Causes of occurrence Key signs of the disease Diagnosis and innovative detection methods Treatment of Burkitt's lymphoma in Israel Advantages of treating the disease in Israel Prognosis and rehabilitation
In medicine, under the term " Burkitt's lymphoma"
"mean a malignant tumor that can appear in almost any lymphatic tissue of the human body.
This formation has a pronounced tendency to rapidly spread beyond the lymphatic system, affecting neighboring organs and causing pain. Initially, the disease was diagnosed only in the countries of Oceania or Central Africa, but recently cases of Burkitt's lymphoma
have been recorded on the European continent.
Causes
Today, experts find it difficult to give a clear answer as to what exactly provokes the occurrence of lymphomas. However, the list of main factors influencing the appearance of malignant tumors includes:
- bad heredity;
- exposure to ionizing radiation;
- unfavorable environmental conditions;
- ingestion of chemical toxins or carcinogens into the body.
Additionally to the list of causes of Burkitt's lymphoma
certain infections can be included. For example, it has been scientifically established that 95% of African children suffering from the disease in question were initially diagnosed with the disease caused by the Epstein-Barr virus. It contributed to the development of fatal tumors, especially in those who suffered from immune deficiency or constant overwork.
Discussion
As noted earlier, due to the rarity of LB, the number of studies on the treatment of this disease is small, there are no randomized studies, and most of the presented studies included a small number of patients. The main international results of LB therapy are presented in Table. 8 [9-27]. These studies can be divided into 3 groups: non-intensive programs [5-14], intensive protocols (LMB, Hyper-CVAD, CODOX-M/IVAC, LMB, CALGB, NHL-BFM-83/86) without the inclusion of rituximab [13- 21] and intensive chemotherapy programs with rituximab [22–27]. As can be seen from the presented data, despite the intensification of therapy and the inclusion of rituximab in the protocols, OS and DFS did not change significantly.
Table 8. World data on LB treatment Note. n/a - no data.
The largest prospective study evaluating LB therapy in adults included 363 patients from 98 centers. Treatment was carried out according to the GMALL-B-ALL/NHL2002 protocol, which is a modified and improved version of the German group protocols B-NHL83, B-NHL86 and B-NHL90. The main features of the protocol were the inclusion of rituximab and a reduction in the dose of methotrexate to 1500 mg/m2 for patients aged 55 years or younger, to 500 mg/m2 for patients over 55 years of age. Remission was achieved in 88% of patients, 5-year OS was 80%. At the same time, in patients of the older age group (over 55 years of age), OS is significantly lower - 62% (compared to OS of patients aged 55 years or younger, which was 86%) [26]. T. Intermesoli et al. [24] conducted a study to evaluate the effectiveness of treatment of LB patients using a similar protocol GMALL-B-ALL/NHL2002. The study included 105 patients aged 17 to 78 years, median age was 47 years. 3-year OS and DFS were 67 and 75%, respectively. As can be seen, according to the results of our research group, the 5-year OS reaching 85% and the 5-year RFS reaching 95% are optimistic.
As in our study, in the work of D. Hoelzer et al. [26] showed that in the older age group there was a higher mortality rate compared to that in younger patients - 11 and 2%, respectively; Moreover, 90% of deaths are caused by infectious complications during the period of chemotherapy. Similar results are reported by T. Intermesoli et al. [24]: early treatment-related mortality was 13% and was observed predominantly in patients over 45 years of age with generalized stages of the disease (III-IV or Burkitt leukemia). In our study, treatment-related mortality was 8.6% (6 patients died), 3 patients were over 40 years of age. It is worth noting that the median age of our patients was slightly lower—31 years. J. Hong et al. [27] note that in addition to the high mortality rate in the group of older patients, it is precisely these patients who cannot be fully treated. In 25.6% of patients, the protocol program (R-Hyper-CVAD) is not followed due to its high toxicity.
J. Kelly et al. [28] analyzed data from the SEER database (Surveillance, Epidemiology and End Results) from 1973 to 2004, as well as publications according to PubMed, Web of Science, Cochrane Library from 1989 to 2007. The analysis included studies that included 10 patients or more with newly diagnosed HIV-negative LB. J. Kelly selected 13 publications (543 patients). Patients over 40 years old accounted for 42.2% ( n
=229). The OS of patients over 40 years of age in studies before 2000 was 40%, after 2000 - 60%, which is significantly lower than the OS of young patients.
Factors of unfavorable prognosis.
In a study by D. Hoelzer et al. [26] factors of unfavorable prognosis affecting OS (univariate analysis) were female gender, leukocyte levels >30·109/l, platelets <25·109/l, bone marrow lesions, involvement of the central nervous system, stages III-IV of the disease, LDH activity >250 U/L, high IPI and aaIPI. When conducting a multivariate analysis, statistically significant factors for unfavorable prognosis were age over 55 years, CM involvement, and female gender [26]. According to T. Intermesoli et al. [24], age over 60 years and ECOG score >1 point affect OS and DFS. In a study by J. Hong et al. [27], a multivariate analysis revealed that age over 60 years, ECOG somatic status score of 2 points or more, absolute lymphocyte count less than 1.2·109/l, high IPI are independent prognostic factors affecting survival. According to our data, CM, poor somatic status (ECOG score 3-4 points), Burkitt leukemia are factors of unfavorable prognosis that affect OS (according to multivariate analysis). Our results are fully consistent with the data of foreign authors.
Key signs of the disease
Externally Burkitt's lymphoma
represents single or multiple neoplasms that appear on the kidneys, ovary, peritoneal cavity, pancreas, intestines, and other vital organs.
The tumor quickly increases in size, affecting soft tissues or destroying bones, as a result of which the patient may experience difficulty breathing, dizziness, and increased body temperature. Further development of Burkitt's lymphoma
leads to compression of the spinal cord roots, permanent bone fractures or paralysis. Other important signs of this disease include:
- deformation of the nasal septum;
- swallowing dysfunction;
- intestinal obstruction or abdominal pain;
- the presence of neoplasms in the jaw area, etc.
Depending on the form of development of the disease, the symptoms of Burkitt's lymphoma
may be accompanied by a number of other painful sensations, if they occur, you should immediately consult a doctor.
Treatment
Malignant Burkitt lymphoma is highly sensitive to chemotherapy. In 80% of cases, intensive high-dose polychemotherapy provides long-term remission (https://cyberleninka.ru/article/n/limfoma-berkitta-klinika-diagnostika-lechenie/viewer). But relapses of LB are difficult to treat.
The main treatment method for LB is intensive PCT regimens. Additionally, symptomatic treatment is prescribed to correct electrolyte disturbances and eliminate other symptoms. In case of acute renal failure, hemodialysis sessions are performed daily.
Surgical treatment for Burkett's lymphoma is not advisable. It not only does not improve the condition, but also leads to loss of time and worsening prognosis due to prolonged rehabilitation after surgery and rapid re-growth of the tumor.
Surgical intervention is justified only in life-threatening conditions (gastrointestinal bleeding, organ perforation, intestinal obstruction
Diagnostics and innovative detection methods
In Israeli clinics, this disease is diagnosed based on several factors, the main ones of which are enlarged lymph nodes and structural changes in the epithelial composition of the affected areas. For examination, a tissue biopsy is performed on the patient under general or local anesthesia, after which the presence of malignant cells is detected. In addition, a number of studies are being conducted to help determine the stage of development of Burkitt lymphoma.
and the presence of other pathologies in the body.
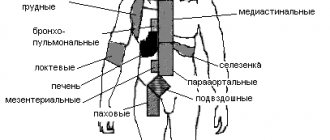
If enlarged lymph nodes cannot be detected by visual examination or by palpation, then a computed tomography scan is prescribed, which makes it possible to see hard-to-reach areas of the pelvis, abdominal cavity, and chest. The unique “St Jude/Murphy” system also helps to establish the stage of development of the disease, which displays the state of the patient’s immune system based on special studies.
Materials and methods
From 2003 to 2014 at the Federal State Budgetary Institution State Scientific Center M.Z. Russia, Federal Medical Research Center named after. P.A. Herzen, Medical Radiological Research Center named after. A.F. Tsyba, Orenburg Regional Clinical Hospital observed 70 patients diagnosed with LB: 45 men and 25 women aged from 15 to 62 years, median age 31 years. The stage of the disease was determined based on the S. Murphy classification. Stage I of the disease was diagnosed in 4 (5.7%) patients, stage II - in 9 (12.9%), stage III - in 25 (35.7%), stage IV - in 11 (15.7%), Burkitt's leukemia - in 21 (30%). In 23 (32.9%) patients, involvement of the BM in the tumor process was noted, in 15 (21.4%) - the central nervous system (neuroleukemia in 12, intratumor of the spinal cord in 3, intratumor of the brain in 3). B-symptoms were detected in 56 (80%) patients, increased lactate dehydrogenase (LDH) activity - in 50 (78.1%) out of 64, while 34 (56.2%) out of 64 showed an increase in LDH activity by more than 2 times compared to reference values. The median LDH level was 2398 (238–20,300) U/L. Acute renal failure (ARF) at the onset of the disease was determined in 17 (24.2%) patients, 8 chemotherapy (CT) was started against the background of therapy replacing renal function. Obstructive jaundice due to involvement of the head of the pancreas and bile ducts in the tumor process was detected in 3 patients. As the first stage of treatment, patients underwent drainage of the bile ducts (in 1 - endoscopic retrograde cholangiopancreatography, nasobiliary drainage, in 1 - minilaparotomy, transvesical drainage of the bile ducts, in 1 - laparotomy, intraoperative cholangiography, cholecystostomy). At the time of admission to the hematology clinic, 6 patients were diagnosed with gastric bleeding; in 1, in addition to gastric bleeding, multiple subdural hematomas and hemorrhages in the sclera were detected. Due to postrenal anuria caused by compression of the ureters by the pelvic tumor, nephrostomy was performed in 1 patient before admission to the clinic.
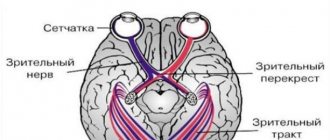
The diagnosis of LB was established in accordance with the 2008 WHO criteria based on a biopsy of the tumor, subsequent histological, immunohistochemical and cytogenetic studies. The patient examination protocol included a medical history and physical examination, a general blood test, a general urinalysis, a biochemical blood test, a coagulogram, a myelogram, an immunochemical study of blood serum and urine, computed tomography (CT) of the chest, abdominal and pelvic organs, an electrocardiogram, a biopsy lymph node - lymph node (tumor neoplasm), histological, immunohistochemical and cytogenetic studies, trepanobiopsy, lumbar puncture with cytological and biochemical studies of the cerebrospinal fluid. All patients were assessed for HIV status, the presence of HBsAg (qualitative test), and antibodies to the hepatitis C virus antigen. According to indications, fibrogastroduodenoscopy, colonoscopy with multiple biopsies of the mucous membranes of the stomach and intestines, CT scan of the soft tissues of the neck and brain, and magnetic resonance imaging of the brain were performed. brain, soft tissues of the neck, pelvis with intravenous bolus contrast, diagnostic laparoscopy or laparotomy with biopsy of the tumor formation. All women were consulted by a gynecologist; according to indications, ovarioprotection was prescribed for the period of chemotherapy. The immunohistochemical panel included antibodies to CD20, CD3, CD10, BCL2, BCL6, c-MYC, Ki-67, MUM1, cyclin D1, and in some cases, TdT. Cytogenetic studies were performed in 70 patients. A standard cytogenetic study (G-differential staining of chromosomes) was performed in 8 patients, tumor cells (LN) were examined in 4 cases, and BM cells in 4 cases. In 29 patients, a cytogenetic study was performed using fluorescent in situ
(FISH): in 9 cases, a suspension of tumor cells was used as a material, in 5 - a suspension of BM cells, in 13 - tumor prints (gastrobiopsy in 6, colon biopsy in 1, tonsil in 1, trephine biopsy in 1, lymph node in 4), in 2 — CM smears.
Histological sections of paraffin blocks were examined in 33 patients [5]. FISH study was carried out with DNA probes Vysis LSI IGH/MYC, CEP 8 Tri-color, Dual Fusion Translocation Probe (Abbott Molecular) to determine t (8;14)(q24;q32), Vysis LSI MYC Dual color, Break Apart Rearrangement Probe (Abbott Molecular) to detect rearrangement of the MYC
.
To exclude the presence of rearrangements of the BCL2
and
BCL6
genes, the Vysis LSI BCL2 Dual color, Break Apart Rearrangement Probe (Abbott Molecular) and Vysis LSI BCL6 (ABR) Dual color, Break Apart Rearrangement Probe (Abbott Molecular) probes were used, respectively.
Translocation t (8;14)(q24;q32) was detected in 56 of 63 cases, t (8;22)(q24;q11) - in 2 of 63 patients, variant translocations (presence of rearrangement of the MYC
in the absence of translocation t ( 8;14)(q24;q32)) - in 6 out of 63. In 7 cases, rearrangement of the
MYC
; FISH was not performed to detect t (8;14)(q24;q32).
In all cases, there were no rearrangements of the BCL2
and
BCL6
.
Treatment was carried out according to the LB-M-04±R protocol (4 consecutive blocks A-C-A-C) [4]. Since 2011, patients with CM lesions were treated with 6 blocks A-C-A-C-A-C with rituximab. Block A included intravenous administration of 10 mg/m2 dexamethasone on days 1–5, 1500 mg/m2 methotrexate over 12 hours on day 1, 800 mg/m2 ifosfamide on days 1–5, 1 mg/m2 vincristine on day 1, 50 mg/m2 doxorubicin on day 3, 150 mg/m2 cytarabine on days 4–5, and 100 mg/m2 etoposide on days 4–5; block C consisted of intravenous administration of 10 mg/m2 dexamethasone on days 1–5, 1500 mg/m2 methotrexate over 12 hours on day 1, 5 mg/m2 vinblastine on day 1, 2000 mg/m2 cytarabine 2 once a day on days 2-3, 150 mg/m2 etoposide on days 3-5. Rituximab was administered intravenously on day 0 of the course at a dose of 375 mg/m2. All patients received neuroleukemia prophylaxis on the 1st day of each block by intrathecal administration of 3 drugs: 30 mg of prednisolone, 30 mg of cytarabine and 15 mg of methotrexate. When neuroleukemia was detected, lumbar punctures with intrathecal administration of chemotherapy were performed 2 times a week until the cerebrospinal fluid was completely sanitized and 3 normal cerebrospinal fluid tests were obtained. As the disease progressed, the patient was removed from the protocol. In three patients with involvement of the tonsils, oropharynx and nasopharynx in the tumor process due to the threat of asphyxia, treatment was started in the intensive care unit with artificial pulmonary ventilation (ALV) [6].
29 (41%) patients had a history of surgical interventions related to the underlying disease (Table 1). The main goal of such interventions, usually carried out in general surgical hospitals, was to reduce the volume of the tumor mass or radical removal of an incidentally detected tumor. Urgent histological examination was not performed. Doctors and patients learned about the diagnosis of lymphoma after 10-14 days. During this period, in most cases, continued rapid tumor growth was observed.
Table 1. Surgical interventions in 29 patients with LB before the start of chemotherapy according to the LB-M-04 protocol
Complications of chemotherapy were assessed in accordance with CTCAE (Common Terminology Criteria for Adverse Events) 2009 [7].
Statistical data analysis.
When statistically analyzing the data using univariate and multivariate analyzes (Cox regression analysis), unfavorable prognostic factors associated with LB were discovered and assessed.
Overall survival (OS) was chosen as the main criterion for assessing unfavorable prognosis factors, and relapse-free survival (RFS) was chosen as an additional criterion. Along with the survival values, we present the standard error ( SE
), risk ratio (HR), and corresponding 95% confidence interval (CI).
The threshold level of statistical significance p
was chosen equal to 0.05. The licensed statistical package SAS 9.1 was used for calculations.
Treatment of Burkitt's lymphoma in Israel
Has proven itself in the process of getting rid of Burkitt's lymphoma
a method of chemotherapy that involves introducing various potent substances into the patient’s body that kill malignant cells.
One of these drugs was cyclophosphamide, administered intravenously in an amount of 30-40 mg/kg. The course of therapy, as a rule, includes 2-3 injections every 10-14 days (not more often).
Embiquin, also administered intravenously at 0.2-0.3 mg/kg/day, helps in the fight against Burkitt's lymphoma The course of treatment with the mentioned medication is no more than 5-6 days at the discretion of the attending physician.
In recent years, Israeli medical institutions have combined chemotherapy with antiviral drugs. The fact is that during treatment the patient’s body is exhausted and susceptible to all sorts of viral infections, which cause serious health complications and also slow down the rehabilitation process. For example, when taking cyclophosphamide and ganciclovir (sometimes foscarnet) in combination, the likelihood of various types of pathologies in the patient decreases.
An innovative way to combat the described disease, used in Israeli clinics, is the introduction of hematopoietic cells into the affected lesions. This method allows you to consolidate the effect achieved with chemotherapy and restore the functions of damaged organs in the shortest possible time.
100% accurate diagnosis is Ichilov’s calling card
Even before the patient arrives at the clinic, his examination program is carefully planned in order to obtain the necessary information about the characteristics of the disease in the shortest possible time and begin treatment on time. Typically the diagnostic process takes only three days.
First day
Immediately upon arrival at the clinic, the patient has a consultation with the attending physician, who conducts an examination, clarifies the symptoms that are troubling the patient, and studies the medical documentation provided by the patient. At the end of the consultation, the doctor decides which diagnostic procedures the patient will undergo in Ikhilov to confirm the diagnosis.
Second day
Typically, diagnosis of lymphoma in Israel is carried out using the following methods:
- CT scan. Using this method, the condition of the lymph nodes is checked.
- Blood analysis. The number of lymphocytes and deviations in other parameters are assessed.
- Positron emission tomography. This highly sensitive method can show the extent of the disease.
- Biopsy. Based on the test results, accurate conclusions can be drawn about the presence of lymphoma, as well as its type and size.
- Bone marrow puncture with cytogenetic analysis. Allows you to determine the condition of bone marrow tissue and identify the need for bone marrow transplantation.
- Gallium scintigraphy. The patient is injected with a gallium radioisotope and scanned with a gamma camera.
The third day
After receiving the results of the examination, a medical consultation gathers. On this day, doctors assess the overall prognosis and collectively choose the most promising treatment regimen.
Advantages of treating the disease in Israel
Today, Israeli medicine has made significant progress in the treatment of Burkitt's lymphoma.
High-tech equipment allows timely diagnosis and effective treatment of this disease at any stage of development. The list of key advantages of treatment in the mentioned country includes:
- quality care and spacious rooms;
- use of the latest drugs;
- 24-hour supervision by highly qualified doctors;
- the opportunity to consult with leading experts in their field.
When primary signs of Burkitt's lymphoma
You shouldn’t delay visiting a doctor, because the likelihood of recovery directly depends on how quickly a person seeks help.
Advantages of Top Ichilov
- The clinic’s oncologists and oncohematologists are first-class doctors and experts in the treatment of a variety of lymphomas. They have undergone many years of training and have exceptional experience.
- Diagnostic studies are carried out using the latest laboratory technology and high-precision equipment.
- Unique methods are used for treatment, ranging from highly effective chemotherapy regimens to the use of immune drugs.
- Patients of the clinic live in comfortable rooms, surrounded by an atmosphere of comfort, and a personal curator-translator is engaged in interaction with doctors and translation of medical documentation.
- 5
- 4
- 3
- 2
- 1
(12 votes, average: 4.4 out of 5)