Inappropriately elevated mood is a condition that is the exact opposite of depression. If it haunts a person for quite a long time and is accompanied by other inadequate or illogical manifestations, then it is considered a mental disorder. This condition is classified as manic and requires special treatment. Depending on the severity of symptoms, consultation with a psychotherapist or psychiatrist may be required.
At CELT you can get advice from a psychiatrist.
- Appointment with a psychiatrist with an extended interview, psychotherapy session - 4,700
Make an appointment
Features of the development of mania
In some cases, manic tendencies can be a personality trait, just like apathy tendencies. Increased activity, constant mental agitation, inadequately elevated mood, outbursts of anger or aggression - all these are symptoms of manic syndrome. This is the name given to a whole group of conditions that have different causes and sometimes different symptoms.
Both various life situations and incidents, as well as uncorrected pathological character traits, lead to the development of mania. A person prone to manic behavior is very often obsessed with an idea, he strives to realize it, even if it is unrealistic. Often the patient is driven by theories that have political, religious or scientific justifications. Quite often, patients show a tendency to be active in social and community activities.
A significant proportion of manic patients have so-called overvalued thoughts and ideas. Sometimes they can be global, sometimes these are ideas at the everyday level. From the outside, the behavior of patients talking about their ideas sometimes looks quite comical. If a highly valuable thought is global in nature, the patient, on the contrary, seems thoughtful and enthusiastic to others. Especially if he has enough education and erudition to substantiate his beliefs.
This condition is not always a pathology; it can be individual characteristics of the psyche. Treatment is necessary if overvalued thoughts and ideas get out of control and consume the patient’s entire life, in other words, interfere with the life of himself or those around him.
Treatment
Treatment for manic-depressive psychosis is gradual. First, the current exacerbation is stopped, normalizing the psychophysical state of the person. Next, maintenance and anti-relapse treatment regimens are individually prescribed.
A suicidal condition is an indication for emergency hospitalization. In some cases, electroconvulsive therapy (ECT) is justified to overcome drug resistance. ECT is relatively safe, as it is performed under anesthesia with the use of muscle relaxants, but there are a number of contraindications.
Medication
The choice of pharmaceuticals depends not only on the severity of symptoms. Relief from an acute condition is possible with the help of rationally prescribed drugs in adequate dosage. Often during treatment it is necessary to change medications, taking into account individual tolerance.
The following groups of pharmaceutical drugs can be used in the treatment of bipolar disorders:
- mood stabilizers - eliminate psychomotor agitation, normalize mood - Valproate, lithium preparations, benzodiazepines;
- neuroleptics - auxiliary drugs in the presence of severe psychotic symptoms, eliminate delusions and hallucinations;
- antidepressants from the group of selective serotonin reuptake inhibitors;
- combinations of psychotropic drugs in individually tolerable doses;
- symptomatic treatment of concomitant disorders.
Quickly bringing aggression and psychomotor agitation under control prevents the exacerbation episode from prolonging. The preventive effect of the drugs develops gradually, so maintenance therapy is prescribed for a long period. Timely relief of depression is necessary to prevent suicidal behavior.
Psychotherapy and rehabilitation
Pharmacotherapy is carried out against the background of psychosocial support. Rehabilitation measures significantly help in managing people with a depressive phase, reducing the frequency of relapse. Particular attention is paid to the following areas:
- increasing awareness of the patient and his caregivers about the nature of the disease, features of the course, methods of therapy and prognosis;
- formation of motivation to improve the quality of life;
- explaining the need to comply with the prescribed regimen;
- training to recognize early signs of developing relapse;
- methods of dealing with stress, exacerbation triggers, risk factors;
- psychotherapy – individual (cognitive-behavioral, rational), family, group (interpersonal).
A scheduled consultation with your doctor is a key point in treatment, so you need to openly discuss all issues with a specialist. The psychiatrist must regularly monitor not only the effectiveness of the measures taken, but also monitor changes in the person’s status. If necessary, the therapeutic course is modified.
When do you need a doctor's help?
Manic syndrome is already a deviation from the norm, which is characterized by a number of symptoms that are more unpleasant for others than for the patient himself. This disease manifests itself as disturbances in mental activity and the emotional sphere.
Usually the behavior of a manic patient is incomprehensible to others and looks at least strange.
There are certain symptoms that indicate the need for medical attention:
- Extremely elevated mood, up to constant mental excitement and euphoria.
- Optimism that does not correspond to the situation, the patient does not notice real problems and is not inclined to experience a bad mood appropriate to the situation.
- Accelerated speech, accelerated thinking, lack of concentration on objects and phenomena that do not interest the patient. Therefore, with mania, learning is often difficult, when you have to pay attention to rather boring things.
- Increased mobility, active gestures and exaggerated facial expressions.
- Extravagance, pathological generosity. The patient can spend all his savings in a minute, without realizing responsibility for his actions.
- Insufficient control over behavior. The patient does not realize that his high mood is not appropriate everywhere.
- Hypersexuality, often with promiscuity (for example, a person who has never been prone to cheating before suddenly begins to flirt “indiscriminately”, enters into close relationships that he would never have dared to enter into before, even to the point of starting several novels in parallel or starting into a series of “short, non-binding relationships”, which later, after the episode of mania has passed, he will repent and feel shame and even disgust, sincerely not understanding “how this could happen”).
Treatment is complicated by the fact that the patient himself often does not recognize himself as sick. He considers his condition to be normal, subjectively pleasant, and does not understand why others do not like his behavior: after all, he feels better than ever before. It is difficult to send such a patient to see a doctor and persuade him to undergo therapy.
Clinical picture of bipolar disorder
The symptoms of bipolar disorder are determined by the manifestations of the main phases - mania (hypomania), depression. The number of episodes is unpredictable, as is their severity. The duration of an exacerbation can range from several days to 1-2 years. Intermissions (“bright” interval with the absence of symptoms) with controlled treatment persist for 3-10 years or more.
Symptoms and signs of the manic phase
Manic syndrome varies in severity, from hypomania to severe psychotic disorders. The classical phase should include a triad of such signs: ideational-mental and motor arousal, elevated mood (hyperthymia). A “full” episode occurs in 5 stages, accompanied by a worsening of symptoms followed by calm.
Hypomania is the mildest degree, not accompanied by delusional-hallucinatory phenomena. The patient is unusually cheerful, active, and energetic. Increased social activity, hypersexuality, and shortened sleep duration are possible. People take extravagant actions, spend money thoughtlessly or, on the contrary, become aggressive. Thinking is accelerated, speech is confused, and attention is easily distracted.
Approximately 86% of patients with bipolar disorder experienced a severe manic phase. Delusional ideas of grandeur, hallucinations, and an influx of thoughts (mentism) cause social maladjustment. Mood changes should be clear, observed for at least 4-7 days (depending on the phase criteria according to ICD-10).
Symptoms and signs of the depressive phase
Depressive episodes usually last at least three times longer than manic episodes. The classic syndrome includes the following symptoms that should be observed for at least 2 weeks:
- Symptoms are worse in the morning.
- Decreased/absent habitual responses to events or activities that would normally resonate within the person.
- Interests are reduced. The patient ceases to enjoy individually pleasant phenomena, things, food.
- Appetite, body weight, and libido decrease.
- Psychomotor retardation confirmed by others.
- Fast fatiguability.
- Lack of self-confidence, decreased self-esteem.
- Slowing of mental activity, ineffective work capacity.
- Unreasonable feelings of guilt, self-judgment, thoughts of death, or suicidal behavior.
- Insomnia or drowsiness.
Mixed episodes consist of symptoms from both phases and can appear at any stage of the disease. Rapid cyclicity (10-15% of patients) is indicated by the development of at least 4 cases of exacerbation per year, accompanied by intermissions.
Patients usually remain in the depression phase most of their lives. Thus, patients with type G BD are on average 32% of the time in a state of depression and 9% in a state of mania/hypomania. Patients with type BD GG spend 50% of their time in the depression phase and only 1% in a state of hypomania. Depression is usually the first symptom of BD, especially in women. The risk of suicide during this phase is greatest.
Sturov N.V., Romanova O.L. Bipolar disorders: clinical picture and principles of therapy // Difficult Patient. 2008. No. 4.
Symptoms and signs of the disease
In addition to the signs listed above, there are several characteristic symptoms that unite almost all manic states:
- Tendency to thoughtlessly waste money.
- Tendency to make bad deals and gamble.
- Frequent violation of the law.
- Tendency to provoke fights and conflicts.
- Excessive alcohol consumption or addiction to other bad habits.
- Promiscuous sexual behavior.
- Pathological sociability - the patient often meets strange, suspicious individuals and spends time in a variety of companies.
If these signs get out of control, qualified medical attention is needed. It is important to understand that such behavior is not promiscuity, but symptoms of a disease that needs to be treated. Appealing to common sense is useless.
In some cases, the patient has a specific mania - for example, a mania of a special purpose. Then the patient is sincerely confident in his special mission and tries to implement it with all his might, despite the skepticism of others.
Diagnostics
The clinical picture plays a major role in making a diagnosis. Symptoms can only be assessed by a psychiatrist after a comprehensive life history collection. Laboratory and instrumental studies are of little significance. The criteria for bipolar disorder must correspond to those specified in the International Classification of Diseases (ICD-10), which are used in the protocols for providing assistance to the Russian Federation.
Mental status is examined not only at the time of examination, but throughout the entire history of the disease. The patient’s complaints, symptoms observed from others (by others), and the age of first manifestations are taken into account. Relatives must honestly talk about the peculiarities of raising children, the presence of hereditary burden of (any) mental illnesses, including through generations.
An important diagnostic point is assessing the risk of suicide. The most commonly used is the Columbia scale. Self-harmful behavior and preparatory actions are also included in the criteria for severe MDP.
Types of manic states
There are several classifications based on the manifestations of mania and their content.
Based on content, the following types are distinguished:
- Persecution mania is accompanied by paranoia. The patient is convinced that he is being persecuted; anyone can act as a persecutor - from relatives and friends to the intelligence services.
- Mania for a special purpose - the patient is sure that he needs to create a new religion, make a scientific discovery, save humanity.
- Delusions of grandeur are similar to the previous one. The main difference is that the patient does not have a goal, he simply considers himself the chosen one - the smartest, the most beautiful, the richest.
- Mania of guilt, politeness, self-destruction, nihilistic - rarer situations. Patients prone to alcohol abuse often experience mania of jealousy.
According to the emotional state, manic syndrome can be:
- Joyful mania is excitement, an unreasonably elevated mood.
- Angry – hot temper, tendency to create conflict situations.
- Paranoid – manifested by paranoia of persecution, paranoia of relationships.
- Oneiric – accompanied by hallucinations.
- Manic-depressive syndrome is characterized by alternating mania and depression.
With manic-depressive syndrome, intervals may alternate after an equal amount of time, or one type of behavior predominates. Sometimes the next phase may not occur for years.
TIR in children
In almost 60% of cases, the prerequisites or problems associated with manic-depressive psychosis arise in childhood/adolescence.
Early onset of the disease increases the risk of late diagnosis, progressive course, and severe psychosomatic disorders. Due to their age, young people are susceptible to emotional swings, suicide attempts, and exposure to psychoactive substances. Excessive study load, family quarrels, lack of education are the main provoking factors. According to the results of Swedish-American studies, bipolar disorder is 4 times more likely to occur in children with excellent grades. Teenagers compensate for stress with demonstrative behavior, running away from home, and aggression.
MDP occurs more often in children from single-parent or conflict families. At the same time, social status is unimportant, since gaps in education can exist at any level of income. Often manic-depressive psychosis is combined with eating disorders, dysmorphophobia, and overvalued interests.
Questions and answers
When is hospitalization required for a manic patient?
In case of severe mania, hospitalization will allow the patient to avoid actions aimed at himself and others. It will also help to identify the minimum maintenance doses of drugs to prevent another exacerbation. If a person, after stopping the attack, continues to follow the recommendations for taking medications, then the likelihood of developing the next phase will be minimal.
What is the best thing to do if a relative develops a manic stage and refuses treatment?
There are several options. One of them is calling a doctor at home and following his recommendations. The second is forced hospitalization if a person poses a threat to himself and others. Usually, after the symptoms subside, most patients agree to go to the doctor on their own, as their condition worsens, they feel weak and empty.
Causes of psychotic syndrome
The main etiological factors of the disease are:
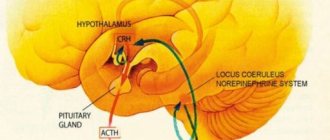
- endogenous: hereditary predisposition associated with congenital, genetically predetermined disorders of the functioning of individual brain structures, transmission of nerve impulses, information processing, accumulation and use of experienced experience;
- psychogenic: severe stress in one way or another affects the psycho-emotional state of any person;
- organic, associated with diseases of the central nervous system.
But as a rule, it is impossible to single out any one cause of psychomanic personality disorder, so experts are convinced of the polyetiological nature of the disease. Genetic predisposition only increases the risk of developing the disease, but trigger factors may include:
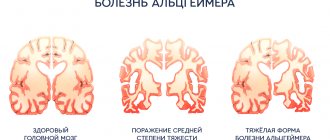
- neoplasms in the brain: aneurysms, hematomas, cysts, tumors;
- complications after brain surgery, ischemic or hemorrhagic stroke;
- acute or chronic intoxication with drugs, alcohol and other poisons;
- suffered a severe infection with neurological complications (meningitis, encephalitis, etc.) or other hidden chronic pathologies (for example, syphilis, HIV);
- complicated pregnancy and childbirth: acute fetal hypoxia, placental insufficiency, defects in the development of the central nervous system under the influence of teratogenic factors, etc.;
- a stressful situation that is painful for a person.
As practice shows, perfectionists, people who strive to completely control all areas of not only their lives, but also those around them, are predisposed to the development of manic personality disorder. They are confident and ready to prove that they are right; they are offended when people try to argue with them or do not follow their advice.
When psychotherapists ask patients about their childhood, they often talk about problematic relationships with parents, total control on their part, punishment for the slightest offenses, lack of interest in the problems and inner world of the child.
As for the pathogenetic mechanism of development of manic personality disorder, most experts adhere to the biochemical theory. The initial link in pathogenesis is a violation of the production, metabolism and sensitivity of central nervous system cells to the action of catecholamines (dopamine, adrenaline, norepinephrine) and endorphins (in particular, serotonin).
Such changes “trigger” a whole cascade of biochemical reactions that lead to disruption of hormonal levels and electrolyte balance. This predetermines an inadequate emotional reaction to certain events.
Differences between males and females
If you believe the statistics, men get sick less often than women. Ratio: 3:2. The female part of the patients is characterized by a rapidly cyclical nature of the disorder. Women have low sensitivity to therapeutic methods. They have a higher risk of suicidal behavior and a higher rate of hospitalization. The symptoms of bipolar disorder in men are practically no different from the manifestations of the disorder in women.
Minor differences - in the male part of the patients the phases of mania and hypomania predominate, and in the female part - depressive states. Symptoms of depression in women are much more pronounced.
How is hypomania treated?
Not all hypomanic conditions require treatment. In some cases, isolation from external stimuli and proper sleep can restore normalcy. The following therapeutic measures are used to treat hypomania:
- Physiotherapy.
- Pharmacotherapy (motor stabilizers, neurometabolic therapy, antipsychotics).
- Diet therapy.
- Biofeedback therapy.
Treatment of a manic state is possible in a hospital
, and at home.
The hypomanic state may itself end with a return to normal mood. In some cases, hypomania develops into a more severe painful disorder - a manic state.