Pharmacological properties of the drug Gentos
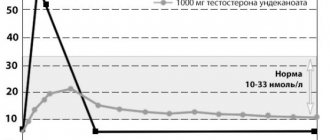
The drug Gentos has a complex therapeutic effect on the urogenital system. Restores neurohumoral regulation in the hypothalamus-pituitary-testicular system, helps normalize the levels of testosterone, 5-α-dihydrotestosterone and estradiol, eliminates age-related androgen deficiency. Has an antiproliferative effect on the prostate. It affects both the mechanical component (cessation of stroma proliferation) and the dynamic component (normalization of the tone of the smooth muscle of the detrusor and the bladder wall, which leads to the restoration of its reservoir and evacuation functions) of the formation of dysuria in benign prostatic hyperplasia. Improves microcirculation, venous outflow in the tissues of the urogenital zone and reduces congestion in the pelvic organs and the severity of intravesical obstruction caused by prostate edema. It has an anti-inflammatory, anti-exudative effect, reduces the intensity of pain in patients with acute prostatitis. Improves microcirculation and venous outflow in the tissues of the genitourinary system, moderately increases cavernous blood flow, improving erectile function in patients with chronic prostatitis. Having an antiproliferative effect on the prostate gland, it reduces benign prostatic hyperplasia.
Microflora of the urogenital tract in men examined for chronic prostatitis
Treatment of chronic inflammatory pathology of the urogenital tract in men has always been a difficult task in urology. Treatment for these diseases, especially those complicated by impaired fertility, sexual dysfunction, pelvic pain syndrome, can be successful if done individually and based on knowledge of the etiology of the inflammatory process, immunoreactivity to this inflammatory process and morpho-functional changes in the pelvic organs.
In widespread medical practice, at present, when diagnosing the etiological factor of inflammatory pathology of the urogenital tract, the emphasis is on identifying sexually transmitted infections. The purpose of this study is to demonstrate the significance of other, no less important, etiological factors, as well as the place of STIs in the pathogenesis of this group of inflammatory diseases. An infectious inflammatory process in the urogenital tract occurs by two mechanisms.
In the first case, a virulent STI causes clinically and laboratory identifiable urethritis, which subsequently leads to the occurrence of an ascending inflammatory process. The pathogenetic role of sexually transmitted infection in this case is obvious: when examining discharge from the urethra, prostate secretion, seminal fluid, a significant increase in the number of leukocytes and STIs is revealed; The primary inflammatory process begins with the clinical picture of urethritis. Patients with an inflammatory process of this nature are most often treated in dermatovenerological dispensaries, when in addition to acute venereal disease there is a prostatitis clinic.
The second mechanism is more complex. The occurrence of an infectious inflammatory process in the urogenital tract in this case is preceded by certain predisposing factors.
Let's highlight several main groups:
- The first group of factors includes vascular, trophic and morpho-functional changes in the pelvic organs, which arise as a result of congestion in the pelvic organs, habitual intoxication and other reasons. These changes are well known and widely discussed in the specialized domestic literature.
- Infravesical obstruction is also a predisposing cause of infectious inflammation. In this case, a retrograde flow of urine occurs into the acini of the prostate gland at the time of urination due to an increase in intraurethral pressure. This can lead to infection of the prostate gland by microflora from the overlying urinary tract.
- The most important predisposing cause of the inflammatory process of the urogenital tract is secondary immunodeficiency, which develops against the background of a sluggish bacterial intracellular infection (chlamydia, mycoplasma) and persistent viral infection (urogenital herpes, cytomegalovirus). Infection of the urogenital tract with this microflora leads to a characteristic disturbance of phagocytic activity (HCT test), a decrease in class A immunoglobulins with an increase in class G immunoglobulins; disruption of T helper and T suppressor interaction. Secondary immunodeficiency, as well as certain morpho-functional changes in the pelvic organs open the way to infection of the urogenital tract with banal pathogenic and conditionally pathogenic bacterial microflora.
With the development of an infectious process in the urogenital tract according to this mechanism, there is no clinical manifestation of urethritis, in studies of discharge from the urethra there will be no significant increase in the number of leukocytes, in scrapings from the urethra STIs will be detected much less frequently, however, patients will have a clinically and laboratory identifiable inflammatory process in the prostate-vesicular complex or in the scrotal organs.
In the presence of the above predisposing factors, infection of the urogenital tract with banal bacterial microflora is fundamentally possible in two ways: transurethral and hematogenous.
Hematogenous infection most often occurs from foci of chronic infection with concomitant ENT pathology, diseases that are widespread among the population; for diseases of the rectum with chronic constipation, hemorrhoids (especially with frequent exacerbations). Infection through this route most often occurs when there are already pronounced structural changes in the prostate gland (congestion, calcifications, BPH).
The transurethral route of infection with secondary bacterial microflora is more significant. Four main sources of bacterial infection should be identified.
- Widespread bacterial vaginosis in women. According to the Preobrazhenskaya Clinic, women examined for inflammatory diseases of the genital organs were diagnosed with bacterial vaginosis in 20% of cases. The cause of bacterial vaginosis is small opportunistic rod flora, which often leads to infection of the urogenital tract of men. The cause of bacterial vaginosis is sluggish bacterial and persistent viral infections, hormonal disorders and other causes that cause secondary immunodeficiency. In married couples, women suffering from bacterial vaginosis and husbands are much more likely to have chronic prostatitis than women with inflammatory gynecological diseases, but not having bacterial vaginosis.
Table of microorganisms most often found in the genital organs of women with inflammatory diseases caused by gardnarella vaginalis and non-spore-forming bacteria. (collection of works of UrNIIDVII, 1985)
| Types of microorganisms. | Morphological features. |
| Garnarella vaginalis | Coccobacilli single, paired, polymorphic |
| Undifferentiated species | Coccobacilli polymorphic |
| Coryneforms | Club-shaped sticks |
| Bifidobacteria | The rods are variable, often with forked ends. |
| Bacterioids | Rods, coccobacilli, often bipolarly colored |
| Lactobacilli | Polymorphic shelves, often arranged in long filaments. |
| Anaerobic cocci | Cocci, solitary, in groups or in chains. |
| Aerobic cocci | Cocci, chains, tetrads, clusters. |
| Propionibacteria | Polymorphic rods, club-shaped, coccoid. |
| Cellos | Cocci, diplococci, clusters or chains. |
| Fusobacteria | The rods are large, polymorphic, often long with pointed ends, and may have thickenings in the center. |
- The prevalence of oral-genital and anal sexual intercourse is also a source of infection of the urogenital tract of men. In the first case, infection occurs predominantly with streptococcal or staphylococcal microflora, in the second case - with Gr-bacillus flora (Proteus, Klebsiella, Escherichia coli, etc.).
Clinical case.
Patient N13603 Igor Nikolaevich, 30 years old, applied on May 16. 98 years old with complaints of pelvic pain. Examined at UrNIIDVII for the presence of STIs - gonorrhea, trichomoniasis, candidiasis, gardnarellosis, chlamydia, ureaplasmosis, mycoplasmosis, HSV were not found, in the secretion of the prostate gland there were 20-40-80 leukocytes per p/z, there was no evidence of extragenital inflammatory pathology. A bacteriological study of prostate secretions was performed. Staphylococcus with hemolysis and Gr+ bacillus with hemolysis were detected, TMC 10x9 in 1 ml of discharge. Upon further questioning, it was found that the family regularly practices oral-genital sex, and the wife suffers from chronic tonsillitis and sinusitis with frequent exacerbations. The wife (N13784 Anna Sergeevna, 29 years old) was referred to an otolaryngologist. A bacteriological study of tonsil washings revealed staphylococcus with hemolysis, Gr+ rod with hemolysis, TMC 10x6 in 1 ml of discharge, the presence of chronic tonsillitis and sinusitis in the subacute phase was confirmed.
- Iatrogenic infection by hospital microflora during urethral therapeutic or diagnostic procedures, which are widespread at present.
- Infection from the upper urinary tract and bladder, especially in the presence of bladder outlet obstruction.
The mechanism for the development of bacterial inflammation in the urogenital tract, when its cause is not sexually transmitted infections, is clearly presented below.
The purpose of this work was to analyze the microflora in patients examined for chronic prostatitis. In addition to examinations for STIs, over 1996-98, the Preobrazhenskaya Clinic performed more than 200 bacteriological cultures on men for various indications.
Bacteriological research of prostate secretions is carried out on the basis of the bacteriological laboratory of the UrNIIDVII. Before collecting the material, the patient is asked to empty the bladder and toilet the glans penis and preputial sac. Next, a massage of the prostate gland is performed, its secretion is placed in a test tube with a storage medium - sugar broth. Test tubes in a thermostat are delivered to the bacteriological laboratory within 40-60 minutes, where the material is immediately dispersed into 4 nutrient media: meat peptone agar, blood agar, Endo medium and Sabour medium. After 24 hours, for further identification of the pathogen, subculture is carried out on appropriate nutrient media (for example, to identify staphylococcus in yolk-salt agar to assess lyceto-vitellase activity, in blood plasma to assess plasma-coagulating activity). After 5 days, the results are “read”, pure cultures are transferred to media with disks soaked in antibacterial drugs, and after 24 hours the antibiogram is “read”.
The study group included only those patients who, despite the presence of clinical and laboratory data for the inflammatory process in the prostate-vesicular complex, did not have any data for inflammation in the urethra, those who met the following conditions below.
- Minimum scope of examination: smear analysis, examination of prostate secretions, examination for chlamydia, ureaplasmosis, mycoplasmosis, chronic gonorrhea, blood for HIV, RW, bacteriological examination of prostate secretions, ultrasound of the prostate gland with a transrectal sensor.
- The entire examination complex was completed within no more than 14 days.
- There is no clinical evidence of urethritis, and in the study of leukocytes discharged from the urethra there are less than 10 leukocytes in the field of view.
- Negative Wesserman reaction and absence of HIV.
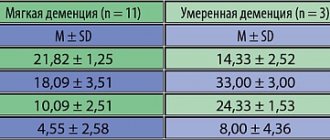
Thus, in the study group there were 63 patients in whom 113 microorganisms were isolated in a bacteriological study of prostate secretions. The age of the patients ranged from 20 to 65 years. Let us note a certain pattern in the total degree of leukocytosis in prostate secretions in patients of different age groups.
| Age | Number of persons | % | Leukocyte count min | White blood cell count average | White blood cell count max |
| 20-29 years old | 18 | 28 | 21 | 35 | 65 |
| 30-39 years old | 25 | 40 | 34 | 58 | 101 |
| 40-49 years old | 13 | 21 | 27 | 44 | 93 |
| 50-65 years | 7 | 11 | 24 | 44 | 83 |
In the first age group, due to the fact that the inflammatory process began relatively recently, leukocytosis is still quite moderate. In the second group, where the history of the inflammatory process is already long, and the immune response to the inflammatory process is quite active, leukocytosis is the highest of the groups presented. In the third and fourth groups, despite pronounced structural changes in the prostate gland, leukocytosis decreased again. This may be due to a significant decrease in the immune response during a long-term chronic inflammatory process.
The structure of the identified microflora in the bacteriological study of prostate secretion is presented in Table N1.
The data from the research performed must be assessed with a high degree of criticality for the following reasons:
- This laboratory does not have an anaerostat to perform inoculation under anaerobic conditions, therefore the number of anaerobic microorganisms should be significantly greater.
- A significant increase in opportunistic microflora sometimes obscures the true causative agent of inflammation. During repeated bacteriological examination after treatment, pathogenic microflora are sown much more often. However, this topic is beyond the scope of this work.
Both pathogenic and opportunistic microorganisms were identified. The ratio of pathogenic and opportunistic microorganisms is presented in the diagram.
Microorganisms were sown both as a monoinfection and in associations, which is presented in Table N2.
Thus, it is clear that in 68.2% of cases, in a bacteriological study of prostate secretions, associations of microorganisms are sown. Note that in 46% of those examined (those 29 patients out of 63), microorganisms causing hemolysis of blood agar were identified in the secretion of the prostate gland, and the higher the degree of association, the more often a hemolytic microorganism is detected in its structure. More than half of the patients are diagnosed with STIs, and their detection rate remains almost the same regardless of the degree of association.
These data are presented in table N2.
Table N3 shows the identified hemolytic microflora:
The presented diagram shows that the detection of staphylococcal microflora predominates, which corresponds to the general layout of the detected microflora. Second place is occupied by Gram+ rod flora (unidentified Gr+ rod flora and corynobacteria), and streptococcus is in third place. Separately, we note that a certain part of the Gram-rod flora also exhibits hemolytic activity (12.5% of the total number of identified Gram-bacteria).
We classified all other microorganisms as opportunistic microflora. We decided not to isolate microorganisms from this group, which can be considered more likely to be saprophytes. In our opinion, it is necessary to classify a particular microorganism as a saprophytic microflora individually, taking into account all clinical and laboratory diagnostic data.
Opportunistic microflora is presented in Table N4.
Based on the structure of pathogenic and conditionally pathogenic microflora, it is easy to notice that the detected coccal microflora, especially streptococcal microflora, is also characteristic of chronic diseases of the oral cavity. Gr+ and Gr- rod microflora are a common causative agent of bacterial vaginosis in women; in addition, Gr- rod microflora is often a hospital microflora and an infection detected in chronic inflammatory diseases of the urinary system.
In 33 patients i.e. In 52.4% of those examined, in the absence of clinical and laboratory signs of an inflammatory process in the urethra, STIs were detected.
The identified STIs are presented in Table N5.
Gonorrhea was identified by examining scrapings from the urethra using the PCR method.
Yeast cells were detected during bacterioscopic examination of urethral discharge or in bacteriological examination of prostate secretions with identification to species. Chlamydia was identified by examining scrapings from the urethra using PCR or PIF or by the presence of class M immunoglobulins for infection. Ureaplasmosis and mycoplasmosis were identified by examining scrapings from the urethra using the PCR method. HSV and CMV were identified by examining scrapings from the urethra using PCR or by the presence of class M immunogobulins for infection.
A comparative analysis of the detection rate of STIs in patients in two groups was carried out:
Group 1 - bacteriological culture of prostate secretion contains a pathogen, Group 2 - bacteriological culture reveals only opportunistic microflora.
The obtained data are presented in table N6.
Thus, it is clear that candidiasis, ureaplasmosis, mycoplasmosis, and viruses are detected equally in both groups. But in the group with pathogenic microflora, gonorrhea and chlamydia are detected much more often. In practice, in patients with clinical and laboratory data of an inflammatory process in the prostate-vesicular complex and in the presence of chlamydia, hemolytic bacterial microflora is always cultured!!!
Another reason why this work was done is demonstrated by the following diagram.
Conclusions:
- In all patients examined for chronic prostatitis in the absence of clinical and laboratory data of acute or chronic urethritis, bacteriological examination of prostate secretions revealed nonspecific bacterial microflora. In 46% of patients (29 out of 63 people), pathogenic (hemolytic) microflora was detected.
- In 54% of patients, opportunistic microflora was identified; the pathogenicity of this microflora is assessed based on the specific clinical situation, taking into account all examination data.
- In 68% of cases, microorganisms were sown by associations. Moreover, the higher the degree of association, the more often a microorganism with hemolytic activity was identified in it.
- The structure of the bacterial microflora of the urogenital tract in men (both with and without hemolytic activity) suggests its possible source is bacterial vaginosis and diseases of the oral cavity in sexual partners, as well as, possibly, a hematogenous route of infection.
- In 52.4% of patients, in the absence of clinical and laboratory data of acute or chronic urethritis, sexually transmitted infections were detected. Moreover, in cases where gonococci or chlamydia were determined in scrapings from the urethral mucosa by the PCR method, hemolytic microflora was determined during bacteriological examination of prostate secretions.
- Considering the fairly pronounced resistance of the identified microflora to antibacterial drugs, it is recommended to include bacteriological culture of prostate secretions in the examination program for patients with inflammatory diseases of the urogenital tract.
Zhuravlev V.N., Vlasenko L.Yu., Pankov V.I.
Use of the drug Gentos
Gentos in the form of drops for oral use: orally, adults and adolescents - 10 drops of the drug in pure form or diluted in 1 tablespoon of water 3 times a day 30 minutes before or 1 hour after meals. At the beginning of treatment, as well as in cases requiring rapid reduction of symptoms of the disease, it is possible to take the drug every 30 minutes until the condition improves, but no more than 8 times a day, after which it can be taken 3 times a day. To achieve maximum effect, it is recommended to take Gentos between meals (30 minutes before or 1 hour after meals), and keep the drug in your mouth for some time before swallowing. For acute prostatitis and acute cystitis, the course of treatment is 2 weeks. For benign prostatic hyperplasia, chronic prostatitis, chronic cystitis, bladder atony, chronic urination disorders of various origins, the course of treatment is 3 months. When the condition stabilizes, it is possible to switch to a 1-2 dose dose. Gentos in tablet form.
Dosing | A course of treatment | |
| Benign prostatic hyperplasia: | ||
| Adults | 1 tablet | 2 times a day for 3 months |
| Prostatitis: | ||
| Teens and adults | 1 tablet | 2 times a day for 1–3 months |
| Cystitis, bladder atony : | ||
| Teens and adults | 1 tablet | Cystitis: 1st–2nd day of treatment - 4 times a day, then 2 times a day for 2 weeks. Bladder atony: 2 times a day for 3 months |
| Children 5–12 years old | 1/2 tablet | |
| Disorders of urination, including in the postoperative period: | ||
| Teens and adults | 1 tablet | 2 times a day for 3 months |
| Children 5–12 years old | 1/4 tablet | |
At the beginning of treatment, as well as in cases requiring rapid reduction of symptoms of the disease, the drug can be taken by adults and adolescents, 1 tablet; children aged 5–12 years, 1/2 tablet 4 times a day until the condition improves, but no more than 8 times, after which take 2 times a day. To achieve the maximum effect, Gentos should be taken 30 minutes before or 1 hour after a meal; it is recommended to keep the tablet in the mouth until dissolved.
Composition and release form:
- Gentos drops in dark glass bottles with a drop dispenser of 20 drops; 50 and 100 ml. The bottle contains a transparent liquid of yellow or orange-brownish color, with a sweet aspen taste and a specific odor. Bottle in a cardboard box.
- Gentos sublingual tablets. Flat-cylindrical in shape, with a chamfer and a notch, white in color (possibly a yellowish tint, small inclusions and marbling). Without smell. There are 20 pieces in a blister. In a cardboard box 1; 2 or 3 blisters.
Gentos-drops
- Active ingredients (per 100 ml): Populus in dilution D1 - 7 ml, Sabal in dilution D6 - 10 ml, Conium in dilution D6 - 10 ml, Kalium iodatum in dilution D12 - 10 ml, Ferrum picrinicum in dilution D12 - 10 ml.
- Auxiliary component: ethanol up to weight (43%).
Gentos tablets
- Active ingredients (per 1 tablet): Populus in dilution D1 - 25 mg, Sabal in dilution D6 - 37.2 mg, Conium in dilution D6 -37.2 mg, Kalium iodatum in dilution D12 -37.2 mg, Ferrum picrinicum in dilution D12 – 37.2 mg.
- Auxiliary ingredients: potato starch, lactose monohydrate, magnesium stearate.
Note!
The description of the drug Gentos on this page is a simplified author’s version of the apteka911 website, created on the basis of the instructions for use. Before purchasing or using the drug, you should consult your doctor and read the manufacturer's original instructions (attached to each package of the drug).
Information about the drug is provided for informational purposes only and should not be used as a guide to self-medication. Only a doctor can decide to prescribe the drug, as well as determine the dose and methods of its use.
Gentos Forte price, where to buy
Gentos Forte is quite rare in Russian pharmacies. The lowest price indicated in Russian online stores is 205 rubles.
The price of Gentos Forte in Ukraine is usually about 250 hryvnia. Gentos, similar in action, in drops and tablets may be higher. The price of tablets is about 300 rubles, and capsules – 350 rubles.
- Online pharmacies in RussiaRussia
- Online pharmacies in UkraineUkraine
LuxPharma* special offer
- Gentos Forte capsules No. 40
RUR 3,450 order
show more
Pharmacy24
- Gentos forte No. 40 capsules A.R.K.O.-Kemie GmbH, Nimechchina
374 UAH.order