Anxiety disorders and experience with paroxetine
Anxiety disorders are extremely common, with 13–25% of the population experiencing anxiety disorders in their lifetime. According to the DSM-IV (Diagnostic and Statistical Manual) classification, anxiety disorders include [10]:
- panic disorder;
- generalized anxiety disorder;
- agoraphobia without panic disorder;
- obsessive-compulsive disorder;
- social phobia;
- specific phobias;
- post-traumatic stress disorder;
- acute stress disorder.
Many people are familiar with the symptoms of anxiety. They can be divided into general (mental and vegetative) and specific, determining the type of anxiety disorder. Common mental symptoms include restlessness, irritability, anxious thoughts, motor agitation, flinching at sudden sounds, decreased concentration, increased fatigue, impatience, inability to relax, sleep disturbances, and nightmares. The anxious mood is perfectly conveyed in Edvard Munch’s painting “Anxiety” (Fig. 1).
As a rule, mental symptoms of anxiety are accompanied by vivid vegetative symptoms. Thus, the face of the woman depicted in the picture is pale, tense, and her lips are dry. She keeps her hands on her neck. Perhaps this is a feeling of shortness of breath, a coma in the throat and a feeling of chills. Other autonomic symptoms of anxiety include tachycardia, increased sweating with cold, clammy palms, hot flashes or chills, dyspeptic disorders (abdominal pain, flatulence, diarrhea), dizziness, increased urination, increased physiological tremor, and increased muscle tone.
Clinical forms of anxiety disorders
Generalized anxiety disorder (GAD) is one of the most common forms of anxiety, with 4–9.2% of the population experiencing it during their lifetime [20]. The DSM-IV criteria for GAD are the presence of anxiety and restlessness in combination with at least three of the following symptoms:
- impatience or feeling on edge;
- increased fatigue;
- difficulty concentrating or feeling empty in the head;
- irritability;
- muscle tension;
- sleep disorders.
The duration of the disease must be at least 6 months, the symptoms must cause significant distress or affect social, professional and other areas of activity.
Panic disorder is also extremely common: according to epidemiological studies, panic attacks are observed in 1.5–4% of the population [11], although 35.9–46% of the human population have experienced panic at least once in their lives [2]. Panic disorder affects 6% of people seeking primary care [2]. The main clinical manifestation of panic disorder is panic attacks - attacks of severe anxiety, accompanied by somatic and cognitive symptoms. The main diagnostic signs of panic attacks are paroxysmal occurrence, polysystemic vegetative symptoms, and the presence of emotional disorders, the severity of which can range from a feeling of “discomfort” to “panic” [2]. Agoraphobia is very similar to panic disorder and is defined as anxiety that occurs in response to situations in which the solution is difficult or difficult, or when help will not be available if a panic attack develops. If anxiety in panic disorder can be defined as anxiety in anticipation of a subsequent attack, then agoraphobia is characterized by the presence of provoking factors or situations - being alone outside the house, being in a crowd, on a bridge (as in a Munch painting), traveling on public transport, etc. Provoking situations are actively avoided by patients; getting into them is accompanied by significant distress.
Specific phobias are characterized by the connection of anxiety with certain situations (air travel, contact with animals, the sight of blood, etc.), also accompanied by an avoidance reaction. Finding yourself in a phobic situation provokes an anxious reaction, similar to a panic attack. Patients are critical of their experiences, however, phobias have a significant impact on various areas of the patients’ activities. An example of a specific phobia can be found in the famous artist Pablo Picasso. “For a long time he was deathly afraid of getting his hair cut. For months I wore my hair too long and was hesitant to go to the hairdresser. As soon as someone started talking about it, he fell into a real panic. As a rule, it ended with him asking his loved ones to shorten his hair or locking himself in a small room and trying in vain to cut off his hair himself” [3, 11].
Social phobia is characterized by the occurrence of anxiety in social situations - communication and self-presentation (public speaking or even being in public), fear of possible condemnation from others. As with other anxiety disorders, patients actively avoid social situations because the anxiety causes them significant distress. Thus, the Russian critic and publicist V. G. Belinsky writes: “One thing torments me terribly: my timidity and embarrassment do not weaken, but increase in monstrous progression. I can’t show myself in public: my face is flaring up, my voice is trembling, my arms and legs are shaking, I’m afraid of falling. Self-affirmation is carried out in forms that are in every possible way opposed to accepted norms of behavior. Hence the eccentricity, wildness, and absurdity” [7, 11].
Obsessive-compulsive disorder is characterized by the presence of intrusive thoughts (obsessions) that increase anxiety and ritual actions or thoughts aimed at suppressing this anxiety. There are two key characteristics of symptoms in obsessive-compulsive disorder: egodystonia (the patient is unable to ignore or suppress the symptoms, although he is fully aware of their absurdity) and the presence of significant distress for a significant time (more than an hour a day). The most common obsessions are fear of contamination (45%), pathological doubts (42%), somatic obsessions (36%), the need for symmetry (31%), aggressive impulse (28%), sexual impulse (26%) [14]. Among the compulsions, the most common are checking (60%), washing (50%), counting (36%), the need to ask or admit something (31%), the need for symmetry/neatness (28%), hoarding (18%). ). Distinctive features of obsessive-compulsive disorder from other forms of anxiety disorders are an earlier age of onset, equal representation among both sexes (other forms of anxiety are more common in women), and a fairly high resistance to serotonergic drugs.
Post-traumatic stress disorder has 17 core symptoms, grouped into three groups: re-experiencing the trauma (instructive thoughts, nightmares, emotional and somatic reactions in response to memories), avoidance of memories associated with the trauma (avoidance of thoughts, feelings, places, acquaintances, inability to remember details of a situation, decreased interest in entertainment, withdrawal from other people, lack of prospects for the future) and agitation (sleep disturbances, irritability, difficulty concentrating, hypervigilance and increased startle reflex).
Difficulties in diagnosing anxiety disorders
The main reasons for underdiagnosis of anxiety disorders are the presence of subsyndromal forms of anxiety, as well as a wide range of comorbid disorders - depression, chronic pain syndromes, and other forms of anxiety disorders.
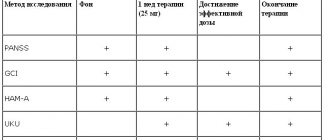
Diagnostic criteria for anxiety disorders are widely presented in the literature and are known to practicing physicians. However, in their daily practice, neurologists and internists much more often see not developed, but subsyndromal forms of anxiety disorders, when in the clinical picture of the disease it is not the mental, but the somatic or neurological components of anxiety that come to the fore. Thus, in the case of GAD, the DSM-IV diagnostic criteria have a significant drawback - they are mainly focused on the presence of mental symptoms, which can lead to underdiagnosis of the anxiety disorder. In the ICD-10 criteria, to make a diagnosis of GAD, the presence of 4 symptoms out of 22, divided into five groups - vegetative, respiratory or gastrointestinal symptoms, symptoms affecting mental activity, general symptoms and nonspecific symptoms, is required, but internists and doctors It is not always convenient for other specialties to use ICD-10 criteria. Starcevic V. et al. identified the most significant symptoms of GAD from the DSM-IV and ICD-10 classifications. The criteria proposed by the authors are much more convenient to use in everyday practice (
.) [18].
Recent epidemiological studies have shown a high prevalence of subsyndromal panic disorder that does not meet diagnostic criteria. In these cases, panic attacks, although rare, anxiety also significantly affects the lives of such patients [15]. Certain diagnostic difficulties can be caused by atypical panic attacks when clinical phenomena not covered by DSM-IV criteria are observed during an attack—diffuse or local pain syndromes, senestopathies, muscle tension, obsessions and compulsions, etc. [2]. There are 10 atypical, conversion symptoms of panic attacks: (1) feeling of a lump in the throat, (2) feeling of weakness in an arm or leg, (3) visual or hearing impairment, (4) gait disturbance, (5) speech or voice disturbance, ( 6) loss of consciousness, (7) a feeling that the body is arching, (8) cramps in the arms and legs, (9) nausea, vomiting, (10) abdominal discomfort [2].
When making a diagnosis of agoraphobia, it is necessary to remember that in cases where the patient has only one or two anxiety-provoking situations, it is necessary to think about specific phobias, and if the anxiety is associated only with social triggers, then about social phobia.
Another feature of panic disorder and agoraphobia is the presence of permanent autonomic disorders, which can occur predominantly in one system or be multisystem in nature [2]. These disorders can be the reason for contacting specialists of various profiles. Thus, patients can come to see a cardiologist with cardialgia, cardiosenestopathies, arterial hypo- and hypertension, syncope and lipothymic conditions, a feeling of lack of air, a feeling of suffocation, and Raynaud's syndrome. Gastroenterologists may encounter in their practice patients who persistently complain of dyspeptic symptoms, dry mouth, nausea, abdominalgia, constipation or diarrhea. Such patients should always request that their anxiety disorder be excluded.
Like other anxiety disorders, obsessive-compulsive disorder is underdiagnosed. Typically, patients with obsessive-compulsive disorder are embarrassed to talk about mental symptoms, even when asked about them directly. The following 5 questions can help a practitioner diagnose this type of anxiety disorder [19]:
- Do you wash or clean things a lot?
- Do you check something over and over again?
- Do you have thoughts that bother you that you would like to get rid of, but you can’t?
- Do your daily activities take up a lot of your time?
- Is your attention focused on any order or symmetry?
Depression is an integral accompaniment of anxiety. Anxiety disorders occur in 57% of patients with depression [15]. The combination of anxiety and depression significantly aggravates the course of the disease. This is manifested by more severe symptoms, a tendency to chronicity, mental dysfunction, refusal to work, greater seeking of medical help, a greater risk of suicide and resistance to therapy.
Paroxetine in the treatment of anxiety disorders
Drugs of various pharmacological groups are used to treat anxiety disorders. However, antidepressants are currently considered the drugs of choice. Widely used until recently, anxiolytics, most of which are benzodiazepines, are not used as a basic drug, primarily due to frequent complications: sedation, behavioral toxicity, paradoxical reactions, tolerance, addiction, dependence, withdrawal and rebound syndrome, as well as the presence of drugs interactions. Among antidepressants, preference should be given to selective serotonin reuptake inhibitors (SSRIs) as they are effective and the most well tolerated drugs. Among the SSRIs, paroxetine is the most studied drug in the treatment of anxiety disorders.
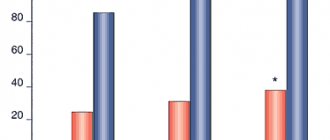
For GAD, paroxetine has shown its effectiveness both in comparison with placebo and tricyclic antidepressants and benzodiazepines [17]. Thus, among patients receiving paroxetine, remission was achieved in 72%, while among patients receiving placebo, only 34% (p < 0.001). Already at 4 weeks of use, paroxetine significantly improved the level of anxiety on the HAM-A scale by 15.6 points compared to benzodiazepine, which improved the anxiety score by only 11.8 points (p < 0.01). The dose of paroxetine effective for the treatment of GAD is 20–40 mg/day (10–50 mg/day) [17].
Paroxetine is the most studied drug in the treatment of panic disorder and agoraphobia. In a large placebo-controlled study, paroxetine was effective compared with placebo, characterized by the occurrence of an attack-free period, at a dose of 40 mg/day (p < 0.02). Thus, when taking paroxetine, an attack-free period occurred in 86% of patients, and when taking placebo - in 50%. Paroxetine also had a significantly lower relapse rate (5%) compared to placebo (30%), p = 0.002 [16].
Studies have also been conducted on the effectiveness of paroxetine for social phobia and post-traumatic stress disorder. Among patients with social phobia, 55% of patients taking paroxetine and 24% of patients taking placebo were responders. In a study of the effectiveness of paroxetine for post-traumatic stress disorder, the differences with placebo were less significant due to the high placebo effect. In the paroxetine group, 60% of patients were responders, in the placebo group - 49% [19].
Obsessive-compulsive disorder is the most resistant to treatment among anxiety disorders. However, the effectiveness of paroxetine has also been proven in this form of anxiety, although in higher doses (40–60 mg/day). The paroxetine group showed a significant improvement on the Y-BOCS scale compared to placebo. The relapse rate was also significantly lower in the paroxetine group (38%) compared with the placebo group (59%), p < 0.033 [13].
Paroxetine has a favorable safety profile. The main side effects when taking it are headache, nausea and other gastrointestinal disorders, sleep disorders and sexual dysfunction. Side effects are not pronounced and regress on their own during the first weeks of taking the drug. The cardiac safety of paroxetine appears to be proven [12].
There is extensive experience in the use of Rexetine (paroxetine), including in domestic clinical practice. The clinical effects of Rexetine have been most studied in the treatment of anxiety disorders encountered in the practice of a neurologist and internist, although it can also be used in psychiatric clinics. Thus, in a study of the effectiveness of Rexetine at a dose of 20–60 mg/day in the treatment of anxiety and depressive disorders in patients who consulted a psychiatrist, the proportion of responders was 50% [1]. When taking Rexetine in patients with anxiety and depressive disorders against the background of dyscirculatory encephalopathy, remission was observed in 91% of patients [8].
In a neurological hospital, Rexetine was effective not only for panic disorder, but also for other diseases accompanied by anxiety - somatized dysthymia, “masked” depression, migraine, tension headache, and other chronic pain syndromes [4].
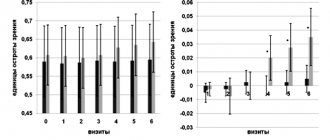
In the work of Less Yu. E. et al. [6] studied the effectiveness of Rexetine at a dose of 20 mg/day for GAD, taking into account comorbid anxiety and affective conditions (panic disorder, agoraphobia, obsessive-compulsive disorder, depression). The patients were divided into three groups. The first group consisted of patients with isolated GAD, the second group included patients with GAD accompanied by erased comorbid disorders at the subsyndromal level. The third research group included individuals with extensive, clinically significant comorbid disorders. The study confirmed the high effectiveness of Rexetine for GAD. In 35.9% of patients, a remission level was achieved by the end of the course of therapy, 17.9% were classified as responders, 28.3% as partial responders, and only 17.9% as non-responders. The dynamics of anxiety on the Hamilton scale, assessed in this study, are presented in
.
According to the dynamics of the total HAM-A score, a significant decrease in anxiety was noted at all time points (7, 14, 21, 28, 35 and 42 days from the start of taking Rexetine). The rate of reduction in symptoms, which was the same in all groups during the first two weeks of therapy, further slowed down in the group of patients with severe comorbid disorders, while in the groups of patients without comorbid disorders and with subclinical comorbid disorders, the therapeutic effect steadily increased, reaching a maximum level by the end of the study. By the time the course of therapy was completed, the regression of anxiety symptoms in the groups of patients without comorbid disorders and with subclinical comorbid disorders was significantly greater than in the group of patients with severe comorbid disorders [6]. Thus, this study confirms the information about the high effectiveness of Rexetine in the treatment of GAD. The anti-anxiety effect of the drug begins to manifest itself from the first days of therapy and gradually increases, reaching a maximum after a month of treatment. A dose of 20 mg appears to be adequate in most cases, but in cases of GAD complicated by comorbid emotional disorders, the dose of Rexetine should apparently be increased [6].
Rexetine has proven to be a highly effective drug for the treatment of specific phobias. With this form of anxiety disorder, a fairly rapid effect of Rexetine was noted. Already in the first week, there is a decrease in the feeling of internal tension, regression of vegetative symptoms (sweating, the intensity of the feeling of “incompleteness” of inspiration has decreased), and sleep improves. The most pronounced reduction in the intensity of anxious experiences and improvement in the well-being of patients was observed during the first 4 weeks of Rexetine therapy. Normalization of well-being to the initial, pre-painful state was observed starting from 3–4 weeks of treatment [9].
There is experience in using Rexetine in patients with somatic diseases and concomitant anxiety and depressive disorders. Thus, Rexetine can be used with antihypertensive, vascular, cardiological, antidiabetic and other drugs that are often necessary for patients for health reasons. It has been established that it does not cause addiction or dependence [5].
Our experience in using Rexetine in patients with anxiety and anxiety-depressive disorders showed that among 20 observed patients, 12 people (> 50%) noted complete remission after 6 months of therapy. In approximately 2/3 of cases (13 patients), comorbidity with depressive spectrum disorders was noted. The most common manifestations were: sad mood, depression, sleep disturbances, pain (in the neck and lower back), slowness of movements and speech. During therapy, a gradual reduction of these manifestations was observed. In the dynamics of anxiety symptoms, such manifestations as anxiety, fatigue, irritability, and muscle tension underwent the greatest regression. It should also be noted the effect of therapy on the presentation of autonomic manifestations of anxiety: tachycardia, hot and cold flashes, cold extremities. In general, according to patient reports, 14 of them (70%) rated the results of treatment as “good” or “excellent”. It should be noted that at the time of therapy, 4 patients were taking pharmacological agents prescribed by internists for concomitant diseases (beta-blockers, antihistamines, vasoactive drugs). In no case were there any signs of drug interactions. In addition, during therapy, one patient noted a decrease in episodes of existing tension-type headaches, in two cases a reduction in insomnia was observed, 4 patients noted a decrease in the intensity of accompanying pain manifestations (pain in the cervical region and lower back) and a decrease in the amount of analgesics consumed while taking Rexetine.
Thus, the proven effectiveness, high safety of Rexetine and extensive experience in its use in the treatment of anxiety disorders allow this drug to be actively used in everyday practice by doctors of various specialties.
Literature
- Bobrov AC, Petrunko OB, Kovaleva AB, Pavlova O. N. Rexetine in the treatment of depressive states // Journal of Neurology and Psychiatry named after. S. S. Korsakova. 2005. No. 11.
- Vein A. M., Dyukova G. M., Vorobyova O. V., Danilov A. B. Panic attacks. M.: Eidos Media. 2004. 408 p.
- Gaev G. Geniuses in private life. M.: Kron-press. 1999.
- Dmitriev O.V. Experience of using the drug Rexetine in a neurological hospital // Breast Cancer. 2005. T. 13. No. 22.
- Enikolopov S. Anxiety and hypertension. Vicious circle // Ukrainian Rheumatology Journal. 2008. No. 2 (32). pp. 27–28.
- Less Yu. E., Malygin Ya. V., Chakhava V. O. Efficacy of the drug Rexetine in patients with generalized anxiety disorder // Breast Cancer. 2005. T. 13. No. 22.
- Pietsukh V. A. Literary dreams of V. G. Belinsky. A comment. M.: Moscow worker. 1989.
- Retyunsky K. Yu., Khmelnova I. V., Malkova E. B. Therapeutic effectiveness of rexetine in vascular depression // Psychiatry and psychopharmacotherapy. 2005. T. 7. No. 6.
- Rumyantseva G.M., Stepanov A.L., Levina T.M. Clinical effectiveness of the drug “Rexetine” (paroxetine) for anxiety spectrum disorders // Psychiatry and psychopharmacotherapy. 2005. T. 7. No. 6.
- Smulevich A. B. Depression in general medical practice. M., 2000. 160 p.
- Shuvalov A.V. Psychiatry, narcology, sexopathology. New classification of ICD-10. M.: Soviet sport. 2001.
- DeVane CL Pharmacokinetics, drug interactions and tolerability of paroxetine and paroxetine CR // Psychopharmacology Bulletin. 2003. V. 37 (Suppl1). P. 29–41.
- Ninan TP Obsessive-compulsive disorder: implications of the efficacy of an SSRI, paroxetine // Psychopharmacology Bulletin. 2003. V. 37 (Suppl. 1). P. 89–96.
- Nutt D., Ballenger J. Anxiety disorders. Generalized anxiety disorder, obsessive-compulsive disorder and post-traumatic stress disorder // Blackwell Publishing. 2005. 242 p.
- Nutt D., Feeney A., Argyropolous S. Anxiety disorders comorbid with depression: panic disorder and agoraphobia // Martin Dunitz. 2002. 111 p.
- Pollack MH, Doyle AC Treatment of panic disorder: focus on paroxetine // Psychopharmacology Bulletin. 2003. V. 37 (Suppl. 1). P. 53–63.
- Sheehan DV, Mao CG Paroxetine treatment of generalized anxiety disorder // Psychopharmacology Bulletin. 2003. V. 37 (Suppl. 1). P. 64–75.
- Starcevic V., Bogojevic G. The concept of generalized anxiety: disorder between the too narrow and too wide diagnostic criteria // Psychopathology. 1999. V. 32. P. 5–11.
- Stein DJ, Hollander E. Anxiety disorders comorbid with depression: social anxiety disorder, post-traumatic stress disorder, generalized anxiety disorder, obsessive-compulsive disorder // Martin Dunitz. 2002. 72 p.
- Walley EJ, Beebe DK, Clark JL Management of common anxiety disorders // Am Fam Physician. 1994. V. 50. P. 1745–1753.
G. R. Tabeeva Yu. E. Azimova
MMA im. I. M. Sechenova, Moscow
Table.
Rice. 2.
PAROXETINE (tablets)
chii, but there is always the opportunity to purchase to order.
The cost is quite affordable - 370 rubles. I’ll tell you about the effect of the drug a little later, but now the appearance of the packaging: I bought paroxetine from the pharmaceutical company ReplekPharm, but there are other manufacturers.
The expiration date is stamped on the packaging.
The tablets themselves are small in size, film-coated, and easy to swallow with a small amount of liquid.
The instructions for the drug are frighteningly huge, the number of side effects is alarming, but I, deciding that things couldn’t get worse, dared to try this medicine.
And then the fun began. It’s good that the doctor warned that it is better to start taking pills on Friday evening, so that by the end of the new week you will become a little more human. The first day was just hell. All my worries and fears seemed to increase in volume several times. On Friday evening I just howled like a beluga. The family fled to different corners, realizing that it was better not to get caught by me. On the second day it got even worse, I was shaking like an alcoholic after a serious binge. I didn’t want to do anything, I didn’t want to eat, I didn’t want to drink, I didn’t want to do anything, I didn’t want to see anyone either. My husband rushed to call the doctor, but he reassured me that this was how it should be, you just had to be patient. But I absolutely didn’t want to endure it; it was unclear why such medications were needed if they made me feel so bad after them. Well, they persuaded me to wait another day, citing the fact that if it doesn’t go away on Sunday, then we’ll stop taking it on Monday. On Sunday it became easier, I no longer wanted to kill anyone, I just wanted to sleep. I fell asleep at lunchtime and slept without my hind legs almost until the evening. In the evening I took another pill, drank some water and continued to sleep, finally thinking that I wouldn’t get up for work tomorrow no matter what. Monday morning was the most ordinary, nothing special. Having slept well and taken another pill, I safely went to work. I was surprised that almost nothing pisses me off. Everything seems calm, and things that used to irritate me no longer bother me. I thought it was because I slept enough. I took the tablets on schedule three times a day. I was surprised to notice that practically nothing irritates me. This was the result after a week of taking the drug. I was calm as a boa constrictor after lunch. All emotional problems went away, I calmed down. I took paroxetine for two months. The doctor said that the minimum dose of the drug is one month to restore the functions of the nervous system. It is not recommended to take the medicine for less than a month, as there will be no therapeutic effect. The most important thing is that there is no “withdrawal effect”, i.e. a return to a depressive state; - a large number of side effects; - Sold only with a doctor's prescription; — the price, which is affordable at first glance, actually results in a decent amount for the entire course of treatment; — for a course of treatment you need to order at least four packages at once.
In conclusion of my review, I would like to note that our health is in our hands. Do not bring your emotional state to a critical point; it can be very difficult to recover. Take care of your nerves, no problems are worth killing yourself over. But if a problem arises and there is no way to cope on your own, there is nothing reprehensible in turning to specialists. And the most important thing is the support of loved ones. And the medicine, although scary, works. If such a drug is chosen by a doctor, then you need to take it. I give the drug four stars for the initial effect. Take care of yourself and your loved ones.