Bacterial vaginosis - first symptoms and treatment regimen
Bacterial vaginosis (gardnerellosis, vaginal dysbiosis, vaginal dysbiosis) is a common disease in women associated with a disruption of the normal microflora of the vagina and an increase in the number of other microbes, including gardnerella.
The nature of the disease depends on many factors, so when your health improves, the symptoms completely disappear. The disease is not sexually transmitted and does not affect men. Unprotected sexual intercourse has a certain role in the occurrence of the disease. Frequent changes of partners contribute to changes in the vaginal microflora.
Causes
To date, science does not fully have information about what actually provokes the development of non-inflammatory syndrome. However, the relevance of this problem is increasing every year.
Factors that provoke the development of the disease include:
- weakening of local and general immunity;
- poor nutrition;
- long-term antibacterial and hormonal therapy;
- frequent douching;
- the use of local contraceptives (condoms, creams and suppositories) that contain 9-nonoxynol;
- frequent change of sexual partners;
- wearing synthetic underwear;
- endocrine and gynecological pathologies;
- failure to comply with basic rules of personal hygiene;
- intestinal diseases.
Currently, bacterial vaginosis is one of the most common diseases among women of active reproductive age (from 23 to 33 years). According to statistics, about 30-35% of women suffer from vaginosis, but only half of the total number of patients know about their problem due to the presence of a characteristic odor. The rest, as a rule, don’t even know about it.
When to see a doctor
The following reasons may be reasons for contacting a gynecologist:
- You have never had an infectious disease. Your doctor will help you understand the causes and identify the symptoms.
- You have had similar diseases before, but the symptoms that arose this time are different from before.
- You have had several sexual partners or recently found a new one. Possibly a sexually transmitted disease. The signs and symptoms of some sexually transmitted infections are similar to vaginal bacteriosis.
- You tried to treat yourself and took medications, but recovery did not occur. There is a high temperature or an unpleasant vaginal odor from the vagina.
Symptoms
Often the only symptom of bacterial vaginosis is the presence of copious vaginal discharge with an unpleasant smell of stale fish, which can bother you for a long time. At the beginning of the disease, the discharge is thin, white or grayish.
The general symptoms of bacterial vaginosis are as follows:
- discharge with an unpleasant odor (fishy), which occurs as a result of the breakdown of amines produced by anaerobic bacteria.
- copious, homogeneous, creamy vaginal discharge of a grayish-white color, adhering to the walls of the vagina.
- sometimes vulvovaginal irritation appears in the form of itching and burning, discomfort during sexual intercourse.
- signs of vaginal inflammation (addition of vaginitis) are observed in half of the patients.
- rarely - urination disorders and pain in the perineum.
If the disease continues for a long time, more than 2 years, then the following symptoms occur:
- the color of the discharge becomes dark green;
- leucorrhoea changes its consistency, becomes more viscous or resembles a curdled mass;
- Also, the following signs are characteristic of discharge due to vaginal dysbacteriosis: over time they become thick and sticky, and their distribution along the vaginal walls is even. Leucorrhoea is easily removed from the walls with a cotton swab;
- with a long-term process, a number of patients complain of minor or moderate itching/burning in the vulva area (see vaginal itching);
- pain during sexual intercourse (see pain during intercourse);
- the volume of vaginal discharge reaches 0.02 liters per day (taking into account that the normal amount of leucorrhoea is no more than 2 - 4 ml);
- in a number of situations, pathogenic flora joins the described infectious process, which contributes to the development of vaginitis;
- Sometimes urinary disorders occur (frequent and painful urination in women).
A distinctive feature of the disease is the absence of visible signs of inflammation. That is, upon visual examination, a physiological pink color of the vaginal mucosa is observed. Only in some cases, single reddish dots are observed in menopausal women.
Causes of the disease and risk factors
Vaginosis is caused by the overgrowth of one of several types of organisms commonly found in the normal vaginal flora. As a rule, there are more “good” bacteria (lactobacillus) than “bad” bacteria (anaerobes) in normal conditions. But if the growth of anaerobic bacteria becomes too large, they disrupt the natural balance of microorganisms in the vagina, leading to the development of bacterial vaginosis.
Main risk factors:
- Multiple sexual partners or a new sexual partner. The relationship between sexual activity and bacterial vaginosis is not entirely clear, but bacterial vaginosis is more common in women who have multiple sexual partners or when their partners change. Bacterial vaginosis is also more common in women who have sex with other women.
- Douching. Treating the vagina with water or detergents (douching) disrupts the natural balance of the normal environment. This can lead to an overgrowth of anaerobic bacteria, which in turn causes the development of disease.
- Congenital absence of lactobacilli bacteria. If your natural vaginal environment does not produce enough lactic acid bacteria, you may be prone to bacterial vaginosis.
Severity
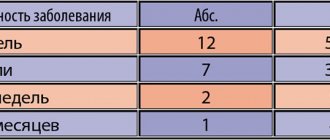
According to the severity of vaginal dysbiosis, there are:
| Compensated or 1st degree | there is no microflora in the smear, epithelial cells are present without changes and the possibility of infection with other pathogenic microorganisms remains. |
| Subcompensated or 2nd degree | the content of Doderlein bacilli decreases, gram-negative and gram-positive flora increases, there are from 1 to 5 “key” cells, a slight increase in leukocytes - up to 15 - 25. |
| Decompensated or 3rd degree | there are no lactic acid bacteria, there is a clinical picture of the disease, “key” cells entirely, various pathogenic and facultative or conditionally pathogenic microorganisms. |
According to the flow, acute, torpid or erased and asymptomatic vaginal dysbiosis is distinguished.
Diagnostics
A preliminary diagnosis of bacterial vaginosis can be made already during a gynecological examination. After the examination, discharge is taken from the posterior inferior vaginal vault.
The diagnosis can be made if 3 of the 4 listed signs are present:
- specific nature of the discharge;
- acidity >4.5 (normal 3.8-4.5);
- positive amino test;
- presence of “key” cells. The so-called “key cells” are mature epithelial cells (the superficial layer of the vaginal epithelium), on the entire surface of which microbes are densely and in large numbers attached.
Completing one of the 4 tests is not sufficient to make a diagnosis.
Complications
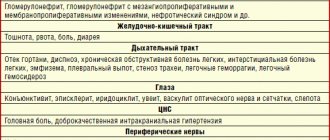
Bacterial vaginosis, as a rule, does not cause complications. But under certain circumstances, bacterial vaginosis can cause:
- Premature birth. In pregnant women, bacterial vaginosis is associated with premature birth and low birth weight babies.
- Sexually transmitted infections. Bacterial vaginosis makes women more susceptible to sexually transmitted infections such as HIV, herpes simplex virus, chlamydia or gonorrhea. If you have HIV infection, bacterial vaginosis makes it more likely that a woman will be able to infect her partner more easily.
- Risk of infectious complications after gynecological operations. Bacterial vaginosis can cause postoperative complications (eg hysterectomy).
- Inflammatory diseases of the pelvic organs. Bacterial vaginosis can cause inflammation of the pelvic organs, for example, prevention of HIV, uterus and fallopian tubes, which leads to an increased risk of infertility.
How to treat bacterial vaginosis?
Initially, a woman is prescribed antibiotics to treat bacterial vaginosis: they have a detrimental effect on nonspecific bacteria and clear the vaginal mucosa of them.
The drugs of choice are Metronidazole, Tinidazole, Clindamycin, as they are active against anaerobes. Local use of antibiotics is preferable to avoid systemic side effects, but in some cases the gynecologist is forced to resort to tablet forms.
The treatment regimen is selected individually:
- Tinidazole 2.0 in tablet form is taken orally 1 time per day for 3 days;
- Metronidazole in the form of a 0.75% gel is administered into the vagina once a day for 5 days;
- Clindamycin suppositories 100 mg are administered into the vagina once a day for 3 days;
- A cream containing 2% Clindamycin is injected into the vagina once a day for 7 days;
- Metronidazole 2.0 tablets are taken orally once.
During antibacterial therapy and a day after its completion, it is necessary to avoid drinking alcohol, even in minimal doses. The drugs disrupt the metabolism of ethyl alcohol in the body, which causes the accumulation of toxic metabolites and severe intoxication. In its course, it resembles a severe hangover: the woman experiences severe weakness, limbs shake, blood pressure rises, a severe throbbing headache occurs, and painful nausea and vomiting develop.
Clindamycin cream contains fat, so it can damage the condom or latex contraceptive membrane. All local forms of drugs are administered immediately before bedtime to prevent them from flowing down the vaginal walls.
If antibiotics are intolerant or there are contraindications to their use, the first stage of treatment is carried out with local antiseptics:
- Hexicon 1 suppository is administered 2 times a day for 7-10 days;
- Miramistin in the form of a solution is irrigated into the vagina once a day for 7 days.
Preparations for bacterial vaginosis, used in the second stage of treatment, contain lactobacilli and create favorable conditions for restoring the vaginal microflora. They are used 2-3 days after completion of antibacterial therapy:
- Acylact 1 suppository 2 times a day is inserted into the vagina for 5-10 days;
- Bifiliz 5 doses are taken orally 2 times a day for 5-10 days.
Antifungal suppositories for bacterial vaginosis are usually not prescribed. The need for them arises if candidiasis, a fungal infection, joins the opportunistic microflora. In this case, Clotrimazole suppositories are prescribed intravaginally once a day for 6 days.
Treatment
Treatment of this pathology is carried out in stages:
- Stage I – reducing the level of pathogenic microorganisms. Antibacterial therapy is used for these purposes;
- Stage II – restoration of the vaginal microflora. In this case, probiotics, suppositories with lactobacilli, and immunomodulators are used.
A control smear is prescribed after one and a half to two months. Until then, it is recommended to use condoms during sexual intercourse.
Possible treatments:
- The “Gineton” device is a low-frequency ultrasound, the effect of which is the basis of this hardware technique, which eliminates the source of infection and improves the penetration of drugs into tissues.
Treatment of pregnant women
Therapeutic therapy during pregnancy differs from the standard regimen in that:
- Antibiotics are not prescribed;
- Treatment is carried out after the first trimester.
Treatment during pregnancy
How to treat bacterial vaginosis in case of pregnancy? In the first trimester of gestation, systemic therapy for the disease is not performed (metronidazole and other drugs are toxic to the embryo). Local administration of etiotropic drugs in the early stages is used with caution.
Taking metronidazole or clindamycin begins in the second trimester and is carried out in short courses. Metronidazole 0.5 g. (2 tablets) twice a day for 3–5 days, and clindamycin is prescribed in a dosage of 0.3 g. 2 times a day for 5 days.
Pregnancy complications that may occur due to the disease include:
- miscarriage - loss of a fetus during the first 23 weeks;
- premature birth - when a baby is born before the 37th week of pregnancy;
- chorioamnionitis - infection of the chorion and amnion membranes (the membranes that make up the fetal sac) and amniotic fluid (the fluid surrounding the fetus);
- premature rupture of the amniotic sac - a bladder containing fluid in which the fetus develops;
- postpartum endometritis - infection and inflammation of the uterine tissue after childbirth.
If you are pregnant and experience symptoms of vaginosis, contact your gynecologist as soon as possible. Although the risk of complications is low, treatment will help reduce it further.
Treatment of gardnerellosis
Treatment in men requires complete elimination of Gardnerella from the genital tract. For this purpose, antibiotics of the 5-nitroimidazole group (Tinidazole, Clindamycin, etc.) are prescribed. If no other infection (except Gardnerella) is detected, the treatment regimen includes only one drug, and the course lasts 3/5/7 days.
You need to understand that contact with a bacterium is not accompanied by the development of immunity against it. Upon completion of the therapeutic course, an episode of gardnerellosis may recur. To prevent reactivation of Gardnerella, both partners should undergo treatment, and the woman should pay attention to measures to prevent relapses of bacterial vaginosis.
Protection against complications developing against the background of diseases of the male genital area requires an annual visit to a urologist. Highly qualified specialists conduct consultations at the medical clinic. At the clinic you can be tested for gardnerellosis and receive recommendations regarding the prevention and treatment of sexually transmitted infections.
Prevention
The recommendations are as follows:
- using barrier methods of contraception, wearing underwear only made from natural fabrics;
- regular examination by a gynecologist and timely treatment of diseases;
- treatment of chronic pathologies of internal organs;
- strengthening the immune system in natural ways: physical activity, hardening, etc.;
- avoiding douching and other similar procedures.
Bacterial vaginosis is a pathology that reflects a decrease in the body’s level of defense at the moment. Often occurring asymptomatically, gardnerellosis is always detected during examination by a gynecologist. Only a doctor can prescribe the most effective tablets for bacterial vaginosis, suppositories or other forms. Don't delay treatment!
Diagnosis of gardnerellosis in men
If you have signs of the disease, you should contact a urologist. Diagnostics includes the following steps:
- Survey. The doctor clarifies complaints, collects anamnesis, clarifies the features of a man’s sexual life (presence of a regular partner, contraceptive methods used, etc.)
- Laboratory diagnostics. The urologist takes a swab from the urethra. A bacterioscopic examination allows you to identify signs of concomitant inflammation and exclude the most common sexually transmitted infections. Gardnerella in men is detected by PCR.
- Instrumental diagnostics. The doctor prescribes an ultrasound if he suspects the involvement of the pelvic organs in the pathological process.
If necessary, the urologist may recommend consultations with other specialists (therapist, endocrinologist, etc.)