Lymphoma
- a form of cancer that affects lymphatic tissue. This disease is characterized by enlarged lymph nodes; in some cases, the progressive disease affects internal organs, where tumor lymphocytes begin to accumulate. They begin to multiply rapidly, and in the future they cannot perform their main duties. It is important to note that doctors find it difficult to name the exact cause of the development of this disease. However, there are suggestions that weakened immunity, age and infectious diseases may increase the risk of lymphoma.
If we consider the features of the course of this disease, then there are 2 forms of this disease:
• Hodgkin's lymphoma;
• non-Hodgkin's lymphoma.
So, what is this disease and what types it is divided into.
Lymphoma is a malignant tumor that consists of lymphocytes. Lymphocytes, in turn, are cells of the immune system and are found in the blood or lymph. Depending on which lymphocytes the tumor is formed from, several main types of lymph are distinguished.
Today in medicine there are 2 types of lymphocytes:
• T-lymphocytes – take an active part in the fight against infections and are able to act directly on harmful carriers, without resorting to the help of antibodies.
• B-lymphocytes - are responsible for the production of immunoglobulins, that is, antibodies that subsequently fight infections, fungi and viruses.
What is lymphoma?
Lymphoma is a lesion of the immune system and internal organs, in which altered cells accumulate, disrupting tissue function.
The tumor develops in the lymphatic system, which helps us fight infections and other diseases.
The lymph circulating in it washes all the cells of the body and delivers the necessary substances to them, taking away waste. In the lymph nodes located throughout its network, dangerous substances are neutralized and removed from the body. The lymphatic system complements the circulatory system and helps fluids move throughout the body. Unlike blood, the speed of which is set by the “pump” - the heart, lymph slowly circulates on its own.
Complications
Any tumor in the stomach is characterized by complications:
- pain syndrome,
- ulceration with acute or chronic bleeding,
- perforation of the organ wall with the development of peritonitis.
In addition, with lymphoma, there may be a decrease in the specific gamma globulin IgG produced by normal immune cells, which contributes to frequent infections and inflammatory processes. The deficiency is compensated by intravenous administration of immunoglobulin.
In all cases, before starting chemotherapy, prevention of tumor lysis syndrome, which occurs when malignant cells are highly sensitive to drugs, is carried out.
How does lymphoma develop?
Oncology begins with the appearance in the body of just one altered cell of the immune system. In total, there are 2 main types:
- B lymphocytes
: produce antibodies - proteins that protect the body from bacteria and viruses. This is where most lymphomas form. - T lymphocytes
, one part of which destroys germs and abnormal cells, and the second helps to increase or slow down the activity of the immune system.
Almost all abnormal cells are identified and destroyed by our immune system, but some of them manage to survive. They gradually multiply, spread throughout the body, create tumors, accumulate in internal organs and disrupt their functioning.
The disease can occur in any area where lymphatic tissue is located, the main areas of which are:
- Lymph nodes
are small, pea-sized organs that are collections of cells of the immune system, including lymphocytes. There are more than 500 of them in the human body. - The spleen
, located under the lower ribs on the left side of the body. It produces lymphocytes, stores healthy blood cells and filters out damaged ones, and destroys microbes and foreign substances. - Bone marrow is
the spongy tissue inside certain bones. Here new blood cells are formed, including some lymphocytes. - The thymus, or thymus gland, is
a small organ located behind the upper part of the sternum in front of the heart. It is where some lymphocytes mature and develop. - Tonsils, or tonsils, are
collections of lymphatic tissue in the back of the throat. These organs help produce antibodies, proteins that prevent inhaled or ingested microorganisms from multiplying. - Digestive Tract:
The stomach, intestines and many other organs also contain lymphatic tissue.
Is lymphoma cancer?
Official medicine in Russia and some other countries refers to cancer as malignant tumors - life-threatening neoplasms that develop in epithelial cells contained in the skin or mucous membranes and lining the internal surface of organs.
Lymphoma is not a cancer, but an oncological disease. It is formed from lymphocytes, and its cells are also able to divide uncontrollably, accumulate in tissues, disrupting their work, and create additional foci of disease in various parts of the body.
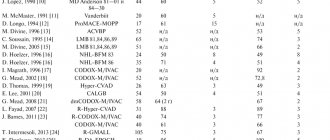
Clinical observation for NHL
Dynamic observation of children and adolescents is carried out for at least 3 years after completion of the treatment program.
In the first 3 months, the patient is examined every month, in the next 9 months - every quarter, then every six months.
The examination includes an examination of the patient with an assessment of complaints, clinical and biochemical blood tests with determination of LDH, ultrasound of the primary lesion, chest X-ray, and CT/MRI is used if indicated.
In recent years, whole body PET/CT with glucose has become widespread for dynamic monitoring of cured patients for the purpose of early diagnosis of relapse.
Types of lymphomas
Doctors distinguish 2 main classes of them:
- Hodgkin's lymphoma, or lymphogranulomatosis
: Most often starts in the lymph nodes of the upper body - in the chest, neck or armpits. It usually spreads to various lymph nodes through the lymphatic vessels, but in rare cases, in later stages it enters the bloodstream and spreads to other parts of the body, such as the liver, lungs or bone marrow. This diagnosis is made when special cells are identified in the body - Berezovsky-Reed-Sternberg, which are modified B-lymphocytes.
- TO non-Hodgkin's lymphomas
include all other types of the disease - there are about 30 of them. Each of them has its own special characteristics: the location of the primary tumor, the structure and speed of development.
Prevention
Lymphoma, which can cause symptoms in adults for a variety of reasons, can be prevented by following certain guidelines. Prevention will help reduce the risk of damage to the body to zero.
For this purpose it is necessary:
- less contact with toxic substances;
- do not neglect contraceptives during sexual intercourse with a casual partner;
- undergoes a course of vitamin therapy at least 2 times a year;
- maintain hygiene (do not use other people’s toothbrushes or towels);
- exercise regularly (moderately, at least 10-15 minutes will be enough).
Causes of lymphoma development
Doctors and scientists do not know exactly why the disease begins to develop in the human body. They only know about the factors that increase the likelihood of developing each type of cancer.
For Hodgkin's lymphomas
they look like this:
- Epstein-Barr virus
, which causes infectious mononucleosis - damage to lymphoid tissue, including adenoids, liver, spleen and lymph nodes. In some patients, parts of the virus are found in Berezovsky-Reed-Sternberg cells, but in most patients there are no signs of it. - Age
: Diagnosis can be made at any age, but it is most common in 20-year-olds and people over 55. - Gender
: The disease is more common among men than among women. - Heredity and family history
: The risk is increased for siblings and for identical twins. Identical twins develop from a single egg fertilized by a single sperm. They come in only one gender, have the same genes and are extremely similar in appearance. owners of Hodgkin's lymphoma. The reason for this is not exactly known - perhaps the whole point is that members of the same family suffer the same infections in childhood, or have common inherited gene changes that increase the likelihood of developing this type of oncology. - Weakened immune system
. The chances of receiving this diagnosis increase in people with HIV infection and disorders of the immune system, which develop, among other things, due to the use of drugs that suppress it, which is often required after an organ transplant.
List of such factors for non-Hodgkin's lymphomas
looks different:
- These include exposure to radiation
, including doses received during radiation therapy used to treat other types of cancer. - Various substances
, including herbicides and insecticides that kill weeds and insects, as well as chemotherapy drugs. - Age
: as a rule, the older the person, the higher his risks - in most cases the disease occurs at the age of 60+, but some types also occur in younger people. - Malfunctions of the immune system
affect the chances of developing all types of lymphomas. - Some viruses
can influence the DNA of lymphocytes, which encrypts all the information about our body, and convert them into cancer cells. - Infections that constantly stimulate the immune system and force our natural defenses to work harder also increase the risk of receiving a serious diagnosis.
- Having close blood relatives - parents, children, brothers or sisters - with this diagnosis also increases the likelihood of developing the disease.
- Some studies have shown that breast implants, especially those with a rough surface, may cause anaplastic large cell lymphoma. It develops on the skin, lymph nodes, or scar tissue formed at the site of the incision.
Symptoms and signs of lymphoma
As a rule, in the early stages this type of oncology does not manifest itself in any way, and its owner feels well and is not aware of the disease - almost all of its symptoms appear later, in advanced stages.
One of the most common signs is the appearance of swelling in the neck, armpits, groin, or above the collarbone.
, which is an enlarged lymph node. Typically, such a tumor does not hurt, but over time it often increases, and new lumps appear next to it or in other areas of the body.
Lymphomas that begin to develop or grow in the abdominal cavity can cause swelling
or
abdominal pain, nausea,
and
vomiting
. Such sensations occur due to enlargement of the lymph nodes or internal organs, such as the spleen or liver, or the accumulation of large amounts of fluid.
An enlarged spleen can put pressure on the stomach, causing loss of appetite.
and
a feeling of fullness after a small amount of food
.
Enlarged thymus Thymus, or thymus gland -
a small organ located behind the upper part of the sternum in front of the heart.
It is where some lymphocytes mature and develop. or lymph nodes in the chest may put pressure on the trachea, which carries air to the lungs. This leads to coughing
,
difficulty breathing, pain
or
heaviness in the chest
.
Brain lesions can cause headaches, weakness, personality changes, and problems with thinking
and
seizures
.
Other types of the disease can spread to the tissues surrounding the brain and spinal cord, causing the patient to see double and have a numb face
and
speech deteriorates
.
Lymphomas of the skin often appear as itchy red bumps
or
cones
.
In addition, symptoms may include:
- weight loss;
- chills;
- night sweats;
- elevated temperature;
- severe fatigue;
- bloating;
- frequent or severe infections;
- Easy bruising or bleeding.
Relapses
MALT lymphoma of the stomach has a slow course, however, as the stage increases, the likelihood of relapse increases. Starting from stage IIE, tumor recurrence is possible in every second patient, but the average period of relapse has not been determined due to the rare occurrence of the disease. The ability of some recurrent nodes to shrink without treatment—self-limitation—has been noted.
With aggressive lymphoma, relapses occur more often and remissions are shorter. In all situations, in case of relapse, chemotherapy is resorted to.
Diagnosis of lymphoma
Most patients see a doctor because they have certain signs of illness or feel unwell. Specialists begin the examination with an examination and questioning about family diagnoses, possible risk factors and other health problems. Then the lymph nodes and other parts of the body that contain lymphatic tissue are examined, including the spleen and liver. After which a number of studies are prescribed:
- Blood tests
: measure the levels of various cells in the blood, detect bone marrow damage, evaluate kidney and liver function, and detect infections and other problems. - Biopsy
is the removal of a piece of suspicious tissue and its transfer to a laboratory for examination. Depending on the course of the disease, doctors may need to biopsy lymph nodes, bone marrow, cerebrospinal fluid, pleural fluid, which is found in the chest, or peritoneal fluid, which is found in the abdomen. - Computed tomography
- allows you to identify foci of the disease in the abdominal cavity, pelvis, chest, head and neck. - Magnetic
resonance
imaging, MRI
, creates a detailed image of soft tissue. The method is usually used to study the spinal cord or brain. - X-ray
– helps detect enlarged lymph nodes in the chest or bones. - Ultrasound, ultrasound
- used to study enlarged lymph nodes or various organs, such as the liver, spleen or kidneys. - Positron
emission
tomography, PET
, can detect lymphomas in enlarged lymph nodes, even those that appear normal on CT. In addition, it can be used to determine whether the disease is treatable.
In the oncology department, a complete diagnosis of lymphoma is carried out - quickly, without queues and loss of precious time, using the most modern equipment. Our specialists guide the patient “from” to “to” – from examination to any treatment.
Criteria for assessing the completeness of remission
Criteria for assessing remission are needed by the doctor to determine the need to continue treatment or intensify therapy programs, or transfer the patient under dynamic observation.
- Complete remission - complete regression of all signs of the disease (clinical, hematological and other manifestations of the disease) according to imaging tests, determined twice with an interval of at least 4 weeks.
- Partial remission is a reduction in the size of tumor formations by at least 50% for a period of 4 weeks in the absence of new lesions.
- Stabilization of the disease is a reduction in the size of tumor formations by less than 50% or an increase in them by no more than 25% of the original volume in the absence of new lesions.
- Progression is the appearance of new lesions during treatment or an increase in previously existing ones by more than 25%, as well as the appearance of symptoms of intoxication.
- Relapse is the appearance of new lesions after achieving complete remission.
Lymphoma stages
Immediately after detecting the disease, doctors determine its stage - find out how far it has spread and what tissues it has damaged. This information is extremely important for specialists, since it allows not only to understand the patient’s prognosis, but also to select the most appropriate treatment for him.
Stages of Hodgkin lymphoma:
I
: Changed cells are found in only one group of lymph nodes or one lymphoid organ, such as the tonsils.
II
: they are present in 2 or more groups of lymph nodes located on one side of the diaphragm, or have spread from one damaged lymph node to an adjacent organ.
III
: lymphoma cells are present in the lymph nodes on both sides of the diaphragm;
or not only in the lymph nodes above the diaphragm, but also in the spleen. IV
: The disease has spread to at least one organ outside the lymphatic system, such as the liver, bone marrow, or lungs.
Stages of non-Hodgkin's lymphomas:
I
: altered cells are found only in 1 group of lymph nodes or one lymphoid organ, for example, tonsils;
or in 1 area of one organ outside the lymphatic system. II
: they are present in 2 or more groups of lymph nodes on 1 side of the diaphragm;
either in the lymph nodes and 1 area of an adjacent organ, or in another group of lymph nodes on the same side of the diaphragm. III
: lymphoma cells are present in the lymph nodes on both sides of the diaphragm;
or they are present in both the lymph nodes above the diaphragm and the spleen. IV
: The disease has spread to at least one organ outside the lymphatic system, such as the liver, bone marrow, or lungs.
Radiation therapy
The final stage of treatment for Hodgkin lymphoma is irradiation of all affected areas of the lymph nodes. As a rule, radiation therapy begins 2 weeks after the end of drug therapy when blood counts are normalized.
The radiation dose depends on the completeness of remission after drug therapy: upon achieving complete remission (disappearance of all clinical and radiological signs of the disease) in the lymphatic zone, according to PET-CT data, the radiation dose is 20 Gy. If the size of the tumor after polychemotherapy has decreased by 75% or more from the original tumor and/or there is a decrease in radiopharmaceutical hyperfixation according to PET-CT to 2-3 according to Deauville, then the radiation dose is 25 Gy. If tumor formations are reduced by less than 75% and/or radiopharmaceutical hyperfixation persists according to PET-CT 4-5 according to Deauville, the radiation dose is increased to 30 Gy.
Fig. 5 Radiation treatment plan. Patient I., 4 years 6 months. Hodgkin's lymphoma stage II. with damage to the cervical, supraclavicular, subclavian lymph nodes on the left, the thymus gland, and the nasopharynx. Condition after 4 courses of PCT, remission. Irradiation of the cervical-supraclavicular lymph nodes on the left with a consolidating purpose, SOD 20 Gy.
Fig.6 Patient M., 11 years old. Hodgkin's lymphoma stage II. with damage to the soft tissues of the neck, lymph nodes of the neck. Condition after 2 courses of chemotherapy. According to the control PET/CT data, no metabolically significant lesions were identified, remission. Conducting radiation therapy of the primary involved areas with a total focal dose of 20.0 Gy for the purpose of consolidation.
Lymphoma treatment
Treating lymphoma is not an easy task.
To solve it, you need not just one doctor, but a whole team of professionals - a chemotherapist, radiologist, surgeon, oncologist, hematologist and others. The oncology department has all the necessary specialists - world-class doctors who conduct a full diagnosis of the disease and any necessary therapy. With us, you don’t have to retake tests, redo studies and ask the question “what to do next?”
We fully guide the patient and give him a clear action plan, following which he gets the best possible result. Several methods are used to combat this type of cancer:
The main one is chemotherapy
– drugs that destroy altered cells. They are taken in pill form or injected into a vein, enter the bloodstream and spread throughout the body. Treatment is carried out in cycles, each lasting several weeks, followed by a period of rest during which the body recovers.
Bone marrow transplantation
or stem cells from which blood cells are formed. The procedure allows higher doses of chemotherapy, sometimes along with radiation, to be given, which helps kill the lymphoma more effectively. Transplantation is possible not only with donor material, but also with your own material, collected several weeks before the intervention.
Radiation therapy
– destruction of altered cells using radiation. This method is suitable for most patients, and works especially well if the disease has affected a small amount of tissue. It is used both independently and in combination with chemotherapy.
Immunotherapy
– drugs that help a person’s own immune system better recognize and destroy abnormal cells. There are several types used for lymphomas. These include:
- monoclonal antibodies are proteins designed to attack a specific substance on the surface of lymphocytes;
- Immune checkpoint inhibitors - drugs that prevent altered cells from masquerading as healthy ones;
- T-cell therapy: removal of immune cells from the patient’s blood and modification in the laboratory, their reproduction and return to the body, where they find and destroy foci of the disease.
Surgery
: Often used to obtain samples of suspicious tissue and determine its type, but rarely for therapy itself. In rare cases, operations are prescribed for lesions of the spleen or other organs that are not part of the lymphatic system - for example, the thyroid gland or stomach.
When to see a doctor
Of course, if fatigue and some other symptoms occur separately, you should not immediately attribute this to the onset of oncology. It is necessary to undergo tests in order to understand the cause of the malaise.
Before taking the tests, you need to prepare. A day before all procedures, a person eliminates alcohol and tobacco. The stomach should be empty. The time of the last meal is at least 12 hours. It is forbidden to drink tea, juices (natural and purchased), and chew chewing gum. Only drinking water is allowed.
Another important condition is that you should not worry before the procedures. Sometimes it is difficult to prevent absolutely all factors that provoke stress. The most common cause of anxiety is waiting for a bad test result.
If a person is taking any medications, the doctor should be informed.
If the diagnosis is confirmed, then the next person the patient is referred to is an oncologist. After the examination, therapy, diet and prognosis for recovery are prescribed.