Ovestin suppositories and cream are a hormonal French medicine for replenishing female hormones during the postmenopausal period, treating synechia for children, before surgical operations. Contains estriol, prohibited for oncology and some other diseases (a full description of contraindications is contained in the original instructions for use of the medicine).
Due to the high cost, large number of restrictions and contraindications, and possible adverse reactions, analogues of Ovestin cream and suppositories are prescribed. Another limitation and factor in the need to select substitutes is pregnancy or a sudden onset during treatment.
pharmachologic effect
The medicine is available in three forms - tablets, cream or suppositories. Contains estriol, a substance that is an analogue of the natural female hormone. When used as a course, it has the following therapeutic effects:
- reduction of postmenopausal symptoms and elimination of estrogen deficiency (disorders of the nervous and cardiovascular systems, osteoporosis, deterioration of skin, hair, nails);
- improvement of the condition of the mucous membrane of the genitourinary system;
- improvement of vaginal microflora;
- strengthening local immunity, cell resistance to infections and inflammation, preventing vulvovaginitis;
- preventing urinary incontinence, improving the urination process;
- reduction of itching and dryness of the vagina, pain during sexual intercourse.
Urogenital disorders in postmenopause and hormone replacement therapy
Changes in the demographic structure of society in the second half of the 20th century. led to an increase in the proportion of women in the older age group in the population. The number of women entering menopause increases every year. If 75 years is taken as 100%, then the duration of the prepubertal period is 16%, the reproductive period is 44%, the premenopausal period is 7%, and the postmenopausal period is 33% (H. Haney, 1986). That is, a woman spends more than a third of her life in a state of deficiency of female sex hormones. Menopause, while not being a disease itself, leads to disruption of the endocrine balance in a woman’s body, causing hot flashes, irritability, insomnia, urogenital disorders, and also increasing the risk of developing osteoporosis and cardiovascular diseases. All these data indicate the need to develop a number of medical and social measures to protect the health, maintain productivity and a decent quality of life for peri- and postmenopausal women.
In recent years, the problem of urogenital disorders has become a leader in the symptomatology of menopausal disorders, which is associated with their pronounced negative impact on the quality of life of postmenopausal women. The incidence of age-related urogenital disorders reaches 30%. In the perimenopausal period, urogenital disorders occur in 10% of women, while in the age group of 55-60 years - in 50%. By the age of 75, 2/3 of women already experience urogenital discomfort, and after 75 years it is difficult to meet a woman who has not experienced individual symptoms of urogenital disorders.
Urogenital disorders in menopause are a symptom complex of secondary changes associated with the development of atrophic and dystrophic processes in estrogen-dependent tissues and structures of the lower third of the genitourinary tract, bladder, urethra, vagina, pelvic ligaments and pelvic floor muscles.
A progressive increase in the incidence of urogenital atrophy with age is associated with irreversible age-related metabolic changes that develop against the background of estrogen deficiency. The vagina, urethra, bladder and lower third of the ureters have a single embryonic origin and develop from the urogenital sinus. This explains the presence of receptors for estrogen, progesterone and androgens in the muscles, mucous membrane, choroid plexuses of the vagina, bladder and urethra, as well as in the muscles and ligaments of the pelvis.
The aging processes of the urogenital tract develop in two directions:
- predominant development of atrophic vaginitis;
- predominant development of atrophic cystourethritis with or without symptoms of impaired urinary control.
Atrophic vaginitis occurs as a result of estrogen deficiency and is characterized by a sharp thinning of the vaginal mucosa, cessation of proliferative processes in the vaginal epithelium, a decrease in glycogen production by epithelial cells, a decrease or complete disappearance of lactobacilli, and an increase in vaginal pH (see Table 1).
The main clinical manifestations of atrophic vaginitis are vaginal dryness and itching, recurrent discharge, dyspareunia, and contact bleeding.
Diagnosis of atrophic vaginitis includes:
- The patient complains of dryness and itching in the vagina; recurrent discharge, often regarded as a symptom of recurrent colpitis; contact bleeding.
- objective examination methods: extended colposcopy: thinning of the vaginal mucosa, bleeding, petechial hemorrhages, numerous translucent capillaries are determined; colpocytological study - determination of the karyopyenotic index (KPI), which decreases to 15–20 with the development of atrophic processes in the vagina, or determination of the maturation index (MI). IS is assessed by a shift in the formula: a shift in the formula to the left indicates atrophy of the vaginal epithelium; Determination of vaginal pH - Vaginal pH in untreated postmenopausal women is 5.5–7.0 depending on age and sexual activity. In sexually active women, the pH is slightly lower. The higher the pH, the greater the degree of atrophy of the vaginal epithelium.
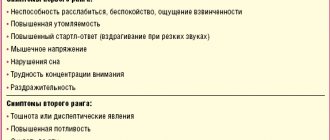
Manifestations of atrophic cystourethritis include “sensory” or irritating symptoms:
- cystalgia - frequent, painful urination during the day, accompanied by a burning sensation, pain and cutting in the bladder and urethra;
- pollakiuria - increased urge to urinate (more than four to five episodes per day) with the release of a small amount of urine with each urination;
- nocturia - increased urge to urinate at night (more than one episode of urination per night);
- stress urinary incontinence (during physical activity, coughing, sneezing, laughing, sudden movements, lifting weights);
- urinary incontinence (urine flows out without strain due to imperative urges).
Examination of women with urinary disorders:
- patient complaints;
- Valsalva test - a woman with a full bladder in a position on a gynecological chair is asked to forcefully push. The test is considered positive if drops of urine appear in the area of the external urethral opening;
- cough test - a woman with a full bladder in a position on a gynecological chair is asked to cough. The test is considered positive if urine leaks when coughing;
- pad test - the weight of the pad is determined after an hour of exercise. If the weight of the pad increases by more than 1 g, then urinary incontinence occurs;
- urine culture for infection and sensitivity to antibiotics;
- urodynamic examination (carried out by urologists) - uroflowmetry, cystometry, urethral profilometry, electromyography.
The identification of the symptoms of atrophic vaginitis and cystourethritis is conditional, since in most cases they are combined. Various combinations of symptoms of atrophic vaginitis and cystourethritis made it possible to distinguish three degrees of severity of urogenital disorders (V. E. Balan, 1997).
Mild urogenital disorders (16% of women) include a combination of symptoms of atrophic vaginitis and “sensory symptoms” of atrophic cystourethritis without disturbance of urination.
Moderate urogenital disorders (80% of women) include a combination of symptoms of atrophic vaginitis, cystourethritis and true stress urinary incontinence.
Severe urogenital disorders (4% of women) include a combination of symptoms of atrophic vaginitis, cystourethritis, true stress urinary incontinence and urinary incontinence.
So, it has been established that estrogen deficiency is the cause of the development of urogenital disorders in women during menopause. The problem of treating urogenital disorders is controversial. The emphasis is on what type of hormone replacement therapy (HRT) is considered optimal. HRT for urogenital disorders can be carried out with drugs that have both systemic and local effects. Systemic HRT includes all drugs containing estradiol, estradiol valerate and conjugated estrogens.
Local HRT includes drugs containing estriol. The choice of the type of HRT for the treatment of urogenital disorders is individual and depends on the patient’s age, duration of postmenopause, leading complaints, the need to treat menopausal syndrome or prevent late metabolic disorders.
The prescription of systemic HRT must comply with generally accepted rules, taking into account absolute and relative contraindications. When prescribing HRT to patients with urogenital disorders, the goal is to restore the normal state of local hormone-dependent structures of the lower parts of the genitourinary system and stimulate biological tissue defense mechanisms.
When deciding on the type of drug for HRT, it is extremely important to determine:
- menopause phase - perimenopause or postmenopause;
- whether we are talking about an intact uterus or the uterus is absent (if absent, then why was the hysterectomy performed).
For an intact uterus, combination therapy with drugs containing estrogens and gestagens is used:
- in perimenopause - two-phase drugs (Climen, Klimonorm, Divina, Cycloproginova, Femoston, etc.) or three-phase drugs (Trisequence);
- in postmenopause - combined monophasic drugs in a continuous mode (Cliogest, Gynodian-Depot, Livial, Climodien, Pausogest, Femoston, etc.).
In women after hysterectomy, systemic exposure is provided by monotherapy with natural estrogens in a cyclic or continuous mode (estrophem, progynova, climara, divigel, estraderm).
A priority role in the choice of HRT for urogenital tract disorders caused by decreased gonadal function belongs to estriol-containing drugs that have selective activity in relation to the genitourinary system. The specificity of the action of estriol is determined by the characteristics of its metabolism and affinity with the corresponding receptor systems. The local effect of steroid hormones is realized through their passive diffusion into the cells of the body. Retaining only in the cells of sensitive tissues, they form complexes with cytosolic receptors, followed by translocation into the cell nucleus. In this way, the action is realized at the level of the genetic structures of the cell. This determines the specificity of the effect characteristic of a given tissue.
The response of tissues to the effects of estrogens is determined by the concentration of receptors, their structure and properties of estrogens. Estriol is the final metabolite in estrogen metabolism. It is excreted from the body in conjugated form in the urine and only in small quantities is excreted in feces, mainly in unconjugated form.
When estriol is administered orally, its maximum concentration in the blood plasma is reached after 1-2 hours. Estriol that enters the blood plasma does not bind to sex steroid-binding globulin and is eliminated quite quickly. Estriol is the least active estrogen with a short-term effect.
It has been established that tissues sensitive to estriol are widely represented in the lower parts of the urogenital tract. Estriol therapy promotes the development and restoration of the vaginal epithelium, and also leads to the restoration of the main elements of connective tissue - collagen and elastin. At the same time, the main thing in prescribing estriol-containing drugs is minimal systemic effect. It is known that to stimulate the development of the endometrium, the connection of its receptors with estrogen must be long-lasting, at least 8-10 hours. Estriol binds to structures sensitive to it for no more than 2-4 hours. Such a short-term effect is not enough for the proliferative reaction of the endometrium, but sufficient to effectively influence the structures of the lower parts of the urogenital tract. Thus, with a single administration, estriol binds to the nuclear receptor for a short time and does not cause endometrial proliferation, therefore, when administered, the addition of progestogens is not required.
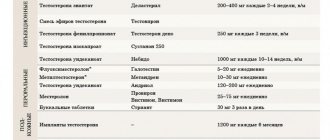
For urogenital disorders, preference is traditionally given to local administration of estrogens and specifically estriol (Ovestin) in ointments and suppositories (see Table 2).
In any form, estriol-containing preparations are taken once a day. The combination of systemic and local forms of the drug is not recommended.
The choice of therapy also depends on the severity of urogenital disorders.
For mild urogenital disorders, estriol preparations (suppositories, cream) are used daily or three times a week, depending on the severity of clinical symptoms. When the phenomena of atrophic vaginitis or atrophic cystourethritis are combined with menopausal syndrome, drugs for systemic HRT are prescribed.
For moderate severity of urogenital disorders, combined therapy (systemic and local) is carried out for at least six months to normalize urodynamic parameters.
In case of severe urogenital disorders in the case of existing indications for systemic HRT, combination therapy with drugs for systemic HRT is carried out in combination with local administration of estriol drugs and one of the additive drugs that have a selective effect on cholinergic (parasympathetic) and adrenergic (sympathetic) or muscarinic receptors, located in the muscular wall of the bladder and various structures of the urogenital tract: the smooth muscle of the urethra and the pelvic floor muscles involved in creating urethral support. Combination therapy must be carried out for six months or more, after which the question of the type of therapy is decided individually for each patient (see Table 3).
| Table 3. Treatment regimen for urogenital disorders. |
This system of differentiated HRT can improve the quality of life of patients with urogenital disorders by 60-70%.
Thus, the presented data allow us to talk about HRT as the main treatment for urogenital disorders in postmenopause.
Due to the progressive nature of urogenital disorders, preference is given to the prophylactic use of HRT and its long-term use. HRT for urogenital disorders should be prescribed for a long time, almost for life, and in this situation it is local therapy with estriol that comes to the rescue.
Today, modern medicine has a fairly wide selection of good drugs for HRT and experience in their use, indicating that the benefits of prescribing HRT significantly outweigh the risk of side effects. All this gives reason to recommend the widespread use of HRT for the prevention and treatment of urogenital disorders in peri- and postmenopause in order to improve the quality of life and preserve the working capacity of women entering this “autumn” period.
A. L. Tikhomirov, Doctor of Medical Sciences, Professor Ch. G. Oleinik, Candidate of Medical Sciences MGMSU, Moscow
Literature:
- Balan V. E.//Gynecology. - 2000. - No. 5; 2. - pp. 140-142.
- Balan V. E., Ankirskaya A. S., Yesesidze Z. T., Muravyova V. V. //Consilium medicum. 2001; No. 7; 3. - pp. 326-331.
- Kulakov V.I., Smetnik V.P. //Guide to menopause. - M., 2001. - 685 p.
- Romanyugo N.N.//Practical gynecology. - 1999. - No. 1; 1. - pp. 28-29.
- Alsina CJ //Maturitas. 1996; 33; 51-57.
- Crook D., Godsland IF //Br. J. Obstet. Gynaecol. 1997; 104; 298-304.
- Heikkinen JE, Vaheri RT //Am. J. Obstet. Gynecol. 2000; No. 3; Vol. 182; 560-567.
- Pickar JH //Am. J. Obstet. Gynecol. 1998; 178; 1087-1099.
- Samsioe G. //Menopause Review. 1998; 3 (1); 9-17.
Indications for use of Ovestin
Suppositories and cream are intended to replenish estriol and estrogen deficiency in the following cases:
- atrophy of the mucous membrane of the genitourinary tract during postmenopause, caused by hormone deficiency;
- the need for vaginal access during surgery;
- to obtain a diagnostic picture when taking a cervical smear;
- fusion of the labia or synechia in girls.
The tablets have additional indications - reducing the symptoms of menopause, some types of infertility, complaints of pain during sex, vaginal itching and a feeling of dryness.
Basic instructions
Hormone replacement therapy with Ovestin for the treatment of signs of menopause is carried out only for symptoms that negatively affect the quality of life. But before this, the specialist evaluates the benefits and all the risks.
At the very beginning of hormone therapy, the doctor collects information from the patient and his family about:
- history of pathologies;
- past illnesses;
- living conditions.
After clarifying the medical history, women's mammary glands and pelvis are examined. During the therapy itself, medical examinations are also periodically carried out. All examinations, including mammography, must comply with generally accepted standards.
Ovestin cream (analogs are cheaper or their group copies are usually prescribed by specialists for local therapy during menopause in women) and its substitutes compensate for the lack of estrogen during menopause. At the same time, atrophy of the mucous membranes of the urinary tract is also treated.
During therapy with Ovestin, patients are continuously monitored with:
- cholelithiasis;
- pancreatitis;
- endometriosis;
- familial hyperlipoproteinemia;
- fibroid or myoma of the uterus;
- otosclerosis;
- previous thromboembolism;
- asthma;
- risk of breast cancer;
- epilepsy;
- arterial hypertension;
- endometrial hyperplasia;
- liver adenoma;
- systemic lupus erythematosus;
- diabetes mellitus;
- severe headaches.
Treatment with hormones is immediately canceled if:
- pregnancy;
- deterioration of liver function;
- migraines;
- strong increase in pressure.
The drug with estriol succinate is not prescribed:
- people with a tendency to allergies;
- uncontrolled in patients with cardiovascular insufficiency and renal impairment;
- as contraception;
- women who are over 65 years of age due to their risk of developing dementia.
Ovestin - instructions for use
Ovestin ointment and suppositories are over-the-counter products; tablets are used after examination by a gynecologist. However, before using approved products, it is important to visit a specialist, read the instructions, and if there are contraindications, find out what to replace Ovestin cream or other forms of release with.
The tablets are used in the prescribed dosages at the same time, preferably in the evening. The course depends on the indications and condition of the patient.
The cream is administered using a calibrated applicator, which is then treated with water. Suppositories are inserted into the vagina at night.
In childhood, especially for the treatment of synechia, it is necessary to consult a specialist. In case of synechia, it is better not to wash yourself with soap or intimate hygiene products, replacing the procedure with plain water.
Ovestin's analogues
If it is impossible to purchase an expensive drug, there are contraindications and restrictions, or adverse reactions occur after use, it is possible to search for an alternative - cheaper Ovestin analogues:
- Orniona;
- Ovipol Clio;
- Trioginal;
- Ovanelia;
- Estrovagin;
- Estrocad;
- Gynoflor E.
Prices for Ovestin and analogues in Moscow are presented for informational purposes only; they may vary in different cities and pharmacy organizations.
| Analogue | Price, in rubles | Manufacturer country |
| Ovestin tablets | 1150-1450 | Spain |
| suppositories | France | |
| cream | 1350-1700 | |
| Orniona | 650-1000 | Russia |
| Ovipol Clio | 550-750 | Russia or Republic of Moldova |
| Trioginal | 800-1100 | France |
| Gynoflor E | 650-900 | Switzerland |
| Ovaneliya | currently not available from suppliers | Russia |
| Estrovagin | 240-400 | Russia |
| Estrocade | 550-850 | Germany |
| Divigel | 600-900 | Finland |
Gynoflor E
A combined cheap analogue in suppositories, aimed at eliminating disturbances in the vaginal microflora and preparing for surgery. Contains estriol and lactobacilli acidophilus. Sold in pharmacies without a doctor's prescription.
Ovaneliya
An over-the-counter domestic drug based on estriol in the form of suppositories. Is a cheap generic or reproduction of suppositories.
Russian analogues are an opportunity to compensate for the lack of hormones at a lower cost.
Estrovagin
An analogue of Ovipol Clio, Estrocade and Ovanelia in the form of candles with a low price - up to 6-7 times cheaper. The difference is prescription.
Estrogial
The cream is an analogue of Ovestin, the price is up to 2 times lower (from 550 rubles). It contains sodium hyaluronate and a natural phytocomplex aimed at eliminating dryness, itching, and discomfort in the vagina. Reduces inflammation, irritation, deodorizes and heals. It belongs to the group of “Non-hormonal analogues of Ovestin cream”.
When choosing between Ovestin or Estrogial cream, it is better to buy the latter. Natural composition, fewer contraindications and side effects, inexpensive course of treatment - the advantages of the analogue.
Divigel
A cheap source of estrogen, it is a gel in two dosages in bags. Indicated in preparation for operations, to replenish hormones.
Price of funds
Information on the price of Ovestin and its substitutes can be found in the following comparative table:
| Name of the drug with estriol | Cost, rub. |
| Ovestin (cream) | 1030-1200 |
| Orniona (cream) | 660-800 |
| Estrovagin (suppositories) | 240-490 |
To get rid of hormonal deficiency during menopause, instead of artificial drugs with estriol, you can use phytoestrogens, which are found in:
- flax seeds;
- shepherd's purse;
- hawthorn;
- Siberian ginseng;
- clover;
- hog uterus;
- linden flowers and chamomile;
- parsley;
- sage;
- licorice root.
To maintain optimal estrogen levels, women are advised to eat:
- vegetable fats in the form of oils;
- beans and soybeans;
- celery and cabbage;
- carrots and asparagus;
- garlic;
- cereals;
- kefir and cheese;
- cottage cheese.
To prevent menopause syndromes, women need to:
- exercise regularly;
- check your blood for sugar and cholesterol every 6 months;
- control body weight;
- constantly measure blood pressure (2 times a day);
- give up bad habits;
- be examined by a gynecologist every 6 months;
- independently check the condition of the mammary glands, and also regularly visit a mammologist.
Non-drug treatments for estrogen deficiency in women include:
- eating food with phytohormones;
- using relaxation techniques to combat stress;
- wearing comfortable clothing to ensure good ventilation;
- constant walking or swimming;
- a healthy lifestyle without bad habits and with quality nutrition.
The female genital area is very sensitive to inflammation and infections, so it needs special support, which can be an intravaginal cream called Ovestin. This drug is also actively used after surgical interventions in the perineal area and for the treatment of synechiae in children. The medication is sometimes replaced with cheaper analogues.
Orniona or Ovestin - which is better?
Orniona is a cheap substitute for Ovestin in the form of a cream, the price is up to 50% lower depending on the city and the chosen pharmacy. Contains estriol in the same concentration. The difference is in the country of origin. The analogue is a domestic drug for the treatment of diseases of women and conditions associated with estrogen deficiency. Also available without a prescription.
When choosing between Ornion or Ovestin, you can take any cream according to your financial capabilities and the preference of the manufacturer - foreign or domestic.
Triozhinal or Ovestin - which is better?
Triozhinal is a complex medication consisting of estriol, progesterone and a culture of lactobacilli. It is aimed at replenishing hormones, improving and normalizing the microflora and acidity of the vagina. Indications for use include preparation for surgery and atrophic vulvovaginitis caused by a lack of hormones.
When choosing, you should take into account that the analogue is available by prescription and has a strong composition.
Analogues of Ovestin cream based on estriol cannot be used when planning and becoming pregnant. In these cases, it is advisable to consult a gynecologist in advance.