magnesium oxide, sodium bicarbonate and other drugs.
Maalox has a cytoprotective effect, but one must understand that one drug will not be able to relieve heartburn in patients with gastroesophageal reflux disease and erosive esophagitis. Therefore, in an open multicenter study that was conducted, in particular published in clinical gastroenterology, I would like to draw attention to the fact that the combination with a proton pump inhibitor - Rabeprazole, Omeprazole, Esomeprazole, Lanso- and Pantoprazole - naturally, the compliance of these drugs is much higher if we We have a combination of these medications, therefore rapid healing of erosion. Effective prevention and therapy of other acid-related diseases, in particular stress-induced ulcers, are points that are very important to consider. And the rational use of drugs in the arsenal of treatment of gastroesophageal reflux disease and acid-related diseases requires, of course, a combination of these drugs.
In conclusion, I would like to say that by rationally using the capabilities of modern antacids in the treatment of non-erosive reflux disease, the doctor provides neutralizing, adsorbent and cytoprotective effects, significantly increasing the quality of life of patients. According to modern research and accumulated experience, for gastroesophageal reflux disease, monotherapy with antisecretory drugs is not always sufficient. And in most cases, it is impossible to completely relieve the symptoms of GERD without the use of antacids, one of which is the drug Maalox. As a means of pathogenetic therapy for GERD, it can be used for a long time (2-3 months). Its use gives a quick effect when we cannot quickly stop heartburn with proton pump inhibitors.
In conclusion, I would like to say that GERD has many faces. We have various manifestations and various specialties, in particular in pulmonology, cardiology, ENT specialists are currently focused on the fact that the symptoms associated with the “masks” of GERD are always very important and they can be relieved with drugs that are available not only to gastroenterologists, but also doctors of various specialties.
Complications of GERD
Gastroesophageal reflux disease can lead to the development of many dangerous complications. The most common complications are:
- chronic esophagitis;
- peptic ulcer of the esophagus;
- esophageal strictures;
- Barrett's esophagus;
- adenocarcinoma of the esophagus.
Especially often, patients with advanced forms of GERD encounter Barrett's esophagus syndrome. Abnormal columnar epithelium appears in the lower esophagus. Complications can be provoked by: lack of treatment for GERD, asymptomatic course of the disease, old age over 50 years. Barrett's esophagus has no specific symptoms. It is diagnosed during endoscopy with a biopsy of the esophageal mucosa.
GERD can cause narrowing of the esophagus as a result of scarring of the damaged lining. This complication develops mainly in older people with a long course of reflux disease. It is treated through surgery, during which an endoscopic dilation of the esophagus is performed.
Variants of the course of reflux disease
The classic version of the disease is manifested by a combination of heartburn, the frequency and intensity of which coincides with the intensity of inflammation and regurgitation. More often, exacerbations occur 1-2 times a year, but a rarely recurrent variant of the course of the disease with exacerbations once every 2-3 years can also occur.
Complications of GERD include the erosive-ulcerative variant of the disease, because it causes bleeding and perforation of the esophagus. Narrowing of the esophagus is also a serious complication of GERD.
Features of GERD in young people
In young people (under 30 years of age), the clinical picture is dominated by pain and dysphagia. Moreover, the development of the disease is often combined with dysfunction of the autonomic nervous system.
Features of GERD in older people
In older people, on the contrary, an asymptomatic or low-symptomatic course of the disease often occurs. Among the complaints, heartburn predominates, which, as the disease progresses, is joined by pain when food passes through the esophagus. Sometimes such chest pain resembles pain due to coronary heart disease.
Features of GERD in obese people
For most people with increased body weight, complaints of dysphagia come to the fore; only a third have chest pain and less than a quarter experience heartburn. This is due to the fact that against the background of obesity, the motor-evacuation function of the stomach is disrupted and gastric secretion decreases.
Features of GERD in obese people
GERD and bronchial asthma have a pronounced mutually aggravating effect. Irritation of the esophageal mucosa by acidic gastric contents causes bronchospasm, and microaspiration of hydrochloric acid into the respiratory tract can further worsen the situation. The presence of bronchial asthma, in turn, leads to a decrease in the tone of the esophagus and a more frequent occurrence of regurgitation and heartburn. Therefore, such mutual aggravating influence requires more intensive treatment of both diseases.
Features of GERD in obese people
The identification of this combination of diseases as a separate variant is due to the fact that there is drug interaction between gastric secretion blockers and antiplatelet/anticoagulant drugs. As a result of this interaction, the drug effect may be reduced, which immediately worsens the course of coronary artery disease.
Prevention of GERD
It is impossible to predict the development of gastroesophageal reflux disease in a particular person. Therefore, the disease is difficult to prevent. If there is a hereditary predisposition, it is recommended for prevention:
- eliminate physical activity that increases pressure in the peritoneum;
- lead a healthy lifestyle without bad habits;
- harden the body;
- promptly treat gastrointestinal diseases;
- regularly diagnose parasitic infestations and, if necessary, undergo treatment;
- eat properly, in portions, regularly and in a balanced manner;
- avoid stress, severe nervous shock;
- treat psychoemotional diseases.
Interesting fact: every day, more than 10% of all energy expended is spent on digesting food. It is most difficult for the gastrointestinal tract to digest alcoholic products and animal proteins. You can relieve the gastrointestinal tract by giving up alcohol and changing the way you prepare meat dishes. It is strictly not recommended to combine alcohol with fatty snacks!
Not all patients can boldly say: “I cured GERD.” An innovative approach to treatment at the ACMD clinic will help you achieve a complete recovery!
Causes of GERD
Under normal conditions, the esophagus is separated from the stomach by the cardiac sphincter, a ring-shaped muscle that closes the lumen. GERD appears when this muscle ceases to cope with its functions:
- normal motility of the gastrointestinal tract is disrupted;
- pressure inside the abdominal cavity increases;
- Sphincter tone decreases under the influence of certain medications and foods.
Experts from the World Gastroenterological Association talk about the following predisposing factors for GERD:
- excess weight (fat deposits on internal organs increase intra-abdominal pressure);
- pregnancy (increased intra-abdominal pressure combined with the influence of hormones that relax the sphincter);
- excess solid fats in food (stay in the stomach for a long time, increasing its pressure);
- love of carbonated drinks;
- other diseases of the stomach and intestines (irritable bowel syndrome, gastritis, ulcers, etc. - disrupt normal gastrointestinal motility);
- flatulence, constipation (impaired motility, increased intra-abdominal pressure);
- taking medications: aspirin, iron, potassium, tetracycline, barbiturates, estrogens (including contraceptives and hormone replacement therapy for menopause), beta blockers, tricyclic antidepressants, etc.